Perspective - Interventional Cardiology (2013) Volume 5, Issue 3
Transradial approach for percutaneous coronary interventions: the future is now
- Corresponding Author:
- Giovanni Amoroso
Onze Lieve Vrouwe Gasthuis, Amsterdam, The Netherlands
Tel: +31 205 994 831
E-mail: g.amoroso@olvg.nl
Abstract
Keywords
percutaneous coronary intervention;same-day discharge;transradial.
Introduction
Percutaneous coronary interventions (PCIs) have been traditionally performed through the femoral artery, which is easy to puncture and large enough to accommodate catheters and devices. Bleeding access-site complications, from hematomas to retroperitoneal bleeding, take place in a quite consistent proportion of patients: between 3 and 5% in normal conditions, up to 10% in high-risk subsets. Access-site complications can result, in the most severe cases, in permanent invalidity or death, and in the less severe ones, patients will still need blood transfusions and/or surgical repair. In any case, access-site complications will always prolong hospitalization, with an increase in direct and indirect costs related to PCI. Access-site complications will be more frequent in cases of multiple antiplatelet therapy, and/or anticoagulation, such as in patients with acute coronary syndromes, chronic atrial fibrillation, prosthetic valves and peripheral arterial disease. Access-site complications will also be more frequent in obese, old and female patients [1]. The miniaturization of catheters and equipment, and the use of access closure devices, have only reduced their incidence, but not completely solved the problem [2].
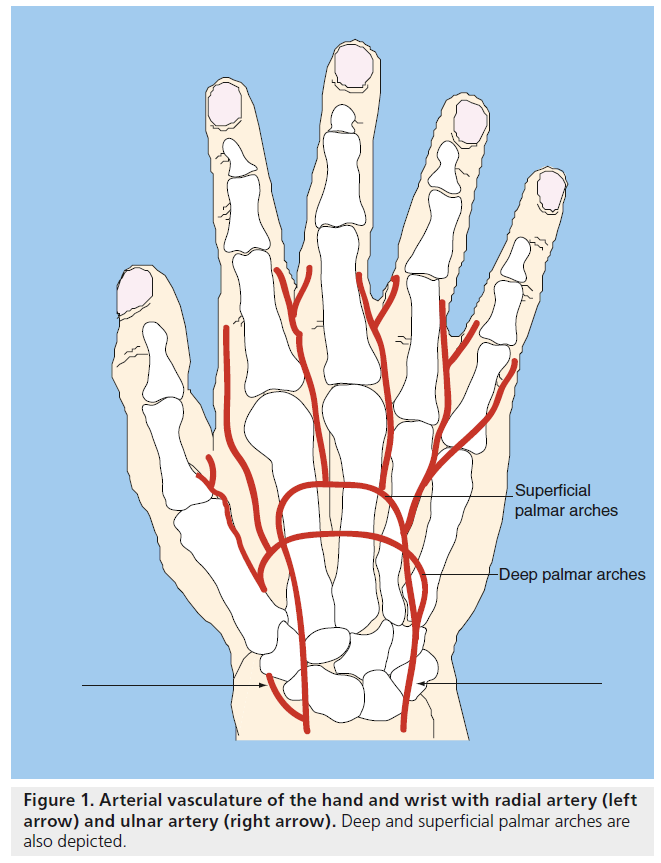
The use of an alternative access, which would be less susceptible to complications, seemed to Kiemeneij and his colleagues the most natural way to bypass this problem [3], as he prepared himself to successfully attempt the first PCI procedure worldwide through the radial artery at Onze Lieve Vrouwe Gasthuis (OLVG; Amsterdam, The Netherlands) 20 years ago. The expected advantages of the radial artery were the following: to be very superficial, thus easy to locate and puncture, but also to compress against the bone structures behind it; no major nerves or veins were located near the artery, minimizing the risk of injury of these structures; and the full dual blood supply (radial and ulnar artery) of the hand, with complete anastomosis by means of the superficial and deep palmar arch: significant ischemic complications in case of radial artery occlusion would, therefore, be very rare (Figure 1). The validity of this intuition was confirmed by the first randomized study (ACCESS), where the transradial approach (TRA) was shown to be superior, in terms of access-site complications, both to the transfemoral and to the transbrachial approaches (0 vs 2.0 and 2.3%, respectively) [4].
Clinical advantages of TRA
Until recently, the problem of bleeding complications during and after PCI procedures had been underestimated as most efforts aimed to reduce ischemic complications. As a matter of fact, the outcomes of PCI patients, particularly in the course of acute coronary syndromes, are also significantly influenced by the occurrence of bleeding complications, not only at nonaccess sites (5.5-fold increase in mortality at 1 year), but also at vascular access sites (2.5-fold increase in mortality at 1 year) [5].
Currently, it is well established that TRA nearly abolishes access-site complications in all patients undergoing a PCI. The superficial course of the distal radial artery allows easy compression (manually or via a device) of the artery. All studies comparing TRA versus transfemoral access have demonstrated, on average, a tenfold reduction in major bleeding with TRA, both in the elective and the acute setting [6,7]. When access-site complications still occur after TRA, they usually have a benign course and do not influence the prognosis of patients.
For this reason, in high-risk subsets of patients, such as those suffering from an acute myocardial infarction, patients with chronic kidney disease and the elderly, this translates to clear clinical advantages, being TRA associated with a significant reduction in morbidity and fatal complications.
The RIVAL study showed, for instance, that TRA is associated not only with a lower rate of local vascular complications in the overall population, but also with a reduction in mortality in the setting of acute PCI [8]. These results have been confirmed in another randomized study (the RIFLE-STEACS study), in which a relative reduction in access-site complications and in mortality of nearly 40% was found by ST-segment elevation myocardial infarction patients in cases of TRA (vs transfemoral approach) [9]. At OLVG, TRA is systematically performed (>90% of the cases), both in the elective setting, as in the case of primary PCI, with a high rate of procedural success and without any delay in coronary reperfusion [10]. The reason why the clinical benefit of TRA becomes more evident in acute and/or high-risk patients lies most probably in the fact that these patients are more fragile and vulnerable to the sequelae of bleeding complications: hemorrhages will, in these patients, precipitate faster to hypovolemic shock; the use of blood transfusion and the discontinuation of antiplatelet therapies will promote stent thrombosis. Both these measures are simply not required in the case of TRA, even when some complications do occur. The net clinical advantage of TRA is further consolidated by the absence of other TRA-related serious complications: recent studies proved for instance no excess of radiation exposure [11] or neurologic complications [12] in the case of TRA procedures.
Nonclinical advantages of TRA
In elective patients, abolishing access-site complications will also translate in additional advantages, not strictly related to the clinical sphere but yet of the same importance.
Following femoral-access procedures, a period of bed rest in supine position is required to avoid complications at the puncture site. This may be poorly tolerated by patients with back and/or hip pain, chronic lung disease or heart failure. On the other hand, patients are able to move immediately after TRA. For that reason, TRA improves comfort, satisfaction and compliance of the patients to medical treatment. The quality of life, in terms of bodily pain, limitation in movements and daily activities, is substantially better in the case of TRA, both in the first 24 h and after 1 week [13]. The hospital stay seems better tolerated, since patients are not confined in bed, they can rely on themselves for going to the toilet or having a meal, they will experience fewer complications and they can go home earlier, to their personal environment and working activities. The psychological impact of the hospital admission seems also to be reduced, particularly in the case of culturally-related or age-dependent taboos, due to a preserved body intimacy and a reduced feeling of dependency. For the same reasons, nurse workload during and after PCI is significantly reduced in the case of TRA [14].
Since vascular access-site complications are rare after TRA, and coronary-related complications occur either in the first 4–6 h or during the subsequent days after an uneventful elective PCI, it is now accepted that many PCI procedures can be performed on an outpatient basis. In a seminal study, we demonstrated that, after a careful triage before and after the procedure, three out of five patients undergoing elective coronary stenting could be safely discharged home, 4–6 h after the procedure [15]. The safety and feasibility of a same-day discharge policy has later been confirmed in a randomized trial (EASY) [16] and, more recently, by many more experiences worldwide [17].
For patients, same-day discharge means a faster access to treatment and return to daily life/activities/work. Most patients will prefer same-day discharge to overnight stay in the hospital, provided that they will receive complete information regarding the risks and the advantages, that they are aware of the existence of a safety network in case of problems, and that they can count on adequate care and support at home. Second, but no less important, is that same-day discharge will result in less hospital-related, procedure- independent complications (e.g., infections, injuries and psychological distress). The safety and feasibility of same-day discharge after TRA PCI has been already acknowledged by many professional regulatory boards, and special reimbursement rates have been agreed between many insurance companies and hospitals [18]. Therefore, the legal and financial issues against same-day discharge, based on the fear for suing procedures and/or reimbursement litigations, are coming to an end. Same-day discharge leads to more efficient logistics (more patients treated in less time, by less personnel and with less hospital beds) and, therefore, to significant cost savings with a gain starting from €250 per patient, in the traditional hospital settings, but able to exceed thousands of Euros per patient, in cases where the departments of interventional cardiology and the protocols for admission and postcare are rethought upon the TRA concept [19].
TRA in (our) daily practice
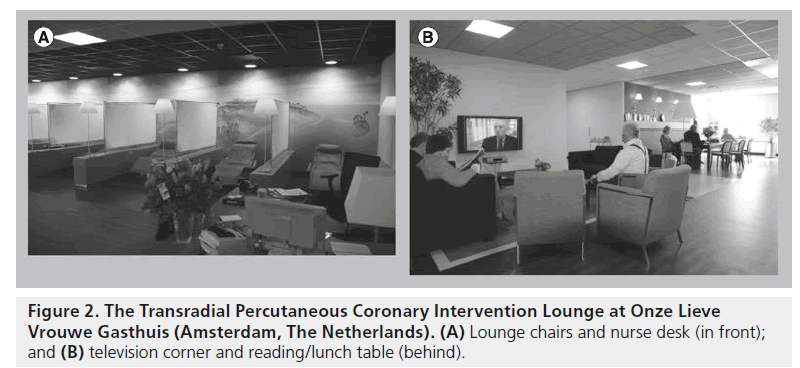
At OLVG, the whole PCI department was rebuilt in 2005 (so-called ‘Transradial PCI Lounge’), and all the pre- and post-care protocols have been fine-tuned, in order to obtain the best advantages out of TRA. The Transradial PCI Lounge does not have rooms and beds, such as in a traditional hospital environment, but is equipped with lounge chairs, a plasma TV screen, reading and personal computer corners, similar to ‘business class’ lounges in airports ( Figure 2A & 2B). People can wait to be treated in the company of relatives or friends, and recover after the procedure under the surveillance of trained nurses. Their hospital stay will be more relaxed (‘healing’ environment), and when they go home soon after, only the bandage on their wrist will betray the fact that they have undergone a PCI procedure [20]. On the other hand, the hospital beds in the other wings of our department and of the coronary care unit, will be occupied by acute patients and/or patients requiring additional care (complex procedures, periprocedural complications).
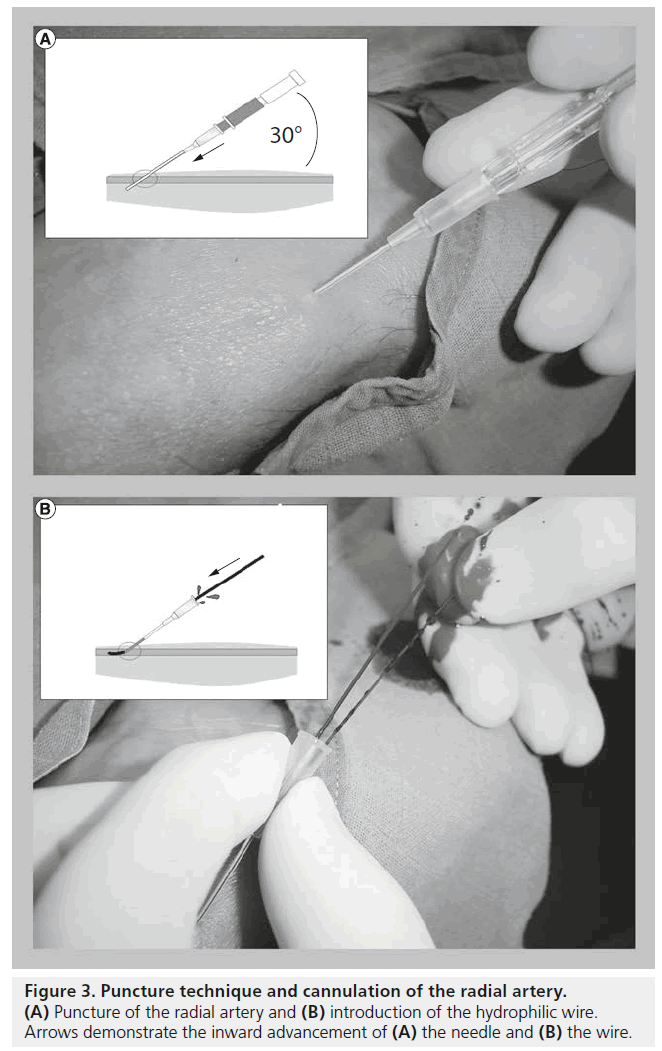
To improve comfort and further speed up turnover, patients are only partly undressed (the chest and the arms) during the procedure, and only the wrist is prepped for arterial access. After administration of local anesthesia (lidocaine 5% subcutaneous, 1–2 ml), the puncture of the radial artery is performed 1–2 cm above the styloid process, with an angle of approximately 30° onto the skin surface, by means of a 21 gauge needle-cannula system. The artery is gently transfixed, then the needle is removed, and the cannula is slowly pulled back until good back flow is achieved. At that point a 0.025 inch hydrophilic wire is inserted, on which the arterial sheath is later introduced (Figure 3A & 3B). Since the radial artery is small and susceptible to spasm, particular care is devoted to achieving cannulation on the first or after very few attempts.
After the procedure, the introducer is removed immediately at the catheterization laboratory and hemostasis is maintained for at least 2 h by means of an inflatable wrist band. Patients (except for the more fragile and old) are not confined to rest and are allowed to walk. In case of an uneventful procedure and no post-PCI complications, patients are allowed to go home on the same day. Intensive load (e.g., driving and pulling weights) of the punctured arm for the following 24 h after the procedure is discouraged.
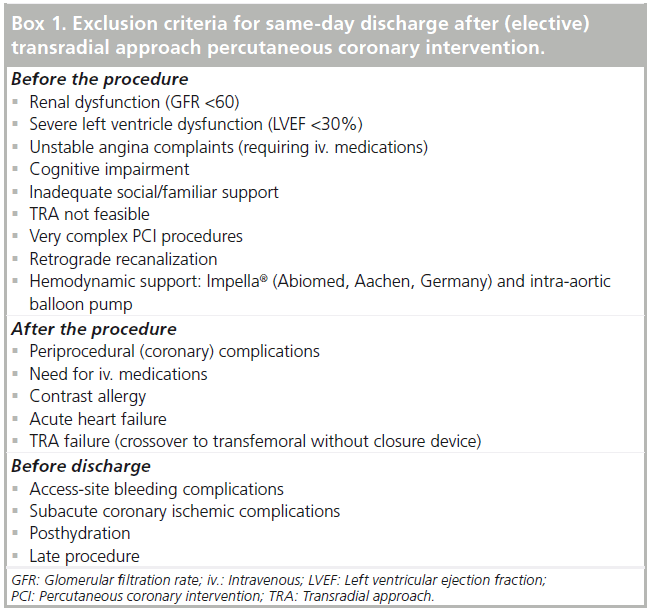
The key for success and safety of a same-day discharge program lies, in our opinion, in three issues: a multistep triage of patients (before admission, after the procedure and before discharge); dedicated staff at the TRA Lounge; patient’s education and social support (Box 1). An unpublished survey of our data since the opening of the Transradial PCI Lounge revealed to us that, among the many thousand/years of patients undergoing a PCI at our hospital every year, approximately four out of ten patients are excluded from a same-day discharge before the procedure owing to acute clinical presentation, clinical frailty and/or anticipated procedural complexity; of the remaining patients, approximately one out of six will experience either a peri- or a post-procedural complication and, therefore, will stay overnight for further treatment and care. Among the patients uneventfully discharged home on the same day of the procedure, approximately 3% will seek medical contact (mostly because of bruising in the arm or atypical chest pain) within the next 48 h, but almost none will be readmitted with severe adverse events.
Worldwide adoption of TRA
For many years after its first attempt, TRA has been considered with a mix of curiosity and scepticism. The lack of hard evidence in favor of TRA, and its alleged technical complexity, has left TRA confined for many years in locally or geographically-isolated contexts (particularly in France, Japan, Canada and India). Suddenly, and in some ways quite unexpectedly, the fire of TRA has started to widely burst out, even in the USA, which were traditionally faithful to the transfemoral approach [21]. Over the last few years, the technological advances in coronary devices have also improved the outcomes and broadened the indications of PCI, but also led to a dramatic increase in the number of PCI procedures performed per year. Coronary artery disease is nowadays also better and more often diagnosed both in western and nonwestern countries [22]. Thus, the reason for this mindset toward TRA is probably not only due to raising the awareness of its clinical advantages, thanks to the recent publication of robust scientific and clinical data, but also the increasing pressure on caregivers to provide more care at a lower cost.
By reducing the incidence of serious access-site complications and simplifying logistics around PCI procedures, TRA offers an appealing solution to the need for more (and affordable) care for coronary patients. Not surprisingly, regulatory bodies have started to acknowledge the advantages of TRA: for instance, the European Society of Cardiology has recently proposed TRA as the preferred vascular access for PCI [23]. Scientific and professional associations are also strongly encouraging TRA education and promoting its use by means of hands-on workshops, courses and E-education [101]. As a result, TRA is rapidly being adapted into clinical practice around the globe; in a recently published survey among PCI centers worldwide, more than 30% of the respondents declared they perform TRA in all their patients, and more than 60% in at least half of patients [24]. The TRA issue is nowadays no longer confined to the medical world but has reached the popular audience and mass-media: television shows, newspapers, patients’ blogs and internet websites, and even smartphone apps are scrupulously covering this issue [102]. Before, as we soon expect, TRA is acknowledged as the standard-of-care for PCI procedures, some issues will need to be addressed: the learning curve of operators and personnel being the first; and the preservation of radial artery patency being the latter.
The issue of the learning curve
Interventional cardiologists may understandably be reluctant to abandon a technique in which they acquired proficiency, such as the transfemoral approach. Moreover, a learning curve for TRA is necessary, since, as for many other invasive maneuver, complications are lowest when procedures are performed by experienced TRA operators and at high-volume radial centers. When compared with the transfemoral access, TRA presents the following technical disadvantages: the artery is of smaller caliber (1.8–2.5 mm); the arm presents more anatomical abnormalities than the groin (i.e., both anatomical variations of the radial artery itself and of the brachiocephalic artery, and/or tortuosities and loops) [25]; the radial artery is naturally susceptible to spasm. As a result, TRA will require dedicated materials (e.g., needles and catheters), and special maneuvers and care (e.g., proper puncture and catheters manipulation, the administration of specific medications; Table 1). Operators will need to take into account a longer learning curve than for transfemoral approach. The operator’s failure will begin at approximately 10%, with a need to cross over to another approach, but soon drop to less than 3% after the first 500 cases performed [26]. After thousands of TRA procedures have been performed, the rate of procedural failure will stabilize at less than 1%, thus making TRA, in the hands of experienced operators, as successful as the transfemoral access.
| Problem | Cause(s) | Solution(s) |
|---|---|---|
| Difficult cannulation | ||
| Arterial puncture failure | Radial occlusion | Locate arterial course. Fixate artery with fingers. Repuncture more proximally |
| Artery small/calcified | ||
| Difficult sheath insertion | Skin resistance | Incise skin. Use smaller diameter (5 Fr). Use hydrophilic sheaths |
| Small radial | ||
| Difficult wire/catheter advancement | ||
| Forearm/elbow | Loop/anatomic variation | Angiography of the forearm. Use hydrophilic wire under fluoroscopy. External |
| manipulation of the arm | ||
| Shoulder/aorta | Tortuous aortic arch | Deep breath. Hydrophilic wire. Begin with JR than exchange over long wire |
| Calcifications | ||
| Poor catheter support | ||
| Into coronary arterial ostia | Aortic curve/diameter | Deep seating (5 Fr). Multiple guidewires. Change to dedicated curve |
| Into bypass venous grafts | High anastomosis | Puncture left radial |
| Miscellaneous | ||
| Radial spasm | Prolonged manipulation | Vasoactive medications through the sheath. Nifedipine sublingual. Smaller |
| Small radial artery | catheter | |
| Forearm hematoma | Side-branch perforation | Bandage forearm. Pressure cuff elbow |
| JR: Judkins right. | ||
Table 1. Problems, causes and possible solutions in the case of transradial approach.
The training and learning process involves not only the proper arterial cannulation, but also negotiation through the upper extremity into the ascending aorta with wires and catheters, and manipulation into the coronary arteries. Based on our experience, we would suggest to interventional cardiologists willing to learn TRA: to begin with simple procedures (elective, single-vessel, type A lesions) in patients with a good radial artery (males, less than 60 years old and normal build), in order to learn the skills of proper puncture; to proceed to more challenging radial arteries (old, women and weak pulsation),in order to acquire the skills in catheters advancement and manipulation, but still in technically simple PCI procedures; and to finally approach complex cases, such as multivessel procedures, chronic total occlusions and primary PCI. Practice will, in any case, make perfect, which means that operators willing to switch to TRA should be able to perform enough TRA cases per year, in order to improve their proficiency and keep their skills. In order to maintain the necessary skills, the European Society of Cardiology’s consensus document recommends performing 80 TRA procedures/year at least after the learning curve, and to perform at least 50% of their cases through TRA [23]. If this would not be possible, operators should reconsider their decision and be content with the transfemoral approach: a higher incidence of procedural failures and complications is, in fact, the consequence of being a low-volume operator, or confining the TRA to a second-choice approach.
PCI is a good example of teamwork, where outcomes are driven by proper selection of patients, proficient interventions and adequate postcare. The role of other medics and paramedics, both at the catheterization laboratory and at the ward, should not be underestimated. In order to prevent medical mistakes, particularly in the postcare, it is fundamental for operators to achieve a consistent agreement on indications (and exclusions) for the use of TRA, but also to adequately train personnel and to define pre- and post-care protocols, with regard to, for instance, concomitant medications, access-site preparation and surveillance of access-site complications, which will all contribute to a successful result.
Preservation of the radial artery’s patency
To preserve the patency of as many radial arteries as possible will be the second challenge in the case of a global ‘transradialization’ of the PCI world. Radial artery occlusion (RAO) is caused by an acute thrombotic formation at the site of arterial puncture, which will later evolve into a fibrotic occlusion of the blood vessel up to the nearest bifurcation (often at elbow level). RAO occurs, in most cases, without any symptoms, given the full dual blood supply of the hand by both the radial and the ulnar artery, converging in both the deep and superficial palmar arches [27]. Moreover, the arm and hand circulation are able to develop collaterals over time in case of RAO. For both these reasons, studies reporting rates of RAO in approximately 5% of patients following TRA PCI probably underestimate its real incidence [28]. Even when asymptomatic, RAO will, however, preclude reintervention through the same route, and therefore significantly undermine TRA programs. The occurrence of RAO is determined by one or more of the following three factors, all of them operatordependent and therefore preventable: incomplete anticoagulation, catheter–artery mismatch and prolonged arterial compression (Figure 4).
The use of heparin intravenously (5000 UI) or into the radial artery (via the introducer) is probably the best way to help prevent RAO. On the other hand, when heparin is not given or is given at a reduced dose, the incidence of RAO can exceed 20% of the cases. New anticoagulants (such as the direct thrombin inhibitor, bivalirudin) have also shown a similar protective effect against RAO [29]. The administration of a spasmolytic cocktail (usually nitrates and/or calcium antagonists) will also reduce the incidence and severity of spasm, which is a predictor of late RAO [30].
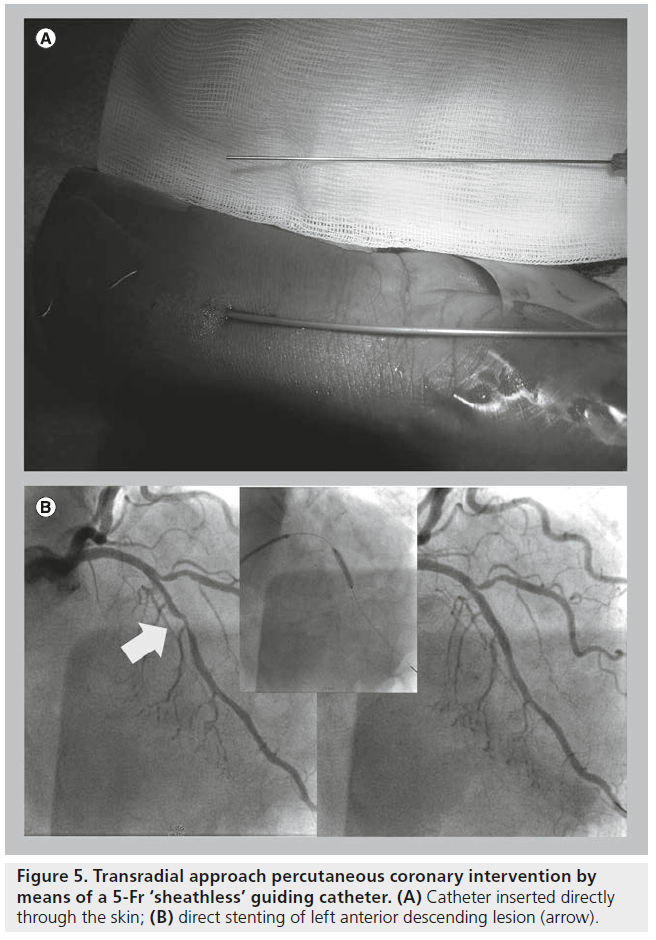
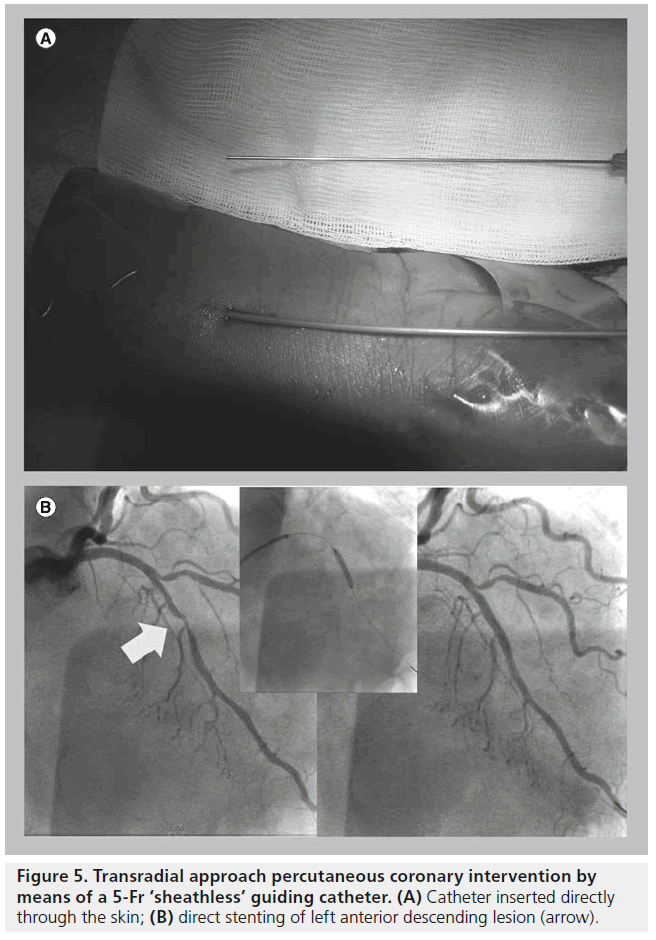
When seeking arterial access for PCI procedures, the current standard combination is a 6 Fr catheter and a 6 Fr compatible introducer. However, many patients will have a radial artery inner diameter smaller than, or equal to, the outer diameter of a 6 Fr compatible introducer: this catheter/radial artery mismatch will affect approximately one of each five male patients and nearly half of the female patients [31]. Female gender, Asian ethnicity, older age and diabetes mellitus seem to predict the occurrence of smaller radial arteries. Catheter–artery mismatch can be prevented by ‘downsizing’, which means the use of smaller catheters and sheaths. A 4- or 5-Fr-guiding catheter (plus introducer) belongs, therefore, to the downsized catheter. The use of so-called ‘sheathless’ catheters also fall into the ‘downsizing’ strategy. This kind of catheters, in fact, can be used without an introducer, which is usually 1–2 Fr sizes bigger in (outer) diameter than the corresponding catheter. Therefore, by using sheathless catheters it will be possible to downsize selectively at the radial artery level, while maintaining the standard diameter (and performance) at the coronary side, in a kind of virtual telescopic effect. For this reason, a sheathless 5 Fr PCI procedure is usually called a virtual 3 Fr procedure.
The use of smaller catheters (4 or 5 Fr), as well as sheathless ones – and ideally the combination of both – reduces the risk and/or extent of trauma to the radial artery, particularly in patients who have a small radial artery, thereby not only reducing patient discomfort, but also leading to fewer bleeding complications and occlusions of the radial artery (Figure 5A & 5B) [32]. By downsizing the inner lumen of the guiding catheters, it is also possible to reduce the amount of contrast agent used: this has a positive effect on safety, as it lowers the risk of contrast-induced nephropathy, a frequent (~15% of the cases) cause of hospital-acquired acute or chronic renal insufficiency after PCI procedures, leading in terms to a substantial increase in in-hospital mortality [33].
The use of downsized catheters still encounters the resistance of many interventional cardiologists, who are afraid of the unavailability of compatible devices. Indeed balloons, filters, wires and stents had been originally projected for being compatible with the standard 6 Fr catheters. At the time of the first TRA PCI 20 years ago, the use of 6 Fr catheters was considered an ‘extreme’ form of ‘downsizing’. Nowadays, as catheters and devices evolve, most of the devices available are already 5 Fr compatible. As a matter of fact, a systematic downsizing strategy could be adopted in many more patients than operators usually believe (up to 80% of most PCI population, even in all-comers studies, would be in fact feasible for a 5-F PCI) [34]. To obviate the problem of bad visualization of the coronary tree, which is another reason for some operators to dislike smaller catheters, automated contrast injectors, such as the ACIST CVi® (ACIST Europe BV, Maastricht, The Netherlands) contrast delivery system have been developed. Such advanced contrast injectors help overcome the limitations of delivering contrast with a hand syringe and a patient manifold through a small catheter [35]. At OLVG, where all catheterization laboratories are equipped with automated contrast injectors, two out of ten PCI procedures are performed either with a conventional 5-F catheter, or a sheathless one. At present, the use of bifurcation stents, chronic total occlusion devices, optical coherence tomography or aspiration catheters still represent a limitation for the use of downsized guiding catheters. In Japan, cardiologists and device companies devoted to the downsizing philosophy, have gathered into the ‘Slender Club’, with the specific aim of developing devices and techniques that can all be compatible not only with 5 Fr, but even with 4 Fr or smaller guiding catheters [36]. Hopefully these developments will soon be available in Europe, as well in the USA, so that there will be no limitation for a downsized strategy.
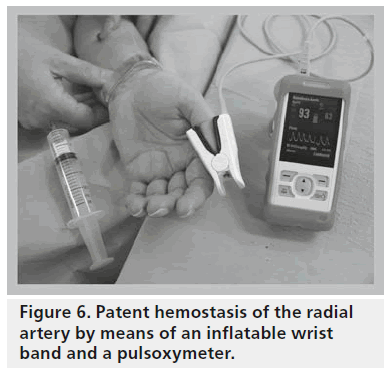
The small caliber of the radial artery, and the fact that it can be easily compressed against the styloid process has, unfortunately, an important drawback. Occlusive and prolonged compression of the radial artery during hemostasis result, in most of the cases, in a permanent, albeit asymptomatic, radial occlusion. So-called ‘patent’ or nonocclusive hemostasis – that is, applying enough pressure to the radial access site by means of an inflatable wrist band to achieve hemostasis and yet maintaining antegrade flow in the radial artery – has been shown to drastically reduce (to less than 1%) the incidence of radial occlusion (Figure 6) [37]. Successful and safe radial hemostasis may also be achieved by a very short application of procoagulant pads [38].
Figure 6: Patent hemostasis of the radial artery by means of an inflatable wrist band and a pulsoxymeter.
Conclusion & future perspective
A total of 20 years after it was attempted for the first time, it is now clear that TRA offers clear advantages upon other arterial accesses when performing PCI. TRA dramatically reduces accesssite complications and, in the case of high-risk patients and procedures, is associated with a reduction in morbidity and mortality. TRA simplifies the logistics around PCI, since patients are not subject to bed immobilization during their hospital stay, and nurse workload is, therefore, significantly reduced. Patients undergoing TRA can, in most cases, be safely discharged home the same day of the procedure. For all these reasons, TRA seems the perfect solution to offer better care to more patients at a lesser cost, which is the most challenging and actual dilemma of contemporary hospital care.
In the near future, we expect TRA to become the preferred arterial access worldwide and, therefore, that the logistics around PCI will undergo a significant reshuffling toward sameday treatment and discharge. Interventional procedures will not only be safer and more comfortable, but will also be offered to more patients at a lesser cost. On the other hand, there will be a strong need for dedicated training and accurate selection of interventional cardiologists, as the success of TRA requires practice and expertise. These should be seen as an opportunity, rather than a limitation of TRA, to set new and higher standards in patient care. Medical institutions and operators, who already have experience with TRA, bear the responsibility to share their expertise and collaborate with starting centers and physicians during their training process. As the number of TRA procedures increases, the issue of preserving radial patency, by careful postcare of the arterial access and adoption of downsized, more radial-friendly devices, will be in the future, by far, the most urgent.
Financial & competing interests disclosure
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Background
▪ The rational for transradial approach (TRA) has been to reduce the incidence of access-site complications after percutaneous coronary interventions (PCI).
Clinical advantages of TRA
▪ TRA reduces bleeding complications in all cases, and is associated with a reduction in mortality in case of primary PCI (for acute myocardial infarction).
Nonclinical advantages of TRA
▪ TRA also improves the patient’s comfort, reduces nurse workload, allows same-day discharge and is cost effective.
TRA in (our) daily practice
▪ At Onze Lieve Vrouwe Gasthuis (Amsterdam, The Netherlands) most procedures are undertaken through TRA and on a same-day discharge basis.
▪ Patients are carefully screened before and after the PCI and stay at a dedicated lounge.
Worldwide adoption of TRA
▪ TRA is penetrating in clinical practice worldwide and TRA coverage on scientific and mass media is rapidly increasing.
The issue of the learning curve
▪ To avoid pitfalls of TRA, a learning curve is necessary.
Preservation of the radial artery’s patency
▪ Radial artery patency after the PCI can be maintained by downsizing and patent hemostasis.
Conclusion & future perspective
▪ TRA is quickly becoming the preferred arterial access for PCI and, therefore, good transradial training programs are necessary.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Waksman R, King SB 3rd, Douglas JS et al. Predictors of groin complications after balloon and new-device coronary intervention. Am. J. Cardiol. 75(14), 886–889 (1995).
- Mann T, Cowper PA, Peterson ED et al. Transradial coronary stenting: comparison with femoral access closed with an arterial suture device. Catheter Cardiovasc. Interv.49(2), 150–156 (2000).
- Kiemeneij F, Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Cathet. Cardiovasc. Diagn.30(2), 173–178 (1993).
- Kiemeneij F, Laarman GJ, Odekerken D et al. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the ACCESS study. J. Am. Coll. Cardiol.29(6), 1269–1275 (1997).
- Verheugt FW, Steinhubl SR, Hamon M et al. Incidence, prognostic impact, and influence of antithrombotic therapy on access and nonaccess site bleeding in percutaneous coronary intervention. JACC Cardiovasc. Interv. 4(2), 191–197 (2011).
- Agostoni P, Biondi-Zoccai GG, de Benedictis ML et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; systematic overview and metaanalysis of randomized trials. J. Am. Coll. Cardiol. 44(2), 349–356 (2004).
- Mamas MA, Ratib K, Routledge H et al. Influence of access site selection on PCI-related adverse events in patients with STEMI: meta-analysis of randomised controlled trials. Heart 98(4), 303–311 (2012).
- Jolly SS, Yusuf S, Cairns J et al.; RIVAL trial group. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group,multicentre trial. Lancet 307, 1409–1420(2011).
- Romagnoli E, Biondi-Zoccai G, Sciahbasi A et al. Radial versus femoral randomizedinvestigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J. Am. Coll. Cardiol.60(24), 2481–2489 (2012).
- Vink MA, Amoroso G, Dirksen MT et al. Routine use of the transradial approach in primary percutaneous coronary intervention: procedural aspects and outcomes in 2209 patients treated in a single high-volume centre. Heart 97(23), 1938–1942 (2011).
- Lo TS, Ratib K, Chong AY, Bhatia G, Gunning M, Nolan J. Impact of access site selection and operator expertise on radiation exposure; a controlled prospective study. Am. Heart J. 164(4), 455–461 (2012).
- Ratib K, Mamas MA, Routledge HC, Ludman PF, Fraser D, Nolan J. Influence of access site choice on incidence of neurologic complications after percutaneous coronary intervention. Am. Heart J. 165(3), 317–324 (2013).
- Cooper CJ, El-Shiekh RA, Cohen DJ et al. Effect of transradial access on quality of life and cost of cardiac catheterization: a randomized comparison. Am. Heart J. 138(3 Pt 1), 430–436 (1999).
- Amoroso G, Sarti M, Bellucci R et al. Clinical and procedural predictors of nurse workload during and after invasive coronary procedures: the potential benefit of a systematic radial access. Eur. J. Cardiovasc. Nurs. 4(3), 234–241 (2005).
- Dirksen MT, Ronner E, Laarman GJ et al. Early discharge is feasible following primary percutaneous coronary intervention with transradial stent implantation under platelet glycoprotein IIb/IIIa receptor blockade. Results of the AGGRASTENT trial. J. Invasive Cardiol. 17(10), 512–517 (2005).
- Bertand OF, Rodes-Cabau J, Larose E et al. One-year clinical outcome after abciximab bolus-only compared with abciximab bolus and 12-hour infusion in the Randomized EArly Discharge after Transradial Stenting of CoronarY Arteries (EASY) study. Am. Heart J. 156(1), 135–140 (2008).
- Abdelaal E, Rao SV, Gilchrist IC et al. Same-day discharge compared to overnight hospitalization after uncomplicated percutaneous coronary intervention: a systematic review and meta-analysis. JACC Cardiovasc. Interv. 6(2), 94–112 (2013).
- Gilchrist IC, Rhodes DA, Zimmerman HE. A single center experience with same-day transradial-PCI patients: a contrast with published guidelines. Cathet. Cardiovasc. Interv. 79(4), 583–587 (2012).
- Le Corvoisier P, Gellen B, Lesault PF et al. Ambulatory transradial percutaneous coronary intervention: a safe, effective, and cost-saving strategy. Cathet. Cardiovasc. Interv. 81(1), 15–23 (2013).
- Amoroso G, Laarman GJ, Kiemeneij F. Overview of the transradial approach in percutaneous coronary intervention. J. Cardiovasc. Med. (Hagerstown) 8(4),230–237 (2007).
- Caputo RP, Tremmel JA, Rao S et al. Transradial arterial access for coronary and peripheral procedures: executive summary by the transradial committee of the SCAI. Cathet. Cardiovasc. Interv. 78(6), 823–839(2011).
- Cook S, Walker A, Hügli O et al. Percutaneous coronary interventions in Europe: prevalence, numerical estimates, and projections based on data up to 2004. Clin. Res. Cardiol. 96(6), 375–382 (2007).
- Hamon M, Pristipino C, Di Mario C et al. Consensus document on the radial approach in percutaneous cardiovascular interventions: position paper by the European Association of Percutaneous Cardiovascular Interventions and Working Groups on Acute Cardiac Care and Thrombosis of the European Society of Cardiology. EuroIntervention 8(11), 1242–1251 (2013).
- Bertrand OF, Rao SV, Pancholy S et al. Transradial approach for coronary angiography and interventions: results of the first international transradial practice survey. JACC Cardiovasc. Interv. 3(10), 1022–1031(2010).
- Lo TS, Nolan J, Fountzopoulos E et al. Radial artery anomaly and its influence on transradial coronary procedural outcome. Heart 95(5), 410–415 (2009).
- Louvard Y, Pezzano M, Scheers L et al. [Coronary angiography by a radial artery approach: feasibility, learning curve. One operator’s experience.] Arch. Mal. Coeur. Vaiss. 91(2), 209–215 (1998).
- Kanei Y, Kwan T, Nakra NC et al. Transradial cardiac catheterization: a review of access site complications. Catheter Cardiovasc. Interv. 78(6), 840–846 (2011).
- Stella PR, Kiemeneij F, Laarman GJ et al. Incidence and outcome of radial artery occlusion following transradial artery coronary angioplasty. Cathet. Cardiovasc. Diagn. 40(2), 156–158 (1997).
- Bernat I, Bertrand OF, Rokyta R et al. Efficacy and safety of transient ulnar artery compression to recanalize acute radial artery occlusion after transradial catheterization. Am. J. Cardiol. 107(11), 1698–1701 (2011).
- Kiemeneij F, Vajifdar BU, Eccleshall SC, Laarman GJ, Slagboom T, van der Wieken R. Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Catheter Cardiovasc. Interv. 58(3), 281–284 (2003).
- Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter Cardiovasc. Interv.46(2), 173–178 (1999).
- Mizuno S, Takeshita S, Taketani Y, Saito S. Percutaneous coronary intervention using a virtual 3-Fr guiding catheter. Catheter Cardiovasc. Interv. 75(7), 983–988 (2010).
- Call J, Sacrinty M, Applegate R et al. Automated contrast injection in contemporary practice during cardiac catheterisation and PCI: effects on contrast-induced nephropathy. J. Invasive Cardiol. 18(10), 469–474 (2006).
- Schöbel WA, Mauser M. Miniaturization of the equipment for percutaneous coronary interventions: a prospective study in 1,200 patients. J. Invasive Cardiol. 15(1), 6–11 (2003).
- Kaluski E, Moussa ID, Heuser RR et al. Automated contrast injectors for angiography: devices, methodology, and safety. Catheter Cardiovasc. Interv. 74(3), 459–464 (2009).
- Takeshita S, Shiono T, Takagi A et al. Percutaneous coronary intervention using a novel 4-French coronary accessor. Catheter Cardiovasc. Interv. 72(2), 222–227 (2008).
- Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion-patent hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterisation. Catheter Cardiovasc. Interv.72(3), 335–340 (2008).
- Politi L, Aprile A, Paganelli C et al. Randomized clinical trial on short-time compression with Kaolin-filled pad: a new strategy to avoid early bleeding and subacute radial artery occlusion after percutaneous coronary intervention. J. Interv. Cardiol. 24(1), 65–72 (2011).
- Angioplasty.org. Transradial (wrist) approach. www.ptca.org/radial/index.html
- Kiemeneij’s TRIbune.
▪▪ First randomized study of transradial versus transbrachial versus transfemoral access.
▪▪ First randomized study of transradial versus transfemoral access demonstrating a clinical advantage of transradial access.
▪ No excess of neurological complications in cases of transradial approach.
▪ First randomized study demonstrating safety of transradial same-day discharge percutaneous coronary intervention (PCI).
▪ Example of custom-made logistics: the Transradial PCI Lounge at Onze Lieve Vrouwe Gasthuis (Amsterdam, The Netherlands).
▪▪ Transradial access is proposed as the ‘preferred’ access strategy for PCI by the European Society of Cardiology.
▪ First report regarding radial occlusion and predictors after transradial PCI.
▪ First published series of ‘virtual’ 3-Fr PCI.
▪ First publication that demonstrates that patent hemostasis reduces radial occlusion after PCI.
▪ Websites