Research Article - Clinical Practice (2018) Volume 15, Issue 2
A clinical study of adjuvant chemotherapy in younger and elder rectal cancer patientsA
- Corresponding Author:
- Annica Holmqvist
Department of Clinical and Experimental Medicine
Linköping University, Linköping, Sweden
E-mail: annika.holmqvist@regionostergotland.se
Abstract
The role of postoperative chemotherapy (CT) is still unclear and the evidence for recommendations of adjuvant therapy in rectal cancer (RC) is sparse. The aim of this study was to investigate the outcome and tolerability of postoperative adjuvant CT in a clinical study of patients with RC ≥ 69 or <69 years. Two hundred and thirty one patients with stage II-IV rectal adenocarcinoma from the South East Health Care Region of Sweden were included in this retrospective nested case control study. The patients received radiotherapy (RT) or chemoradiation (CRT) followed by surgery. Seventy-six patients were subjected to postoperative adjuvant CT. In all patients and in patients ≥ 69 years, patients with capecitabine had an improved overall survival (OS) and cancer specific survival (CSS) compared to patients without adjuvant CT (p=0.01, p=0.02), (p=0.03, p=0.05) independent of sex, age, TNM stage, differentiation grade and preoperative RT (p=0.003, HR 0.29, p=0.002, HR 0.13, p=0.006, HR 0.26, p=0.007, HR 0.13, 95% CI), but not in patients <69 years (p>0.05). In patients ≥ 69 years, treatment with capectiabine/oxaliplatin were related to worse CSS compared to patients with capectiabine alone (p=0.02). Fifty seven percent of the patients with capectiabine/oxaliplatin and 17% with capecitabine alone had to stop the treatment due to severe side effects. Adjuvant capecitabine is related to better OS and CSS in RC patient’s ≥ 69 years. Oxaliplatin containing regimen should be administered with caution, especially in elderly patients.
Keywords
adjuvant chemotherapy, elderly patients, rectal cancer, survival, younger patients
Abbreviations
CT: Chemotherapy; CC: Colon Cancer; CI: Confidence Interval; CRC: Colorectal Cancer; CRT: Chemo-Radiation; DSF: Disease Free Survival; DRFS: Distant Recurrence Free Survival; HR: Hazard Ratio; RC: Rectal Cancer; RT: Radiotherapy; TME: Total Mesorectal Excision; TNM: Tumor Node Metastasis
Introduction
Colorectal cancer (CRC) is one of the leading causes of cancer-related death in both genders worldwide. In Sweden, there are around 5500 new cases each year, where 2000 of these cases are rectal cancers (RC). For many years, colon and rectal cancer have been considered as one disease and many oncological studies have evaluated these two together. In recent years, it has been shown that colon and rectal cancers have different biological behavior despite being seemingly identical tumors [1]. Colon and rectal cancers have differences in the lymphatic drainage and the location of the large blood vessels. RC also has more local recurrences and fewer distant metastases compared to colon cancer (CC) [1]. Even gene expression profile differs significantly in CC and RC [2,3].
The aim of postoperative adjuvant chemotherapy (CT) is to eliminate circulating tumor cells, to reduce the risk of recurrence and improve patient’s survival. In previous studies on CC patients it was shown that 5 fluorouracil (5- Fu) based adjuvant CT was related to improved survival compared to patients without adjuvant treatment [4] and that capecitabine administered orally was equally effective compared to bolus 5-Fu/leukovorin [5]. Further, the addition of oxaliplatin to capecitabine improved the disease free survival (DFS) [6]. In RC patients, the role of postoperative CT is still not yet clear. Some studies have found a positive relationship between survival and adjuvant CT [7,8] while others showed no survival benefit [9].
Due to increased life expectancy, the number of elderly patients is increasing today and the median age at diagnosis has now reached the age of 70 years. It has been shown that patients more than 70 years old are underrepresented in clinical trials, although age itself should not be considered as a contraindication to different therapies [10]. The researchers concerns have been that elderly patients’ body has different physiology which can lead to decreased CT clearance and risk for side effects. They also have other diseases and multiple medications which may interact with CT. Today, it is difficult to define which patients should be considered as elderly only based on their chronological age. It is also difficult to compare the data from different CT trials since most of the clinical trials only enroll younger patients and data for older patients are extrapolated [10,11]. It has been suggested, that combined CT for elderly patients should be used with caution due to increased risk of severe toxicity [12,13]. Recently, it was shown that elderly patients with adjuvant 5-Fu was related to a better survival compared to patients with surgery alone [14]. The addition of adjuvant oxaliplatin to 5-Fu in elderly patients has not been recommended due to increased toxicity and no benefit regarding survival [13].
The aim of this study was to analyse the differences in treatment response, side effects and compliance between patients with RC with adjuvant CT and patients without adjuvant treatment by also considering younger <69 years and elder patients ≥ 69 years.
Patients and Methods
Data
A retrospective medical review was performed on all patients (n=390) diagnosed (between 2004-2012) with rectal adenocarcinoma from the Southeast Swedish Health Care Region. Out of the 390 patients, 111 patients with stage I disease were excluded from further analyses since none of these patients received adjuvant CT. Also patients with poor performance status who did not went through primary surgery (n=28), patients who received a palliative sigmoidostomy (due to advanced disease at diagnosis, n=3) and 17 patients in the group without adjuvant CT who had microscopically not radical surgery (R1), were excluded. Further statistical analyses are based on the remanining 231 patients with stage II-IV disease as shown in TABLE 1.
| Variables | No adjuvant CT n=155 (%) |
Adjuvant CT n=76 (%) |
All patients n=231 |
p-value |
|---|---|---|---|---|
| Sex | 0.94 | |||
| Female | 64 (41) | 31 (41) | 95 (41) | |
| Male | 91 (59) | 45 (59) | 136 (59) | |
| Age | ||||
| <69 years | 59 (38) | 54 (71) | 113 (49) | <0.0001 |
| ≥69 years | 96 (62) | 22 (29) | 118 (51) | |
| TNM | ||||
| IIA-IIB | 80 (51) | 14 (18) | 94 (41) | <0.0001 |
| IIIA | 6 (4) | 5 (7) | 11 (5) | |
| IIIB | 23 (15) | 25 (33) | 48 (21) | |
| IIIC | 14 (9) | 21 (28) | 35 (15) | |
| IV | 32 (21) | 11 (14) | 43 (18) | |
| Differentiation grade | ||||
| Good | 6 (4) | 1 (2) | 7 (3) | 0.09 |
| Moderate | 103 (66) | 42 (55) | 145 (63) | |
| Poor | 46 (30) | 33 (43) | 79 (34) | |
| Mucinous | ||||
| No | 137 (88) | 64 (84) | 201 (87) | 0.37 |
| Yes | 18 (12) | 12 (16) | 30 (13) | |
| Vacular invasion | ||||
| No | 129 (83) | 47 (62) | 176 (76) | 0.0003 |
| Yes | 26 (17) | 29 (38) | 55 (24) | |
| Perineural growth | ||||
| No | 141 (91) | 52 (68) | 193 (84) | <0.0001 |
| Yes | 14 (9) | 24 (32) | 38 (16) | |
| Distant recurrence | ||||
| No | 103 (66) | 41 (54) | 144 (62) | 0.07 |
| Yes | 52 (34) | 35 (46) | 87 (38) | |
| Local recurrence | ||||
| No | 145 (94) | 67 (88) | 212 (92) | 0.16 |
| Yes | 10 (6) | 9 (12) | 19 (8) | |
| Neoadjuvant CT | ||||
| No | 130 (84) | 55 (72) | 185 (80) | 0.04 |
| Yes | 25 (16) | 21 (28) | 46 (20) | |
| Type of preoperative RT | ||||
| No preoperative RT | 43 (28) | 10 (13) | 53 (23) | 0.05 |
| Short RT 5 × 5 Gy | 72 (46) | 43 (57) | 115 (50) | |
| Long RT ±CT | 40 (26) | 23 (30) | 63 (27) | |
| Surgery | ||||
| Rectum amputation | 56 (36) | 30 (39) | 86 (37) | 0.57 |
| TME | 92 (59) | 45 (59) | 137 (60) | |
| TEM | 3 (2) | 0 | 3 (1) | |
| Proctocolectomy | 4 (3) | 1 (1) | 5 (2) | |
| Resection margin | ||||
| Tumour free | 155 (100) | 64 (84) | 219 (95) | <0.0001 |
| Tumour | 0 (0) | 12 (16) | 12 (5) | |
| Distant to anal verge (cm) | 8,08 | 7,64 | 7,93 |
Table 1. Patients and characteristics of the 231 patients with RC without and with adjuvant CT.
Out of the 231 patients, 76 (33%) were subjected to postoperative adjuvant CT. The mean follow up duration was 56 months for overall survival (OS), 56 months for cancer specific survival (CSS) (range 0-133) and 44 months for disease free survival (DFS) (range 0-131). The mean age of the patients was 69 (range 25-90) and the mean time from operation to start CT was 54 days (range 23-115, mean 7.7 weeks). The cut-off point for further analyses was selected as 69 years, since the mean age of the patients in this study was 69 years. Descriptive data such as sex, age, histological examination, tumor location, pathological and radiological stage, time of diagnosis, date of surgery, information about CT and RT were obtained from patients’ oncological and surgical records. All information about the side effects of cancer treatment, CT dose reduction and regimens change were taken from the patients’ oncological files.
Treatment
The preoperative treatment consisted mostly of RT given with 25 Gy in 5 fractions. The surgery was performed with the median of 10 days (range 1-13) after RT. Fifty-seven percent (n=43) of the patients with adjuvant CT (n=76) received short term RT before surgery, as shown in TABLE 1. For advanced RC (T4 tumors), a long-term RT was given with concomitant CT with 50,4 Gy in 28 fractions and the patients were operated with a median of 39 days (range 20-75) after RT. Thirty percent (n=23) of the patients with adjuvant CT received long RT ± CT before surgery as shown in TABLE 1.
Patients were planned to receive a total of 8 treatments (21 days of each cycle) of postoperative adjuvant CT. During the CT treatment, patients were monitored every 3 weeks with interviews and blood sample for signs of acute toxic effects. Forty-two percent (n=32) of the adjuvant CT consisted of capecitabine 1000 mg/m2 × 2 or the combination of capecitabine 850 mg/m2 × 2/oxaliplatin 130 mg/m2 38% (n=29). Of the patients ≥ 69 years, 73% (n=16) received capecitabine, 23% (n=5) capecitabine/ oxaliplatin and 4% (n=1) had other treatments. In the group of patients with the age of <69 years, 30% (n=16) received capecitabine, 44% (n=24) capecitabine/oxaliplatin and 26% (n=14) other treatments. In total, 19% (n=15) of the patients with adjuvant CT received other treatments, therefore further survival analyses are based on these 2 treatment regimes.
The study protocol was approved by the regional ethical committee in Linköping, Sweden (reference number: 2014/79-31) according to the World Medical Associations Declaration of Helsinki 1964 and the Amendment of Tokyo in 1975. All the patients in this study had signed a written consent (just before they went through the surgery).
Statistics
Chi-square method was used to analyze the differences between patients with or without adjuvant CT in relation to clinical and histological factors. Cox’s proportional hazard model was used to estimate the relationship between adjuvant CT and survival including both univariate and multivariate analyses. Survival curves were computed according to the Kaplan-Meier method. The tests were twosided and p-value of p<0.05 was considered statistically significant.
Results
Adjuvant CT in relation to survival
At first, we investigated the relationship between adjuvant CT, OS and CSS in the whole group of patients (n=231), and in patients <69 years and ≥ 69 years, respectively. Next, the subgroup of patients with stage II-III tumors were studied.
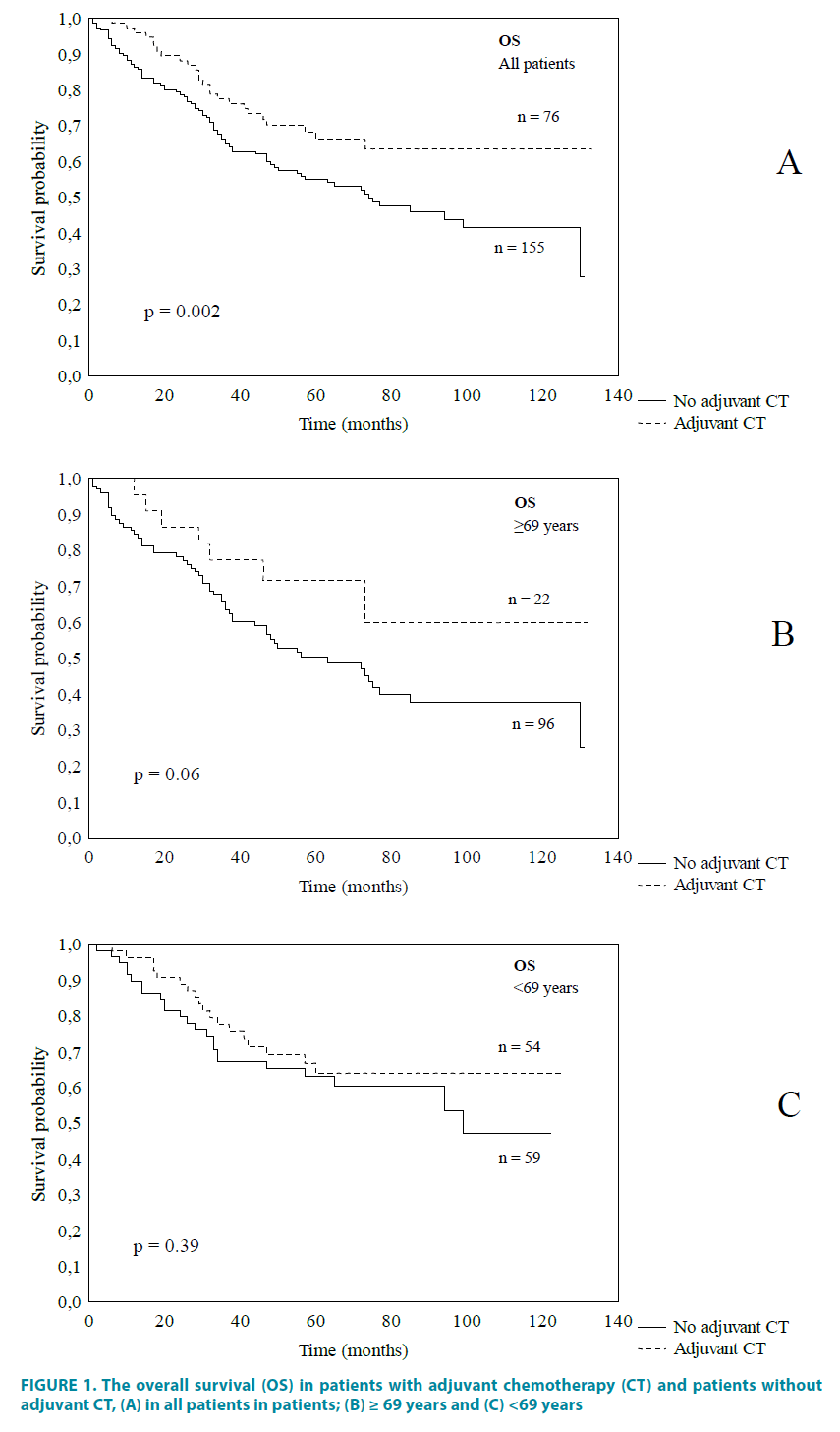
In the whole group of patients, patients with adjuvant CT had a better OS compared to the patients without adjuvant CT (p=0.002, FIGURE 1A), the significance still remained even after adjustment for sex, age, TNM stage, differentiation grade and preoperative RT (p=0.03, HR 0.57 95% CI 0.40-0.95). A trend towards significance was seen in patients ≥ 69 years (p=0.06, FIGURE 1B). No significant differences was found in the subgroup of patients <69 years (p=0.39, FIGURE 1C). No significant differences in CSS was found between patients with adjuvant CT and patients without adjuvant CT in the whole group of patients or in the subgroups of patients aged <69 or ≥ 69 years (p=0.15, p=0.64, p=0.26).
Figure 1: The overall survival (OS) in patients with adjuvant chemotherapy (CT) and patients without adjuvant CT, (A) in all patients in patients; (B) ≥ 69 years and (C) <69 years
In stage II-III tumors, there were no significant differences in the whole group of patients or in patients aged <69 or ≥ 69 years for both OS and CSS (p>0.05).
Adjuvant capecitabine in relation to survival
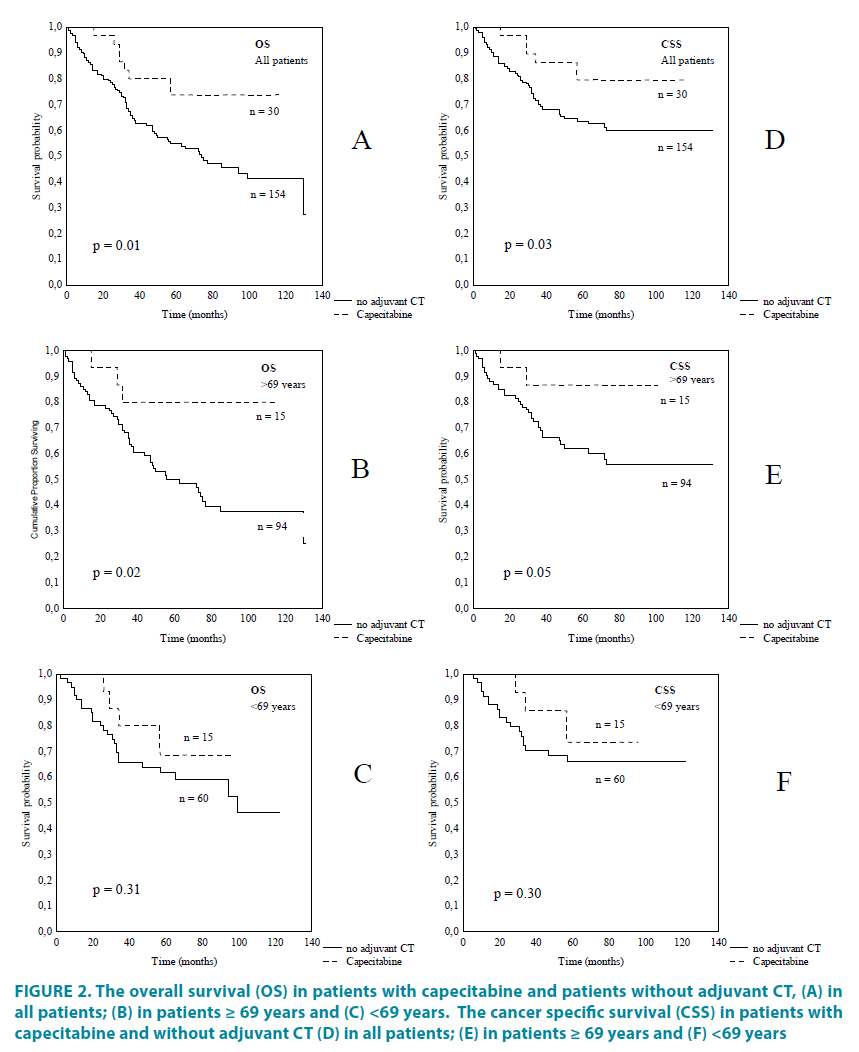
We further compare the survival between patients with capecitabine and the patients without adjuvant CT. In all patients and in patients ≥ 69 years, patients with capecitabine had a significantly better OS compared to patients without adjuvant CT (p=0.01, p=0.02, FIGURE 2A and 2B) independent of sex (age for the whole group), TNM stage, differentiation grade and preoperative RT (p= 0.003, HR 0.29, 95% CI 0.13-0.67, p=0.002, HR 0.13, 95% CI 0.04-0.49). There was no significance in the group of patients <69 years (p=0.31, FIGURE 2C). The same significant difference was found for the CSS where patients with adjuvant capecitabine had a better CSS compared to patients without adjuvant CT in all patients and in patients ≥ 69 years (p=0.03, p=0.05, after adjustment for sex (age for the whole group), TNM stage, differentiation grade and preoperative RT (p=0.006, HR 0.26, 95% CI 0.10-0.68, p=0.007, HR 0.13, 95% CI 0.03- 0.57, FIGURE 2D and 2E), but not in patients with the age of <69 years (p=0.30, FIGURE 2F). The distribution of the TNM stage for patients’ ≥ 69 years old, with and without adjuvant CT and with capecitabine alone are shown in TABLE 2.
Figure 2: The overall survival (OS) in patients with capecitabine and patients without adjuvant CT, (A) in all patients; (B) in patients ≥ 69 years and (C) <69 years. The cancer specific survival (CSS) in patients with capecitabine and without adjuvant CT (D) in all patients; (E) in patients ≥ 69 years and (F) <69 years
| Age ≥69 years |
No adjuvant CT n (%) |
Adjuvant CT n (%) |
Capecitabine n (%) |
Capecitabine /oxaliplatin n (%) |
|---|---|---|---|---|
| TNM stage IIA-IIB IIIA IIIB IIIC IV Total |
55 (57) 2 (2) 12 (13) 9 (9) 18 (19) 96 (100) |
3 (13) 1 (5) 7 (32) 10 (45) 1 (5) 22 (100) |
5 (17) 3 (10) 13 (43) 6 (20) 3 (10) 30 (100) |
1 (20) 0 1 (20) 3 (60) 0 5 (100) |
Table 2. TNM stage in patients ≥ 69 years old with or without adjuvant CT and in patients ≥ 69 with capecitabine and capecitabine/oxaliplatin
There were no significant differences found in OS or CSS in patients with stage II-III tumors in the whole group of patients or the subgroup of patients <69 years or ≥ 69 years old (p>0.05).
Adjuvant capecitabine/oxaliplatin in relation to survival
Further, the survival in patients with adjuvant capecitabine/oxaliplatin was compared with patient without adjuvant CT. No significant relationships were found in OS and CSS between patients with or without adjuvant capecitabine/oxaliplatin in all patients (p=0.42, p=0.98) or in patients aged ≥ 69 years (p=0.37, p=0.18) or <69 years (p=0.49, p=0.74).
In stage II-III tumors, the CSS was significantly reduced in patients ≥ 69 years with capecitabine/oxaliplatin compared to patients without adjuvant CT (p=0.04) and the significance remained even after adjustment for sex, differentiation grade and preoperative RT (p=0.03, HR 3.72, 95% CI 1.10-12.60). No significant differences were found in all patients or in the subgroup of patients <69 years (p=0.11, p=0.22). The TNM stage for patients’ ≥ 69 years old with capecitabine/oxaliplatin are shown in TABLE 2.
Comparison between adjuvant capecitabine and capecitabine/ oxaliplatin in relation to survival
The OS and CSS were further compared between patients with capecitabine and capecitabine/oxaliplatin. Patients ≥ 69 years with capecitabine had a significantly better CSS compared to patients with capecitabine/ oxaliplatin (p=0.02, no multivariate analysis was possible due to few cases, FIGURE 3A and 3B). In the whole group of patients a trend towards significance was seen (p=0.08, FIGURE 3A), but not in patients <69 years old (p=0.48, FIGURE 3C). For the OS, no statistical significance was found in all patients, in patients <69 and ≥ 69 years (p>0.05).
Figure 3: The cancer specific survival (CSS) in patients with capecitabine/oxaliplatin and in patients with capecitabine alone, (A) in the whole group; (B) in patients ≥ 69 years and (C) <69 years old.
In stage II-III tumours, a significantly better OS and CSS was seen in patients ≥ 69 years with capecitabine compared to capecitabine/ oxaliplatin (p=0.04, p=0.02, no multivariate analyze was possible due to few cases).
Side effects/compliance in RC patients with adjuvant CT
Next, the side effects in RC patients with adjuvant CT were analyzed. The most common side effect was neurotoxicity in the whole group of patients (32%) and in the subgroups of patients aged <69 (33%) and ≥69 (29%, TABLE 3). No significant differences were found in the number of side effects between the groups of patients aged <69 and ≥69 years (p=0.78, TABLE 3).
| Patients with adjuvant CT n=76 |
<69 years n (%) |
≥ 69 years n (%) |
All patients n (%) |
p-value |
|---|---|---|---|---|
| Side effects | ||||
| No | 19 (35) | 7 (32) | 26 (34) | 0. 78 |
| Yes | 35 (65) | 15 (68) | 50 (66) | |
| Type of side effects Neurotoxicity |
15 (33) | 5 (29) | 20 (32) | |
| Diarrhea | 3 (7) | 6 (35) | 9 (14) | |
| Hand foot syndrome | 7 (15) | 1 (6) | 8 (13) | |
| Neutropenia | 7 (15) | 1 (6) | 8 (13) | |
| Vomiting | 3 (7) | 0 | 3 (5) | |
| Allergic reaction | 3 (7) | 0 | 3 (5) | |
| High performance status (WHO >2) | 2 (4) | 1 (6) | 3 (5) | |
| Kidney toxicity | 2 (4) | 0 | 2 (3) | |
| Pancytopenia | 1 (2) | 1 (6) | 2 (3) | |
| Thrombocytopenia | 1 (2) | 1 (6) | 2 (3) | |
| Liver toxicity | 1 (2) | 1 (6) | 2 (3) | |
| Skin infection | 1 (2) | 0 | 1 (1) | |
| Total | 46 (100) | 17 (100) | 63* (100) | |
| Compliance n= 76 |
<69 years n (%) |
≥ 69 years n (%) |
All patients n (%) |
p-value |
| No dose modification | 20 (37) | 8 (36) | 28 (37) | |
| Dose reduction | 15 (28) | 7 (32) | 22 (29) | 0.58 |
| Dose interruption | 19 (35) | 7 (32) | 26 (34) | |
| Total | 54 (100) | 22 (100) | 76 (100) |
Table 3. Side effects and compliance of adjuvant CT in patients with RC in relation to age.
The patient’s compliance in relation to adjuvant CT was further investigated. Of the 76 patients with adjuvant CT, 28 (37%) patients completed all the treatments without dose reduction. Twenty-six (34%) patients had to stop the treatment due to severe side effects (TABLE 3).
Side effects/compliance in RC patients with adjuvant capecitabine and capecitabine/oxaliplatin
Further, the side effects in RC patients with adjuvant capecitabine and capecitabine/ oxaliplatin were investigated. Compared to capecitabine alone, patients with capecitabine/ oxaliplatin had a higher frequency of neurotoxicity (73% vs. 17%), diarrhea (63% vs. 37%) and neutropenia/pancytopenia (80% vs. 0%). Capecitabine had a higher rate of hand foot syndrome compared to capecitabine/ oxaliplatin (89% vs. 11%, TABLE 4).
| Type of adjuvant CT | Capecitabine n (%) |
Capecitabine/oxaliplatin n (%) |
Other treatments n (%) |
Total n (%) |
|||
|---|---|---|---|---|---|---|---|
| Age (years) Side effects | <69 | ≥69 | <69 | ≥69 | <69 | ≥69 | |
| Neurotoxicity | 1(6) | 2 (11) | 10 (56) | 3 (17) | 4 (22) | 0 | 18 (100) |
| Hand foot syndrome | 2 (22) | 6 (67) | 1 (11) | 0 | 0 | 0 | 9 (100) |
| Diarrhea | 2 (25) | 1 (12) | 5 (63) | 0 | 0 | 0 | 8 (100) |
| Neutropenia/pancytopenia | 0 | 0 | 5 (55) | 2 (25) | 2 (25) | 0 | 9 (100) |
| Age (years) Compliance | <69 | ≥69 | <69 | ≥69 | <69 | ≥69 | |
| No dose modification | 11 (73) | 5 (33) | 5 (19) | 1 (25) | 4 (29) | 2 (100) | |
| Dose reduction | 3 (20) | 6 (40) | 6 (23) | 1 (25) | 6 (42) | 0 | |
| Interruption | 1 (7) | 4 (27) | 15 (58) | 2 (50) | 4 (29) | 0 | |
| 15 (100) | 15 (100) | 26 (100) | 4 (100) | 14 (100) | 2 (100) | ||
Table 4. Side effects and compliance in patients with RC <69 or ≥ 69 years old with adjuvant capecitabine and capecitabine/oxaliplatin.
Fifty seven percent (n=17) of the patients with capectiabine/oxaliplatin and 17% (n=5) with capecitabine alone had to stop the treatment due to severe side effects. Sixty five percent (n=17) of the patients who had to stop the treatment due to severe side effects received capecitabine/ oxaliplatin and 19% (n=5) single capecitabine. Of the patients with no dose modification, 62% (n=16) received capecitabine and 23% (n=6) capecitabine/oxaliplatin (TABLE 4).
Discussion
In this study, we showed that 5-Fu based postoperative CT was related to improved OS patients with RC with preoperative RT or CRT. Our results are in line with two previous metaanalyses of patients with RC treated with either preoperative RT or CRT. In these studies it was shown that 5-Fu based postoperative CT was associated with improved survival compared to the patients who went through surgery alone [7,8]. Even though these two large meta-analyses showed significantly positive results, the role of postoperative CT in RC patients is still not yet clear. In the meta-analysis by [7] only 5 out 21 trials showed significantly positive results for patients with adjuvant CT compared to patients without CT. Many studies were conducted on a Japanese population treated with Uracil-Tegafur, and the postoperative adjuvant CT was only found beneficial in older studies not employing TME surgery [7]. In the meta-analysis by [8] patients were significantly younger than average and the follow up time was less than 5 years which were suggested to affect the benefit of OS [8]. The weaknesses of our study are that it is a small study based on a retrospective material and the material is taken from patients with real life experience with no randomization. Our result is in line with the previous large meta-analyses, but since this material is relatively small it is difficult to draw any firm conclusions.
The cornerstone of adjuvant CT in RC is fluoropyrymidine containing agents such a 5-Fu administrated either by continuous intravenous infusion or by bolus. It was shown in CC studies that patients with adjuvant 5-Fu and levamisole had a better survival compared to patients with surgery alone [4] and that the use of capecitabine administered orally was equally effective compared to bolus 5-Fu/leucovorin [5]. The main adjuvant treatment today in CRC patients is capecitabine as monotherapy or capecitabine in combination with oxaliplatin. In our study where only patients with RC were included, 42% of the patients received capecitabine and 38% the combination of capecitabine/oxaliplatin as adjuvant CT. Since most of the adjuvant CT consisted of capecitabine or the combination of capecitabine/oxaliplatin we further wanted to investigate the survival relationships between patients with capecitabine or capecitabine/ oxaliplatin, and patients without adjuvant CT.
Here, we showed that both the OS and CSS were significantly increased in the whole group of patients with adjuvant capecitabine compared to patients without adjuvant treatment. The significance still remained even after adjusting for sex, age, differentiation, preoperative RT and neoadjuvant CT. Interestingly, the same significant relationship was found in patient’s ≥ 69 years, where capacitabine improved the OS and CSS independent of sex, differentiation, preoperative RT and neoadjuvant CT. No significant difference was found in patients less than 69 years. In previous reports, it has been shown that patients above 70 years have been underrepresented in clinical trials [11]. The reason for that decision has been that elderly patients’ body has different physiology, with increased fat content and chronic organ insufficiency and that elderly patients more often have other diseases and multiple medications which may interact with the CT. A recent study on CC patients showed that the survival benefit with adjuvant 5-Fu did not diminish with patients’ age [14] and that patients with stage III CRC with the age of ≥ 75 years had a survival benefit with 5-Fu based regimes [13]. The previous studies on elderly patients have included patients with either CC or CRC. As far as we know, this is the first study on a pure RC material that shows that postoperative adjuvant capecitabine is related to improved OS and CSS in patients with RC ≥ 69 years. Unfortunately, there were no significant differences in the subgroup analyses of stage IIIII tumors which might be caused by too few cases in this material. A larger randomized study of patients with RC and adjuvant CT would be beneficial to further investigate this relationship.
The addition of oxaliplatin to 5-Fu based regimes has been shown to prolong the DFS and improve the OS in CRC patients with stage II-III tumors [6,15]. Here in this study, there were no significant differences in OS or CSS between patients with adjuvant capecitabine/ oxaliplatin and patients without adjuvant CT, in the whole group of patients and in subgroups of patients more or less than 69 years old. Interestingly, in stage II-III tumors, the CSS survival was significantly reduced in patients ≥ 69 years with capecitabine/oxaliplatin compared to patients without adjuvant CT and the significance still remained even after adjustment for sex, differentiation, preoperative RT and neoadjuvant CT. No significant relationship was found in the subgroup of patients aged <69 years. This result makes us suggest that the addition of oxaliplatin to 5-Fu based regimes does not improve the outcome, especially in elderly patients with RC.
Few have analyzed the differences in survival between capecitabine and capectabine/ oxaliplatin in elderly CRC patients. One previous study on elderly CC patients showed that the addition of oxaliplatin to 5-Fu was equally efficient compared to 5-Fu as monotherapy [13]. Here, we showed that patients ≥ 69 years had a significantly better CSS with capecitabine alone compared to capecitabine in combination with oxaliplatin. The same result were found in the subgroup of stage II-III tumors, where a significantly better OS and CSS was seen in patients ≥ 69 years with capecitabine compared to capecitabine/oxaliplatin. Unfortunately, no multivariate analysis was able to perform due to few cases. This result together with our previous findings strengthens the theory that capectabine alone is a good adjuvant treatment for patients ≥ 69 years old. However, more studies on a larger cohort of patients are needed to confirm this relationship.
We also showed that, only 37% of the patients <69 and 36% the patient’s ≥ 69 years were able to complete all CT cycles without dose reduction or treatment interruption. Thirty-four percent (34%) of the patients had to interrupt the adjuvant treatment due to severe side effects (CTCA>2). Our results shows a slight higher frequency of side effects compared to previous studies where 41-42% of the patients with RC with preoperative RT/ CRT managed to complete all the adjuvant CT cycles [9]. The reason for that could be that the patient’s performance status was higher in our study compared to the previous trials (WHO 0-1) where a more selected group of patients with a better performance status received the treatment.
In the patients with capecitabine/oxaliplatin only 43% of the patients with capecitabine/ oxaliplatin managed to complete the treatment without dose reduction or interruption. This result is in line with one previous study, where 48% completed six cycles of treatment [16]. Even though it is few patients, it is worth to note that 57% of the patients in our study had to interrupt the treatment with capecitabine/ oxaliplatin. In patients with capecitabine, 17% had to stop the treatment due to severe side effects and 33% were able to complete the treatment after dose modification. The same results were found by others where 17% of the patients with capecitabine had to interrupt the treatment due to severe side effects and 43% needed a dose modification [5]. We also showed that 63% of the patients with treatment interruption received capecitabine/oxaliplatin and 19% single capecitabine. Of the patients with no dose modification, 57% received capecitabine and 21% capecitabine/ oxaliplatin Oxaliplatin based regimes gives a high frequency of treatment interruptions due to severe side effects compared to single capectiabine.
Finally, the side effects were studied in patients with adjuvant CT. The most common side effect in the whole group of patients was neurotoxicity (32%), diarrhea (14%), hand foot syndrome (13%) and neutropenia (13%). In the patients with capecitabine/oxaliplatin compared to patients with capecitabine a higher frequency of neurotoxicity 73% vs. 17%, diarrhea 63% vs. 37% and neutropenia/ pancytopenia 80% vs. 0% was seen. Our result shows that treatment with oxaliplatin in combination with capectiabine has a higher frequency of severe side effects compared to treatment with capecitabine alone.
Conclusions
Capecitabine as a monotherapy given postoperatively contribute to better OS and CSS in RC patients’ ≥69 years. Considering the high prevalence of side effects and no survival benefit, the oxaliplatin containing regimen should be administered with caution, especially for elderly patients. In order to confirm these relationships, more studies on a larger cohort of patients are needed.
Acknowledgements
The authors would like to thank Professor Xiao-Feng Sun, Department of Oncology, Linköping, Sweden, for her great support during this project. This study was supported by grants from the foundation of Oncological Clinical Research in Linköping, the Swedish Cancer Foundation, Swedish Research Council and the Health Research Council in the South- East of Sweden.
Competing interests
The authors declare no conflicts of interest or funding sources that could be perceived as a conflict of interest.
References
- Tamas K, Walenkamp AM, de Vries EG, et al. Rectal and colon cancer: Not just a different anatomic site. Cancer Treat.Rev. 41(8), 671-679 (2015).
- Fransen K, Klintenas M, Osterstrom A, et al. Mutation analysis of the BRAF, ARAF and RAF-1 genes in human colorectal adenocarcinomas. Carcinogenesis.25(4), 527-533 (2004).
- Birkenkamp-Demtroder K, Olesen SH, Sorensen FB, et al. Differential gene expression in colon cancer of the caecum versus the sigmoid and rectosigmoid. Gut.54(3), 374-384 (2005).
- Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N. Engl. J. Med.322(6), 352-358 (1990).
- Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N. Engl. J. Med. 352(26), 2696-2704 (2005).
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J. Clin. Oncol.29(11), 1465-1471 (2011).
- Petersen SH, Harling H, Kirkeby LT, et al. Postoperative adjuvant chemotherapy in rectal cancer operated for cure. Cochrane Database Syst. Rev. 3, CD004078 (2012).
- Petrelli F, Coinu A, Lonati V, Barni S. A systematic review and meta-analysis of adjuvant chemotherapy after neoadjuvant treatment and surgery for rectal cancer.Int. J. Colorectal Dis. 30(4), 447-457 (2015).
- Bosset JF, Calais G, Mineur L, et al. Fluorouracil-based adjuvant chemotherapy after preoperative chemoradiotherapy in rectal cancer: long-term results of the EORTC 22921 randomised study. Lancet Oncol.15(2), 184-190 (2014).
- Hutchins LF, Unger JM, Crowley JJ, et al. Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N. Engl. J. Med.341(27), 2061-2067 (1999).
- Zulman DM, Sussman JB, Chen X, et al. Examining the evidence: a systematic review of the inclusion and analysis of older adults in randomized controlled trials. J. Gen. Intern. Med. 26(7), 783-790 (2011).
- Kim JH. Chemotherapy for colorectal cancer in the elderly.World J. Gastroenterol.21(17), 5158-5166 (2015).
- Sanoff HK, Carpenter WR, Sturmer T, et al. Effect of adjuvant chemotherapy on survival of patients with stage III colon cancer diagnosed after age 75 years. J. Clin. Oncol.30(21), 2624-2634 (2012).
- Iwashyna TJ, Lamont EB. Effectiveness of adjuvant fluorouracil in clinical practice: a population-based cohort study of elderly patients with stage III colon cancer. J. Clin. Oncol.20(19), 3992-3998 (2002).
- Andre T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J. Clin. Oncol.27(19), 3109-3116 (2009).
- Glynne-Jones R, Counsell N, Quirke P, et al. Chronicle: results of a randomised phase III trial in locally advanced rectal cancer after neoadjuvantchemoradiationrandomising postoperative adjuvant capecitabine plus oxaliplatin (XELOX) versus control. Ann. Oncol. 25(7), 1356-13562 (2014).