Research Article - Interventional Cardiology (2020) Volume 12, Issue 2
A Comparative Study between the Routine Using of Ultrasound Guidance versus Anatomical Guidance in Femoral Artery Access for Endovascular Treatment of Chronic Lower Limb Ischemia
- Corresponding Author:
- Mina Ragaa Fekry Abdelmalak
Department of General and Vascular Surgery,
Faculty of Medicine,
Beni-Suef University,
Egypt
E-mail: mina_abdelmalak92@yahoo.com
Received date: March 11, 2020 ; Accepted date: March 20, 2020; Published date: March 27, 2020
Abstract
The goal of this study is comparison between the using of ultrasound guidance versus anatomical guidance in femoral artery access for endovascular treatment of chronic lower limb ischemia, by assessment of first pass success rate, total number of attempts required for access, rate of accidental venipunctures, rate of PFA puncture and time to sheath insertion, and assessment of post procedural puncture site complications defined as bruises or hematoma formation.
The study found that US guidance is superior to anatomical guidance in femoral artery access in endovascular treatment of chronic lower limb ischemia in reducing access time, total number of punctures, and number of incidental venipuncture, the incidence of PFA access and incidence of local bruises.
Keywords
US guidance; Endovascular; Femoral artery access; Anatomical access.
Introduction
Chronic lower-extremity ischemia is considered one of the common causes of morbidity and mortality. The vast majority of patients usually are presented with intermittent claudication; a term refers to pain in the leg muscles after activity, or ischemic rest pain that affects the foot and leads to ulceration as well as severe tissue loss later on. In fact, the incidence of chronic lower-extremity ischemia is likely to increase as a result of increasing the percentage of elderly people. In the developed countries, peripheral arterial disease (PAD) is common influencing about 14-20% of the adult population, with a ratio between symptomatic and asymptomatic patients of 1:3 to 1:4 [1].
The first option for treating infrainguinal PAD is usually endovascular treatment as percutaneous transluminal angioplasty (PTA) with adjunctive stenting that has become increasingly used and accepted approach frequently employed for infrainguinal endovascular treatment [2]. The traditional access procedure includes the use of palpation, anatomic landmarks, fluoroscopic guidance or combinations of these maneuvers in order to reach an arterial access [3]. Access site complications such as hematoma, venipuncture, pseudoaneurysm, and arteriovenous fistula, are the major cause of post procedural morbidity &mortality in individuals undergoing percutaneous vascular interventions (PVI) with longer hospital stays, elevated rates of discharge to rehabilitation/nursing facilities, increased 30-day mortality, and increased one year mortality [4]. In the last decades, US guidance has been widely used for central venous access. In several randomized trials, real time US guidance has been proved to decrease complications, number of trials, and time to access in central venous cannulation [5].
The traditional access procedure includes the use of palpation, anatomic landmarks, fluoroscopic guidance or combinations of these maneuvers in order to reach an arterial access, despite using fluoroscopic guidance seems to be promising in decreasing the complications of access site, randomized trials have not detect the superiority of this maneuver in comparison with the anatomical landmark guidance [3]. On the contrary, the use of ultrasound guidance (UG) has been proved to improve 1st pass success rate and reduce access site complications after common femoral artery access in comparison with the anatomical landmark guidance with and without fluoroscopy [6]. Access complications are accompanied by female gender, extremes of weight, renal insufficiency, and the use of anticoagulant or glycoprotein IIb/IIIa inhibitors. Several retrospective studies have accompanied inappropriate puncture sites with a high risk of complications [7].
Patients and Methods
The study is prospective, randomized trial involving 20 patients with chronic lower limbs arterial diseases .The study is conducted in vascular surgery unit of Beni-Suef University Hospital. Patients were submitted to percutaneous transluminal angioplasty through common femoral artery access. The patients were divided into 2 groups:
Group (1): Ten patients with femoral artery access through the using of anatomical guidance.
Group (2): Ten patients with femoral artery access through the using of US guidance.
Inclusion criteria:
1. Patients with a diagnosis of chronic occlusive or stenotic lower limb arterial disease and considered for interventional angioplasty.
2. Both males and females.
All patients were subjected to:
A. Pre-procedural Preparation:
1-History taking, clinical examination, duplex scanning and CT Angiography.
B. Steps of the procedure
In group A: After being draped, all patients received manual palpation of anatomic landmarks: the anterior superior iliac spine, pubic symphysis, and the femoral pulse. Puncture were made over the femoral pulse until a jet of arterial blood was noted followed by passing of a 0.35fr guide wire and 6fr sheath then an angiogram was made in order to confirm the position of the guide wire and the sheath.
In group B: the US machine was set up and draped, with transmission gel applied. The US imaging was performed in the axial plane. The modified Seldinger technique was intended to be used in all cases.
• Post-interventional surveillance: follow up of the patient so as to evaluate immediate, early or late complications in femoral artery access site within thirty days of the procedure.
• 1ry end point: Successful cannulation of common femoral artery.
• 2ry end point: 1st pass success rate, total number of trials needed for access, rate of accidental venipunctures, rate of accidental PFA access and time to sheath insertion. Post procedural puncture site complications defined as hematoma of 5 cm or more, formation of pseudoaneurysm, retroperitoneal hemorrhage, drop of hemoglobin to 3 g/dl or more with an access source or ≥ 4 g/dl with an unknown source.
Statistical methodology
Femoral angiograms were reviewed for proper CFA placement. Angiograms were analyzed for the position of the sheath, CFA bifurcation, and origin and most inferior reflection of the inferior epigastric artery relative to the femoral head Collected data were analyzed on an intention-to-treat basis. The unpaired Student’s t test or Wilcoxon rank sum test were used for continuous variables and the chi-square test was used for proportions. The Fisher’s exact test was used for clinical outcomes. A 2-tailed p value of 0.05 was used for significance Table 1.
Results
This is a prospective, randomized, single-blinded trial involving patients with chronic lower limbs arterial ischemia. The study was conducted on 20 patients diagnosed as chronic occlusive or stenotic lower limb arterial diseases and considered for interventional angioplasty. The studied cases were randomly allocated into two groups according to the method of femoral artery access for endovascular treatment of chronic lower limb ischemia Table 2:
Group (1): Ten patients with femoral artery access through the using of an anatomical guidance.
Group (2): Ten patients with femoral artery access through the using of ultrasound guidance.The Patients’ age ranged from (49) to (69) with an average age of (59.35 ± 5.7) years old.
| Patients according to access method | Total | p-value | ||
|---|---|---|---|---|
| Anatomical Guidance | US Guidance | |||
| N=10 | N=10 | |||
| Rt. SFA | 2 (20) | 4 (40) | 6 (30) | 0.721 |
| Lt. SFA | 4 (40) | 2 (20) | 6 (30) | |
| Rt. Infra-popliteal | 2 (20) | 2 (20) | 4 (20) | |
| Lt. Infra-popliteal | 2 (20) | 2 (20) | 4 (20) | |
Table 1: Lesion Site among studied population.
| Patients according to access method | Total | p-value | ||
|---|---|---|---|---|
| Anatomical Guidance | US Guidance | |||
| N=10 | N=10 | |||
| Antegrade Ipsilateral | 6 (60) | 9 (90) | 15 (75) | 0.152 |
| Contralateral Retrograde | 4 (40) | 1 (10) | 5 (25) | |
Table 2: Intra-Operative access to femoral artery.
The intraoperative time needed to access the femoral artery was significantly shorter among studied patients who have undergone femoral artery access through uses of ultrasound guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average time in minutes was (2.19 vs. 4.22) in US guidance and anatomical guidance respectively; (p-value=0.007) Table 3.
| Patients according to access method | Total | p-value | ||
|---|---|---|---|---|
| Anatomical Guidance | US Guidance | |||
| N=10 | N=10 | |||
| Mean ± SD | 4.22 ± 1.7 | 2.19 ± 1.1 | 59.35 ± 5.7 | 0.007* |
| Minimum | 1.08 | 0.83 | 49 | |
| Maximum | 7.67 | 4.5 | 65 | |
Table 3: Comparison of time in minuets to access the femoral artery among the studied patients.
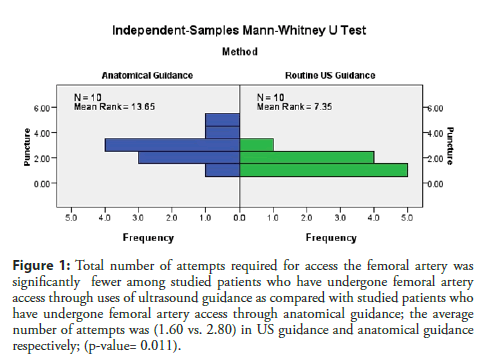
Total number of attempts required for access the femoral artery was significantly fewer among studied patients who have undergone femoral artery access through uses of ultrasound guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average number of attempts was (1.60 vs. 2.80) in US guidance and anatomical guidance respectively;(p-value=0.011) Table (4) Figure 1.
| Patients according to access method | Total | p-value | ||
|---|---|---|---|---|
| Anatomical Guidance | US Guidance | |||
| N=10 | N=10 | |||
| No accidental veni-punctures | 3 (30) | 10 (100) | 13 (65) | 0.013* |
| 1 time | 4 (40) | 0 (0.00) | 4 (20) | |
| 2 times | 2 (20) | 0 (0.00) | 2 (10) | |
| 3 times | 1 (10) | 0 (0.00) | 1 (5) | |
Table 4: Comparison of rate of accidental venipunctures among the studied patients:
All the studied patients who have undergone femoral artery access through the using of ultrasound guidance had no accidental venipunctures in the present study with a statistically significant difference as compared with the anatomical guidance; (p-value=0.013). On the other hand; no accidental venipunctures occurred only in 3 cases (30%) among patients who have undergone femoral artery access through anatomical guidance, 4 cases (40%) had accidental veni-punctures one time, 2 cases (20%) had accidental venipunctures two times, and only one case had accidental veni-punctures three times Table 5 and Table 6.
Discussion
Chronic lower-extremity ischemia is one of the commonest causes of morbidity and mortality, Endovascular treatment is usually the 1st choice for treatment of infrainguinal PAD, Percutaneous transluminal angioplasty (PTA) with adjunctive stenting is a widely used and accepted procedure, and it is the procedure most frequently employed for infrainguinal endovascular treatment [2]. Complications of access site such as hematoma, pseudoaneurysm, venipuncture and AV fistula, are considered a major source of post procedural morbidity and mortality in patients undergoing PVI [4].
In this study, we compared the anatomical guidance versus the US guidance in femoral artery access as regard the number of total trial to successfully cannulate CFA defined as mid-way between the origin of inferior epigastric vessels and bifurcation into SFA&PFA, the time needed for the access, the number of venipunctures, the number of PFA punctures and the rate of bruises and hematoma formation in 20 patients divided into 2 groups. The past randomized multicenter studies detected that routine US guidance of femoral arterial access doesn’t achieve improvement of the rate of CFA successful cannulation except in patients with high CFA bifurcations, otherwise it results in time wasting with no significant difference; besides, and it needs the availability of US devices and specific training in each center.
Based on our study findings, US guidance decreased the risk of vascular access complications, improved the 1st pass success rate and approximately eliminated accidental venipunctures, whereas decreasing the time required for access and demonstrated an increased CFA successful cannulation rate in the patients with a CFA bifurcation occur higher than the inferior border of the femoral head. This subgroup of patients can’t be usually detected before catheterization in the absence of previous angiogram data.
The intraoperative time required for accessing the femoral artery was significantly shorter among studied patients who have undergone femoral artery access through uses of US guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average time in minutes was (2.19 vs. 4.22) in US guidance and anatomical guidance respectively; (p-value=0.007). Arnold Seto et al., [8] in 2016 concluded that US guidance leads to an improved 1st pass success rate (83% vs. 46%, p<0.0001). Abu Fadel et al, [9] in 2009 found that US guidance decreased the number of trials to successfully cannulate CFA (1.3 vs. 3.0, p<0.0001).
In our study the total number of attempts needed for access the femoral artery was significantly fewer among studied patients who have undergone femoral artery access through uses of US guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average number of attempts was (1.60 vs. 2.80) in US guidance and anatomical guidance respectively; (p-value=0.011). A systematic review of 4 trials with a total of 1422 subjects who underwent femoral artery catheterization revealed 42% improvement in likelihood of 1st-attempt success and 49% decrease in overall access site complications with the use of UG in comparison with traditional palpation approaches.
Figure 1: Total number of attempts required for access the femoral artery was significantly fewer among studied patients who have undergone femoral artery access through uses of ultrasound guidance as compared with studied patients who have undergone femoral artery access through anatomical guidance; the average number of attempts was (1.60 vs. 2.80) in US guidance and anatomical guidance respectively; (p-value= 0.011).
All the studied patients who have undergone femoral artery access through the using of US guidance had no accidental venipunctures in the present study with a statistically significant difference in comparison with the anatomical guidance; (p-value=0.013). On the other hand; no accidental venipunctures occurred only in 3 cases (30%) among patients who have undergone femoral artery access through anatomical guidance, 4 cases (40%) had accidental venipunctures one time, 2 cases (20%) had accidental venipunctures two times, and only one case had accidental venipunctures three times.
| Patients according to access method | Total | p-value | ||
|---|---|---|---|---|
| Anatomical Guidance | US Guidance | |||
| N=10 | N=10 | |||
| No | 7 (70) | 10 (100) | 17 (80) | 0.105 |
| Yes | 3 (30) | 0 (0.00) | 4 (20) | |
Table 5: PFA Puncture among Studied Cases
| Patients according to access method | Total | p-value | ||
|---|---|---|---|---|
| Anatomical Guidance | US Guidance | |||
| N=10 | N=10 | |||
| No | 7 (70) | 9 (90) | 17 (80) | 0.291 |
| Yes | 3 (30) | 1 (10) | 4 (20) | |
Table 6: Post-Operative Bruises among Studied Cases:
The occurrence of post-operative bruises was higher among the group of anatomical guided access rather than the US Guidance group; (p-value=0.291). Three cases (30%) in anatomical guidance access method had post-operative bruises in opposite to one case (10%) among US guidance access method. Inagaki et al. in a study published in Annals of Vascular Surgery in 2018 [10], reported that US guidance was protective against bruises and hematoma formation amongst high-volume of procedures (p=0.030).
The clinical benefit of US guidance is most likely mediated by a decrease in tissue and vessel trauma caused by multiple attempts and venipunctures. Also, US guidance is more likely to achieve a true anterior wall puncture that may permit better arterial wall apposition and more appropriate seating of the introductory sheath. Anatomical guidance in femoral artery access may decrease its caliber, elevating the risk of a posterior or double wall puncture. With US guidance, any compression of the artery is both minimized and made visible during the procedure, potentially reducing the risk of a posterior wall puncture.
Conclusion and Recommendations
Routine US guided femoral artery access was found to be superior to anatomical guided femoral access and improved CFA cannulation by decreasing the number of trials, time to access, risk of venipunctures, PFA puncture and local vascular complications as bruises and hematoma formation in femoral arterial access in endovascular treatment of chronic lower limb ischemia. To this end, clinicians should make every attempt to acquire the technical skills that will help them employing US support routinely during vascular access procedures. At least 10 UG vascular access procedures are recommended to be supervised in order to determine demonstrate competency
References
- Ellis SG, Bhatt D, Kapadia S, et al. Correlates and outcomes of retroperitoneal hemorrhage complication percutaneous vascular intervention. Catheter Cardio Inte. 67(4): 541-545 (2007).
- Adams J, Harold P. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 115(20): e478-e534 (2007).
- Johnston KW. Errors and artifacts of carotid ultrasound evaluation. In: AbuRahma AF, Bandyk DF, eds. Noninvasive Vascular Diagnosis: A Practical Guide to Therapy. ed 3. New York: Springer. 2: 25-27 (2013).
- Ortiz D, Jahangir A, Singh M, et al. Access site complications after peripheral vascular interventions: incidence, predictors, and outcomes. Circ Cardiovasc Interv. 7(6): 821-828 (2014).
- Le I. Ferrières R, Guinier D. Ultrasound guidance of central venous catheterisation. J Surg. 146(6): 528-531 (2009).
- Sobolev M, Slovut DP, Lee Chang A, et al. Ultrasound-guided catheterization of the femoral artery: a systematic review and meta-analysis of randomized controlled trials. J Invasive Cardiol. 27: 318-23 (2015).
- Turi, Zoltan G. Vascular access and closure. Cardiovascular Catheterization and Intervention: A Textbook of Coronary, Peripheral, and Structural Heart Disease. 67 (2010).
- Seto AH, Kern MJ. Transulnar catheterization: The road less traveled. Catheter Cardio Inte. 87(5): 866-867 (2016).
- Abu-Fadel MS, Sparling JM, Zacharias SJ, et al. Fluoroscopy vs. 1 traditional guided femoral arterial access and the use of closure devices: a randomized controlled trial. Catheter Cardiovasc Interv. 74(4): 533-539 (2009).
- Inagaki E, Farber A, Siracuse JJ, et al. Routine use of ultrasound guidance in femoral arterial access for peripheral vascular intervention decreases groin hematoma rates in high-volume surgeons. Ann Vasc Surg. 51: 1-7 (2018).