Research Article - Interventional Cardiology (2017) Volume 9, Issue 6
12 Lead electrocardiogram algorithm for the localization of accessory pathways using simple parameters in patients with typical Wolff-Parkinson-White syndrome
- Corresponding Author:
- Si Dung Chu
School of Medicine and Pharmacy
Vietnam National University, Hanoi, Vietnam
Tel: +84906086168
E-mail: chudungsi@gmail.com, dr.swiss.zhu@gmail.com
Submitted: October 06, 2017; Accepted: October 17, 2017; Published online: October 23, 2017
Abstract
Objective: This study was designed to characteristics of 12-lead electrocardiogram (ECG) to compare the position of accessory pathway (APs) in the typical Wolff-Parkinson-White (WPW) syndrome, can be build a new ECG algorithm for the localization of AP. Subjects and method: In 189 patients with typical WPW syndrome have a single anterogradely conducting APs on 12-lead ECG parameters were compared with the localization of APs identified by successful radiofrequency catheter ablation (RCFA). Results: We have developed a new ECG algorithm in localizing APs by the 12-lead ECG with simple parameters such as difference between the left or right side by positive/negative delta wave in V1, the anterior or posterior sites by positive/negative delta wave in at least 2/3 inferior lead, the septal or free wall sites by QRS complex transition in V1V2 lead or after V1V2/before V1; Different in LAL or LL region by R/S>1 or R/S<1, R in V1, the RL or RPL region by positive/negative QRS complex in at least 2/3 inferior lead, midseptal had QRS complex morphology’s specify (Qrs, qRs, qrS) in at least 1/3 inferior lead. The new ECG algorithm had high predictive value from 74.5% to 100%; The ECG parameters in algorithm were closely related to AP position. Conclusion: The 12-lead ECG parameters in typical WPW syndrome closely related to APs localization and can be used to a new ECG algorithm for the localization of AP by simple parameters.
Keywords
Localization of APs, 12-lead ECG, New ECG algorithm, WPW syndrome
Background
Wolff-Parkinson-White syndrome associated with an accessory AV connection (called Kent Bundle); the 12-lead ECG is character- ized by a shortened PR, prolonged QRS, with Delta wave [1,2].
Nowadays, RCFA of accessory pathway (AP) requires precise localization of the AP along the mitral and tricuspid annulus (gold standard) [2]. 12-lead ECG is the first step of great importance for localization of AP in patients with WPW syndrome. fte data obtained from the ECG parameters can be helpful the planning, procedure time and fluoroscopy time were shorten [2,3].
Some algorithms based on 12-lead ECG have been published predicting locations of AP. However, many studies known that difficulty for between other positions, some ECG algorithms had difficult paramaters or some algorithm was only focus on some regions [1-5]. fte purpose of this study was to analyse the 12-lead ECG of AP localization’s confirmed by successful RCFA to develop a new 12-Lead ECG algorithm using simple parameters.
Materials and Methods
Study design
Observational, cross-sectional, retrospective and prospective study.
Sample size
Using the formula for calculating the sample size for diagnostic studies:
• Estimated formular for the minimum sample size to Sensitivity (Se):
(TP+FN)/(1-incidence of disease)=[Z2(1-α/2)×SN×(1-SN)/ω2]/(1-0.003)=125
• Estimated formular for the minimum sample size to Specifity (Sp):
(FP+TN)/(1-incidence of disease)=[Z2(1-α/2) × SP × (1-SP)/ω2]/(1-0.003)=71
N: minimum sample size.
SN & SP: oscillation of Se & Sp are 80% and 90%; ω:Se & Sp index are 0.07.
TP: true positive, TN: true negative, FP: false positive, FN: false negative.
α: statistically significant at the 0.05 level. Z2(1-α/2)=1.96;
Incidence of disease (typical WPW syndrome) on surface ECG are 0.3%.
We selected to Specifity make the standard for the study; Therefore, N (minimum sample size) ≥71. Furthermore, the study needs enough 10 region for localization of AP [6-8].
Study contents
We studied 189 patients with typical WPW syndrome who had a single anterograde AP identified by successful RCFA were enrolled to build a new ECG algorithm propectively for the locate APs using simple parameters from Jannuary 2001 to June 2016.
WPW syndrome was defined as the 12-lead ECG is characterized by a shortened PR interval <120 milliseconds, prolonged QRS duration ≥110 milliseconds, with a delta wave [1]. Localization of accessory pathways confirmed by successfully RCFA (gold standard) [2].
Statistical analysis
We were expressed as mean±SD, compared by unpaired Student’s t test. We were performed on the AP Location confirmed by successful RCFA as the dependent variable and the 12-lead ECG parameters as the independent variables. Value of P<0.05 was considered statistically significant. Calculate for sensitivity (Se), Specificity (Sp), Positive predictive value (PPV), Negative predictive value (NPV) of our new ECG algorithm to localize the APs in 189 patients [1]. IBM SPSS 21.0 software was for analyzing data.
Results
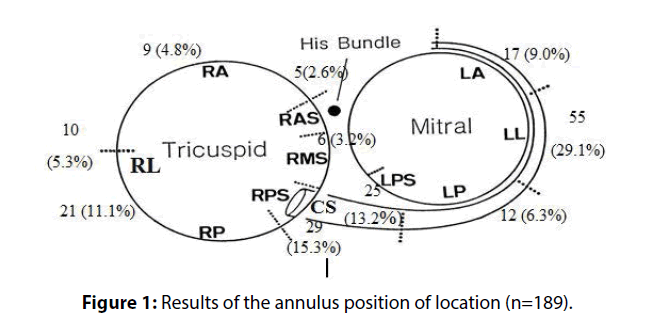
The study population consists of 189 patients, 99 men (52.4%) and 90 female (47.6%), p>0.05, 42.7±14.6 years. Among 189 accessory pathways Left sided accessory pathway was found in 109 patients (57.7%), and right sided accessory pathways had 80 patients (42.3%). 65 patients had septal accessory pathways (34.4%), 84 patients had left free wall sites (44.4%), and 40 patients had right free wall sites (21.2%) (Figure 1).
Characterization of the delta wave polarity in V1 lead for the left or right side
Left side includes left septal (LPS) and left free wall sites (LAL, LL, LPL) in around the mitral valve. Right side includes right septal (RAS, RMS, RPS) and right free wall sites (RAL, RL, RPL) in around the tricuspid valve.
Left side group had positive delta wave was most common at V1 lead found in 106 of 109 patients (97.2%) and right side group had negative delta wave was most common at V1 lead found in 67 of 80 patients (83.8%). Predictive value to localize the left or right side had Se 97.2%, Sp 83.8%, PPV 89.1%, NPV 95.7%, with R=-0.829 and correlation is significant at the 0.01 level (p<0.0001) (Table 5).
| Location Delta wave polarity in inferior | Right Anterolateral (RAL) |
Right Lateral (RL) |
Right posterolateral (RPL) |
Total | |
|---|---|---|---|---|---|
| Positive delta wave in atleast 2/3 inferior |
N | 9 | 1 | 1 | 11 |
| % | 100% | 10% | 4.8 | 27.5% | |
| Negative delta wave in atleast 2/3 inferior |
N | 0 | 9 | 20 | 29 |
| % | 0% | 90% | 95.2% | 72.5% | |
| Total (n): | 9 | 10 | 21 | 40 | |
Table 1: Characterizaton of positive/negative delta wave in at least 2/3 inferior.
| Location QRS complex polarity in inferior | Right Anterolateral (RAL) |
Right Lateral (RL) |
Right posterolateral (RPL) |
Total | |
|---|---|---|---|---|---|
| Positive delta wave in atleast 2/3 inferior |
N | 9 | 9 | 1 | 19 |
| % | 100% | 90% | 4.8 | 47.5% | |
| Negative delta wave in atleast 2/3 inferior |
N | 0 | 1 | 20 | 29 |
| % | 0% | 10% | 95.2% | 52.5% | |
| Total (n): | 9 | 10 | 21 | 40 | |
Table 2: Characterizaton of positive/negative QRS complex in at least 2/3 inferior.
| Location Delta wave polarity in inferior | Left Anterolateral (LAL) |
Left Lateral (LL) |
Left Posterolateral (LPL) |
Total (n) |
|
|---|---|---|---|---|---|
| Positive delta wave in atleast 2/3 inferior |
N | 17 | 52 | 1 | 70 |
| % | 100% | 94.5% | 8.3 | ||
| Negative delta wave in atleast 2/3 inferior |
N | 0 | 3 | 11 | 14 |
| % | 0% | 5.5% | 91.7% | ||
| Total (n) | 17 | 55 | 12 | 40 | |
Table 3: Characterizaton of positive/negative delta wave in at least 2/3 inferior lead.
| Location R/S ratio in V1 lead | Left Anterolateral (LAL) | Left lateral (LL) |
Total (n) |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| 1 | R/S ratio>1 | 13 | 76.5 | 14 | 25.5 | 27 |
| 2 | R/S ratio<1 | 2 | 11.8 | 34 | 61.8 | 36 |
| QRS: R morphology | 2 | 11.8 | 7 | 12.7 | 9 | |
| Total (n) | 17 | 55 | 72 | |||
Table 4: Characterizaton of R/S ratio in V1 lead for the left anterolateral or left lateral.
| Predictive value Location |
Se% | Sp% | PPV% | NPV% | Correlation (R) |
Significant (level) |
|---|---|---|---|---|---|---|
| Left or right side | 97.2 | 83.8 | 89.1 | 95.7 | -0.829 | <0.01 |
| Anterior or posterior site | 100 | 93.1 | 83.8 | 73.7 | 0.883 | <0.01 |
| Septal or free wall site | 89.2 | 87.1 | 78.4 | 93.9 | 0.743 | <0.01 |
| RAL or RL/RPL region | 100 | 93.5 | 81.8 | 100 | 0.875 | <0.01 |
| RAL/RL or RPL region | 94.7 | 95.2 | 94.7 | 95.2 | 0.900 | <0.01 |
| RL or RPL region | 90 | 95.2 | 90 | 95.2 | 0.852 | <0.01 |
| LAL/LL or LPL region | 95.8 | 97.1 | 98.6 | 78.6 | 0.822 | <0.01 |
| LAL or LL region | 76.5 | 74.5 | 48.1 | 91.1 | 0.448 | <0.01 |
| MS or RAS/RPS/LPS region | 83.3 | 86.4 | 38.5 | 98.1 | 0.505 | <0.01 |
Table 5: Overall predictive value to localize the AP and correlation between the AP location and 12-lead ECG.
Characterization of the QRS complex transition on 12-lead ECG for the septal or free wall location
Septal location includes right septal (RAS, RMS, RPS) and left septal (LPS). Free wall location includes Right free wall lateral (RAL, RL, RPL) and Left free wall lateral (LAL, LL, LPL).
Classified transition of septal location was most common at V1,V2 lead (between V2V3 including) found in 58 of 65 patients (89.2%); While classified transition of free wall lateral sites was most common at after V1V2 (V3-V6)/before V1 lead found in 108 of 124 patients (87.1%). Right free wall lateral had QRS complex transition at after V1V2 (V3-V6) found in 36 of 40 patients (90%); Left free wall lateral had QRS complex transition at V1V2 (V3-V6) or before V1 lead found in 72 of 84 patients (85.7%). Predictive value to localize the septal or free wall site had Se 89.2%, Sp 87.1%, PPV 78.4%, NPV 93.9%, with R=0.743 (Correlation is significant at the 0.01 level, p < 0.0001) (Table 5).
Characterization of delta wave polarity in at least 2/3 inferior lead with anterior or posterior location
Anterior location includes anterolateral (LAL, RAL) and anteroseptal (RAS) of mitral or tricuspid valves. Posterior location includes posterolateral (RPL, LPL), and posteroseptal (RPS, LPS) of mitral or tricuspid valves.
Classified anterior location had positive delta wave was most common in at least 2/3 inferior lead (DII, DIII, aVF) found in 31 of 31 patients (100%); While posterior location had negative delta wave was most common in at least 2/3 inferior lead found in 81/87 patients (93.1%). Predictive value to localize the anterior or posterior site had Se 100%, Sp 93.1%, PPV 83.8%, NPV 73.7%; with R=0.883 (Correlation is significant at the 0.01 level, p < 0.0001) (Table 5).
Characterization of 12-lead ECG for the right free wall lateral location
Right free wall location had QRS complex transition was most common at after V1,V2 (V3-V6) lead found in 36 of 40 patients (90%). Beside, right free wall lateral had negative delta wave was most common in V1 lead found in 32 of 40 patients (80%). RAL region had positive delta wave was most common in at least 2/3 inferior lead (DII, DIII, AVF) found in 9 of 9 patients (100%); while RPL region had negative delta wave was most common at least 2/3 inferior lead found in 20 of 21 patients (95.2%). However, RL region had negative delta wave was most common in at least 2/3 inferior lead found in 9 of 10 patients (90%). ftus, both includes RL/RPL had negative delta wave was most common in at least 2/3 inferior lead found in 29 of 31 patients (93.5%) (Table 1). fterefore, predictive value to localize the RAL or RL/RPL region had Se 100%, Sp 93.5%, PPV 81.8%, NPV 100%, R=0.875 (Correlation is significant at the 0.01 level, p < 0.0001).
Classified QRS complex polarity in inferior lead (DII, DIII, aVF) for the RL region and RPL region: RL region had positive QRS complex was most common in at least 2/3 inferior lead found in 9 of 10 patients (90%); While, RPL region had negative QRS complex was most common in at least 2/3 inferior lead found in 20 of 21 patients (95.2%) (Table 2). Predictive value to localize the RL or RPL region had Se 90%, Sp 95.2%, PPV 90%, NPV 95.2%, R=0.852; Predictive value to localize the RAL/RL or RPL region had Se 94.7%, Sp 95.2%, PPV 94.7%, NPV 95.2%, R = 0.9 (Correlation is significant at the 0.01 level, p < 0.0001)(Table 5).
Characterization of 12-lead ECG for the left free wall location
Left free wall location had QRS complex transition was most common at after V1V2 lead (V3-V6) or before V1 lead found in 72 of 84 patients (85.7%). Beside, left free wall lateral had positive delta wave was most common in V1 lead found in 83 of 84 patients (98.8%).
Both in LAL/LL region had positive delta wave was most common in at least 2/3 inferior lead (DII, DIII, aVF) found in 69/72 patients (95.8%); while LPL region had negative delta wave was most common in at least 2/3 inferior lead as above (91.7%) (Table 3). Predictive value to localize the LAL/LL or LPL region had the Se 95.8%, Sp 91.7%, PPV 98.6%, NPV 78.6%, R=0.822 (Correlation is significant at the 0.01 level, p < 0.0001) (Table 5). LAL region was most common with R/S>1 at V1 lead found in 13 of 17 patients (76.5%). LL region had R/S<1 (62,3%) or QRS complex’R morphology (25.5%) was most common in V1 lead found in 41 of 55 patients (74.5%); however, LL region had R/S>1 in V1 lead found in 14 of 55 patients (25.5%) (Table 4). fterefore, the result showed that predictive value to localize the LAL or LL region had the Se 76.5%, Sp 74.5%, PPV 48.1%, NPV 91.1%, R=0.448 (Correlation is significant at the 0.01 level, p < 0.0001) (Table 5).
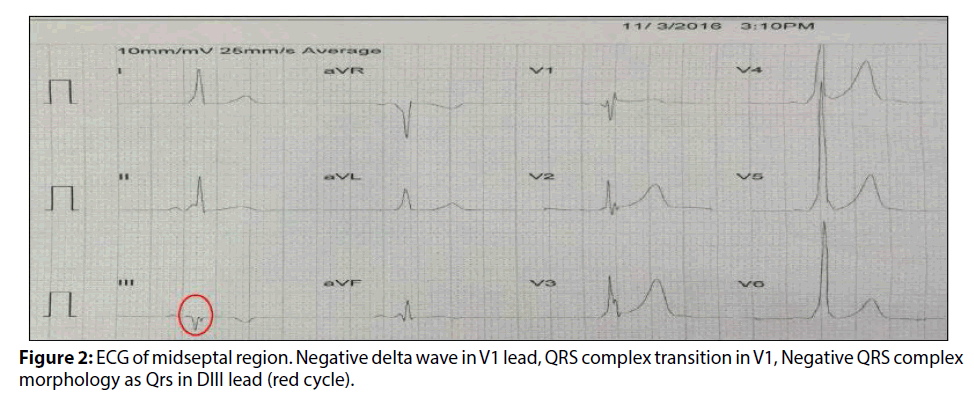
Characterization of 12-lead ECG for the septal location
Septal location had QRS complex transition was most common at V1,V2 lead (between V2V3 including) found in 58 of 65 patients (89.2%). Left septal had positive delta wave was most common in V1 lead found in 23 of 25 patients (92%) and right septal had negative delta wave was most common in V1 lead found in 35 of 40 patients (87.5%). Anteroseptal had positive delta wave was most common in at least 2/3 inferior lead found in 5 of 5 patients (100%) and posteroseptal had negative delta wave was most common in at least 2/3 inferior lead found in 50 of 54 patients (92.6%) (Figure 2).
Classified the QRS complex morphology of midseptal (RMS) region: MS region had specific QRS complex morphology (Qrs, qRs, qrS) was most common in at least 1/3 inferior lead found in 5 of 6 patients contributing 83.3% among total number of midseptal. Conducting among 59 accessory pathway of no midseptal (anteroseptal and posteroseptal) only found in 8 patients (13.6%) had QRS complex morphology as below (8 patients were met in posteroseptal: 4 AP in RPS and 4 AP in LPS region) (Figure 2). Predictive value to localize the RMS or RAS/RPS/LPS region had the Se 83.3%, Sp 86.4%, PPV 38.5%, NPV 98.1%, R=0.505 (Correlation is significant at the 0.01 level, p < 0.0001) (Table 5).
Discussion
Characteristic 12-lead ECG in patient with left side pathway had strongly positive delta wave in V1 lead are noted (97.2%), while right side pathway had strongly negative delta wave in V1 leasd are noted (83.8%). ftis is very useful in selecting the approach of the catheter is the vein or artery; All right-sided AP were ablated with the use of transvenous atrial approach through the femoral vein, while left-side AP were ablated with retrograde arterial approach; if this approach failed the pathway was ablated using antegrade transeptal approach [2].
Some ECG algorithms have been published predicting locations of left-sided or right-sided accessory pathway by positive of negative delta wave [1-3,9]. A study showed that diagnosis of left or right-side accessory pathway by other ECG parameters such as D’ Avila was used to positive or negative QRS complex in V1 [4]. Chern-En Chiang was used to positive or negative delta wave in V1, V3, DIII, aVF lead and showed that R/S<1 or R/S>1 in V1 lead can be suggested that was in the right or left-side [10], Mauricio S. Arruda also found that R/S>1 in V1 lead was the left free location and R/ S<1 in V1 lead was the right side [11]. Muhammad also used to a R/S<1 in aVL lead to predict left side [9], and Noriko was used to only R/S ratio <0.5 or R/S>0.5 in V1 lead can be predicting right or left-side AP [12]; however, the problem was that many left side AP such as left lateral, left septal location had positive delta wave with R/S<0.5; therefore it’s very dificult between right side AP with left side AP by only for R/S ratio in V1 lead [12]. We were not used to the R/S ratio at aVL lead as well as R/S ratio (or QRS) in V1 lead for the suggest a right or left side.
Characteristic 12-lead ECG in patient with septal location pathway had QRS complex transition was most common at V1,V2 lead are noted (89.2%), While free wall location had QRS complex transition was most common at after V1V2/before V1 lead are noted (87.1%).
Some algorithms based on ECG not-yet finding different between anteroseptal with right anterolateral APs, difficult in posteroseptal with posterolateral (left or right). However, many studies were showed that QRS complex transition can be used to predicting locations of septal or free wall accessory pathway [1,2,9].
Characterization of delta wave polarity in at least 2/3 inferior lead (DII,DIII,aVF) for the anterior or posterior location.
Characteristic electrocardiogram in a patient with antero group pathway had strongly positive delta waves in at least 2/3 inferior are noted (100%), while postero group pathway had strongly negative delta waves in at least 2/3 inferior leads (II, III, aVF) are noted (93.1%).
Some ECG algorithms have been published predicting locations of anterior or posterior location by positive or negative delta wave in inferior lead as below [1,2,9]. However, some studies were only forcus on some positions in anterior and posterior location [13]. The results showed that the RAL region had positive delta wave was most common in at least 2/3 inferior lead are noted (95.8%), and includes RL/RPL region had negative delta wave was most common in at least 2/3 inferior lead as above with hight accuracy (93,5%), beside results showed that very dificulty in localizing between two position were RL and RPL region, can be explained by the two regions have similar in electrophysiological side.
According to the statistics as above, the RL region and RPL are often found in the negative delta way in at least 2/3 inferior lead. We performed the characteristic of QRS complex polarity in at least 2/3 inferior lead for the localizing two regions (RL or RPL). Result showed that the RL region had positive QRS complex was most common in at least 2/3 inferior lead (90%); While, the RPL region had negative QRS complex was most common in at least 2/3 inferior lead (95.2%). Thus, this parameter (QRS complex polarity) helped to suggesting that the RL region or RPL region.
Many studies showed that difficulty in localizing between other positions of right free wall pathways. Andre D’ Avila showed that not-yet localizing between two locations as above [4]. Many studies not-yet localizing between other right free wall as Pedro (1996) was used to characteristic of QRS polarity in DII, V1 and V2 lead, can be add to positions (RIP, RI) by one location; Pedro Iturralde selected two locations of right free wall were right anterolateral (RA) and group of includes RIP/RI location [5]. Noriko was used to R/S in V1, V2, AVF, and inferior lead can localizing right anteroseptal-anterolateral and right lateral (RAS, RA, RL) defined by one location with characteristic were R/S ratio <0.5 in V1 and V2 lead, R/S ratio <1 in aVF lead; Noriko Taguchi selected two locations were RA/ RL region and RPL/RP region [12].
In fact, technical ablication by RCFA for accessory pathways in free wall lateral site are rather dificult. Thus, We have been predicted RAL or RL/RPL region by positive or negative delta wave in at least 2/3 inferior, difference between RL and RPL region by positive or negative QRS complex in at least 2/3 inferior lead; which can help the doctors to perform a rapid onset of accessory pathway location on the tricuspid valve forwards or backwards, or within 1-2 cm of the valve; help to facilitate mapping techniques and shorten time radiofrequency ablation [1-3].
Characterization of 12-lead ECG for the Left free wall location
Characteristic 12-lead ECG in patient with the LAL region had strongly positive delta wave in at least 2/3 inferior leads (II, III, aVF) are noted (100%), while the LPL region had strongly negative delta waves in at least 2/3 inferior leads (II, III, aVF) are noted (91.7%). Specialists, the LL region had positive delta wave was most common at least 2/3 inferior leads are noted (94.5%) as the same characteristic of the LAL region.
Therefore, build to a group of includes LAL/LL location had positive delta wave was most common in at least 2/3 inferior lead are noted (95.8%), and LPL region had negative delta wave was most common in at least 2/3 inferior lead as above (91.7%).
According to the statistics as above, the LAL region and LL region are often found in the positive delta wave in at least 2/3 inferior leads are noted. We performed the characteristic of R/S ratio in V1 lead for the localizing between these two regions. Result showed that the LAL position was most common with R/S ratio>1 in V1 lead (76.5%); While, the LL region was most common with R/S<1 or QRS complex’s R morphology in V1 lead are noted (74.5%). Thus, this parameter (R/S) helped to suggesting that the LAL region or LL region but it’s not high accuracy, can be explained by between two location have plenty of sequential zones and similar in electrophysiological angle, so there are many similarities [1].
Many studies showed that difficulty in localizing between left anterolateral or left lateral pathways as well as difficulty in different between other positions of left free wall pathways. Pedro Iturralde (1996) selected two locations of left free wall were includes LPL/LAS region and include LIP/LI region [5]. Noriko Taguchi (2013) selected two locations were includes LA/LL region and includes LP/LPL region [12].
Thus, We have been suggested includes LAL/LL region and RPL region by positive or negative delta wave in at least 2/3 inferior, difference between LAL and LL region by R/S ratio>1 or R/S<1, R in V1 lead; which can help the doctors to perform a rapid onset of accessory pathway location on the mitral valve forwards or backwards, or within 1-2 cm of the valve; help to facilitate mapping techniques and shorten time radiofrequency ablation [1-3].
Characterization of the QRS complex on 12-lead ECG for the septal location
Classified transition of septal location was most common at V1,V2 lead are noted (87.8%). The septal accessory pathway location with Anatomic relation of the atrioventricular junction in relation to other cardiac structures, especially in the septal region’s transitional cell zone [14].
Some algorithms based on ECG not-yet finding different between anteroseptal with right anterolateral APs, difficult in posteroseptal with posterolateral (left or right). However, many studies were showed that transition of QRS complex can be used to predicting locations of septal or free wall accessory pathway [1-3,9].
Left septal had positive delta wave was most common at V1 lead (100%), while right septal had negative delta wave was most common at V1 lead (89.3%). This is very useful in selecting the approach of the catheter is the vein or artery [2].
Characteristic 12-lead ECG in patient with an anteroseptal AP had strongly positive delta wave in at least 2/3 inferior leads (II, III, aVF) are noted (100%), while posteroseptal AP had strongly negative delta wave in at least 2/3 inferior leads (II, III, aVF) are noted (88.9%). Successful ablation was performed at a location on the anteroseptal annulus where a His bundle electrogram was being recorded. Ablation was very anterior, and thus not in the vicinity of the compact AV node [14,15]. The posterior region is a triangular structure between the left ventricle and the right ventricle, located at the base of the triangle kock, can be mixed between left and right in pre-stimulus levels. Successful ablation was performed at a location on the posteroseptal annulus where a His bundle electrogram was being recorded. Ablation was very anterior, and thus not in the vicinity of the compact AV node. The posteroseptal region is specifically located between the posterosuperior process of the left ventricle and inferior wall or the right atrim. Many studies have shown difficulty in discriminating left or right side posteroseptal AP; however, it has been suggested that a postivive or negative delta wave in V1 can further different in the left or right side posteroseptal AP [1,12].
Some ECG algorithms have been published predicting locations of anterior or posterior accessory pathway by positive or negative delta wave in inferior lead as below [1,3,10]. However, some studies were only forcus on some positions in anterosetal and posteroseptal accessory pathway [13].
Many studies have reported that the midseptal is the only true muscular septal area between the offset attachments of the mitral and tricuspid valves, while the previously named anterior and posterior septal areas are those regions that are anterior and posterior to the true septum. Midseptal pathways are inserted into the triangle of Koch region, close to the compact AV node. Accurate assessment of pathway slant and ablation preferably of the ventricular insertion site along with the use of cryoenergy may all be required to minimize the risk of AV block when ablating pathways in this region [15]. Classified QRS complex morphology (Qrs, qRs, qrS) of midseptal location was most common at inferior lead (DII, DIII, aVF) found in 83.3% among total number of midseptal. This “Qrs morphology” in at least 1/3 inferior lead was to distinguish between midseptal from other septal regions (RAS, RPS, LPS). The RAS/RPS/LPS regions (59 patients) only found in some patients of posteroseptal location had QRS complex morphology as below.
Andre D’Avila (n=140) showed that the QRS complex polarity did not allow the correct localization of midsepta1 region; However, DIII lead showed a very similar QRS complex morphology in 5/10 patients with midseptal; The QRS complex was characterized by a large “Q” wave followed by a small “r” wave and an “s” wave in DIII lead. This “Qrs pattern” in DIII lead was highly specific for a midsepta1 location but the sensitivity was not high, may be the author was only used to Qrs pattern in DIII lead for a midseptal [4]. We were using the spesify QRS pattern (Qrs, qrS, qRs morphology) for in at least 1/3 inferior lead (DII, DIII, aVF) and not only for DIII lead.
The Result (Table 5) showed that overall of predictive value to localize the AP had high predictive value with Se and Sp from 74.5% to 100%; however, PPV of LAL or LL region was not high but NPV of LAL or LL region was very high (91.1%), PPV of MS or RAS/ RPS/LPS region was not high but NPV of the MS or RAS/RPS/LPS was very high (98.1%).
Relationship between the 12-lead ECG parameters and AP location was closely related. The Left or right side, anterior or posterior site, RAL or RL/RPL, RAL/ RL or RPL, RL or RPL, LAL/LL or LPL region were very strongly correlation (the left or right side was antithetic correlation). The Septal or free wall site was strongly correlation. The LAL or LL, MS or RAS/RPS/ LPS region were mean-strongly correlation.
Conclusion
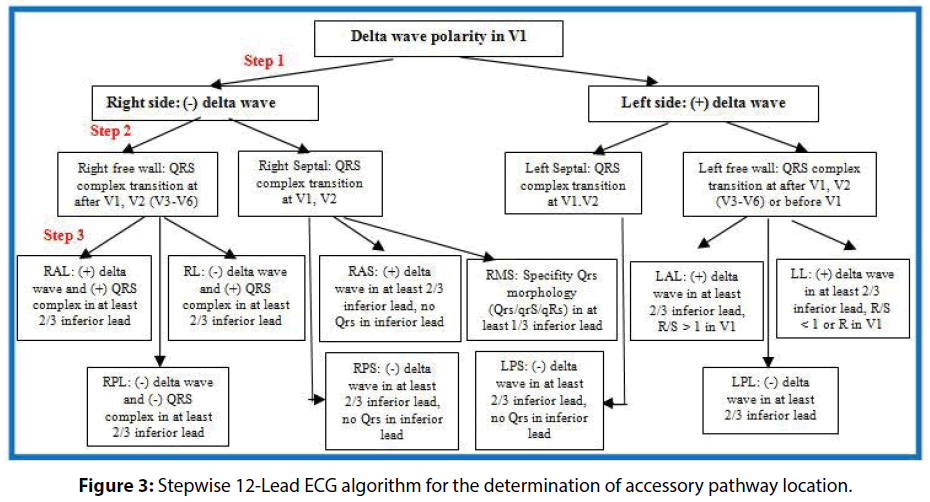
We have developed a new algorithm in localizing accessory pathways by 12-lead ECG with simple parameters (Figure 3). We found that the right side or left side had negative delta wave (83.3%) or positive delta wave (97.2%) was most common at V1 Lead. Anterior location or posterior had postive delta wave (100%) or negative delta wave (93.1%) was most common at least 2/3 inferior lead. Septal location had QRS complex transition was most common at V1,V2 lead (89.2%) and free wall lateral location had QRS complex transition was most common at after V1,V2(V3-V6) lead or before V1 lead (87.1%). Difference between right lateral and right posterolateral by positvie (90%) or negative QRS complex (95.2%) was most common at least 2/3 inferior lead. Defferent between anterolateral and left lateral by R/S>1 (76.5%) and R/S<1 or R (74.5%). Midseptal location had QRS complex morphology’s specify QRS morphology (Qrs, qRs, qrS) in at least 1/3 inferior lead (83.3%). The 12-lead ECG parameters in typical WPW syndrome closely related to AP position and can be used to predict the AP location.
References
- Surawicz B, Knilans TK. Chou’s Electrocardiography in clinical practice: Adult and Pediatric (6th Ed). Elservier Saunders pp: 481-508 (2008).
- Basiouny T, Chillou CD, Fareh S, et al. Prospective validation of a sezer ECG agorithm for localization of accrssory pathways in patients with Wolff-Parkinson-White syndrome. AAMJ. 10: 1340-1348 (2012).
- Robert L, Douglas LW. Value of the resting 12 lead electrocardiogram and vectorcardiogram for locating the accessory pathway in patients with the Wolff-Parkinson-White. Br. Heart. J. 4: 324-332 (1987).
- D' avila A, Brugade J, Skeberis V, et al. A fast and reliable algorithm to localize accessory pathways based on the polarity of the QRS complex on the surface ECG. During Sinus Rhythm. PACE. 18: 1615-1627 (1995).
- Iturralde P, Gomez VA. A new ECG algorithm for the localization of accessory pathways using only the polarity of the QRS complex. J. Electrocardiol. 29(4): 289-299 (1996).
- Akobeng AK. Understanding diagnostic tests 1: Sensitivity, specifity and predictive values. Acta. Paediatrica. 96: 338-341 (2007).
- Parikh R. Understanding diagnostic tests 1: Sensitivity, specificity and predictive values. Ind. J. Ophthalmol. 56: 1-45 (2008).
- Mohammad AB. Requirements for Minimum sample Size for Sensitivity and Specifity Analysis. J. Clin. Diag. Res. 10: YE01-YE06.
- Muhammad AD, Abdul RA. Localization of accessory pathways according to AP Fitzpatrick ECG criteria in patients with Wolff-Parkinson-White syndrome in our population. Pak. Heart. J. 41(2): 29-38 (2008).
- Chern-En C, Wee ST. An accurate stepwise electroardiographic algorithm for localization of accessory pathways in patients with Wolff-Parkinson-White syndrome from a Comprehensive Analysis of Delta Waves and R/S Ratio During Sinus Rhythm. Am. J. Cardiol. 76: 40-46 (1995).
- Arruda MS, Wang X. Development and validation of an ECG algorithm for identifying accessory pathway ablation site in Wolff-Parkinson. J. Cardiovasc. Electrophysiol. 9: 2-12 (1998).
- Noriko T, Yasuya I. A simple algorithm for localizing accessory pathways in patients with Wolff-Parkinson-White syndrome using only the R/S ratio. J. Arrhy. 30(6): 439-443 (2014).
- Thomas R, Daniel S. A new algorithm for concealed accessory pathway localization using T-wave-subtracted retrograde P-wave polarity during orthodromic atrioventricular reentrant tachycardia. J. Interv. Card. Electrophysiol. 22: 55-63 (2008).
- Macedo PG, Bisco SE, Asirvtham SJ. Septal Accessory Pathway: Anatomy, Causes for Difficulty, and an Approach to Ablation. Ind. Pacing. Electrophysiol. J. 10: 292-309 (2010).
- Cheng A, Houge CW. Cardiac Electrophysiology: Diagnosis and Treatment. Anesthesiology. Kaplans. Cardiac. Anesthesia. Exp. Consult. Premium. 4: 6e (2014).