Research Article - Diabetes Management (2022) Volume 12, Issue 2
A cross-sectional investigation of cognitive impairment in type 2 diabetes mellitus patients with chronic periodontitis
- Corresponding Author:
- Arthi Balasubramaniam
Department of Community Dentistry,
Saveetha Dental College & Hospital,
Chennai,
India
E-mail: arthi.bds@gmail.com
Received: 01-Feb-2022, Manuscript No. FMDM-22-4741 ; Editor assigned: 03-Feb-2022, PreQC No. FMDM-22-4741 (PQ); Reviewed: 21-Feb-2022, QC No. FMDM-22-4741 ; Revised: 25-Feb-2022, Manuscript No. FMDM-22-4741 (R); Published: 04-Mar-2022, DOI: 10.37532/1758-1907.2022.12(2).321-328
Abstract
Background: Cognitive impairment is the condition where there is expected cognitive
decline of normal aging. It is characterized by difficulties with memory, language, thinking and
judgment. Type 2 diabetes mellitus is an important risk factor for cognitive impairment and
periodontitis. The chronic effects of both periodontitis and diabetes may have an uncontrollable
additive effect on the body and a greater risk for developing neurodegeneration associated
with dementia. The aim of this study is to evaluate the cognitive impairment in patients with
type 2 diabetes mellitus and chronic periodontitis.
Methods: A total of 70 subjects in the age group of 40 to 60 years which included diabetic
individuals with and without chronic periodontitis. Community screening instrument for
dementia (CSI-D) was used for assessing the cognitive impairment of the patients. Data
obtained were compiled systematically in Microsoft Excel spreadsheet. Pearson Chi-square
test and Pearson correlation test was performed for the statistical analysis. P value<0.05 was
considered to be statistically significant.
Results: The results showed that there are a significant number of diabetic individuals with
chronic periodontitis having possible chances of developing cognitive impairment. It has also
been shown that possible chances of cognitive impairment were higher in males among the
age group of 56 to 60 years.
Conclusion: The clinical implication of these findings helps in modifying the lifestyle of elderly
diabetic population who are at a risk for the development of dementia.
Keywords
cognitive impairment; dementia; diabetes mellitus; innovative technique; periodontitis
Introduction
Cognitive impairment is a condition defined as cognitive decline greater than expected for an individual’s age and education level but that does not interfere notably with activities of daily life [1]. Its prevalence in epidemiological studies ranges from 3% to 19% in adults older than 65 years at the year of 2004 [2]. Some people with mild cognitive impairment seem to [3] remain stable or return to normal over time, but more than half progress to dementia within 5 years. The amnestic subtype of mild cognitive impairment has a high risk of progression to Alzheimer’s disease, and it could constitute a prodromal stage of this disorder [4]. Currently, there is no definitive cure for dementia, evolution of alternative modifying treatment approaches will be an imperative area of its research and it will require a more extensive understanding of the underlying neurodegenerative process responsible for the symptoms of dementia.
Recent reports show that peripheral infections, end vessel damage and oxidative stress may increase inflammation in the brain tissues and play an important role in the pathogenesis of dementia [5]. Previous studies have revealed that diabetes mellitus, hypertension, depression, traumatic brain injury and periodontal problems are associated with cognitive impairment [6– 9]. Diabetes mellitus is a complex metabolic disease that crosses the blood-brain barrier via specific receptors [10]. It can have devastating effects on organs in the body. The non-insulin dependent diabetes mellitus patients are at the risk of accelerated micro vascular disease which is pertinent to the pathogenesis of dementia. Levels of FPG, 2h-PG, HbA1c, and FPI are associated with risk of dementia. The peripheral microvascular complications in diabetes mellitus arising across the brain can be correlated to the neuropathic vascular changes in the brain leading to cognitive impairment [11].
Similarly, chronic periodontitis is a peripheral inflammatory condition that is among the leading risk factors for tooth loss. It is a common oral infection prevalent in older age groups. It has been associated with increase in serum levels of C-reactive protein and pro-inflammatory cytokines. Earlier studies have reported that this association between cognitive impairment and chronic periodontitis is due to the increase in systemic inflammation that accompanies the growth of periodontal pathogenic microorganisms. Systemic inflammation caused by periodontal pathogens can also play a major role in vascular disease and endothelial dysfunction. Researchers have proposed that periodontitis can lead to progression of AD by further increasing levels of pro-inflammatory cytokines and can lead to the invasion of microorganisms from the dental plaque biofilm into the brain.
The global burden of dementia, Type 2 diabetes mellitus, and periodontitis is rapidly increasing and has become a serious area of concern. Diabetes mellitus is a serious risk factor for dementia and it also shares a bidirectional relationship with periodontitis. Earlier studies have reported the link between cognitive impairment and diabetes mellitus and chronic periodontitis. Only few studies have reported the bidirectional relationship of cognitive impairment with diabetes mellitus and chronic periodontitis and hence this study was directed to know the relationship between these factors. The aim of this study is to evaluate the cognitive impairment in patients with type 2 diabetes mellitus and chronic periodontitis.
Methodology
Study setting
The present study was conducted as a retrospective cross sectional study to evaluate the cognitive impairment in patients with type 2 diabetes The present study was conducted as a retrospective cross sectional study to evaluate the cognitive impairment in patients with type 2 diabetes mellitus and chronic periodontitis visiting the dental hospital. A randomised sample of patients who had been reported for periodontitis treatment was chosen for the study. The study took place in a private college hospital setting within the university. The retrospective data was being ethically approved by the institution.
Sampling
A total of 70 patients out of which 35 with diabetes mellitus and chronic periodontitis and 35 with diabetes mellitus and without chronic periodontitis reported from the month of September 2020 to February 2021 were included for the study. The records of all patient data were reviewed from initial to last and were arranged in chronological order. All the blood sugar report data were properly reviewed and cross verified by another examiner. Sampling bias was minimized by simple random sampling. Internal validity is applicable to the study.
Procedure
The brief community screening instrument for dementia (CSI-D) was developed to promote case detection of possible dementia by primary care attendees. The full CSI-D cognitive test assessment includes cognitive assessment scale and informant interview scale. The sensitivity and specificity of this instrument was 97.3% and 90.5% with AUROC of 0.98, representing CSI-D, a good screening instrument for dementia. The overall score tells where the individual is normal, possible dementia and probable dementia. The score depends on cognitive assessment scale which includes seven items and informant interview includes six items. The seven cognitive test items were, in order of item difficulty which includes recall of three items (boat, house and fish) correctly describing the use of hammer, naming elbow, pointing to the window and then to the door, locating the nearest store, orientation to season, orientation to day of the week and delayed recall of three words. The six informant items were in order of item difficulty; often forgetting where she/he had put things, general decline in mention functioning, changes in ability to think and reason, sometimes forgetting what happened the day before, sometimes forgetting where she/ he is and any difficulty in dressing. Periodontal health assessment was carried out by the investigator. The bleeding was dichotomized as bleeding absent and bleeding present, similarly pocket status was dichotomized as pocket absent and pocket present, loss of attachment also was categorized as attachment loss present and attachment loss absent.
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences software (SPSS version 23, USA). Normality test was done using Kolmogorov numerical normality test. It was found that dependent variables were normally distributed. Depending upon the nature of the data, appropriate parametric and non-parametric statistical tests were chosen, p value of 0.05 was considered to be significant. Pearson Chi-square test and Pearson correlation test was performed to find the association and correlation between cognitive test and informant interview on dementia.
Results
The present cross sectional study was to assess the cognitive impairment status of diabetes mellitus patients with chronic periodontitis. The sample size of the study is 70 in the age group of 40 to 60 years. The statistical software SPSS was used for the descriptive and inferential analysis. Results on categorical measurement were presented in percentage (%). Level of significance was predetermined at the probability value of P ≤ 0.05 and any value ≤ 0.05 was considered to be statistically significant.
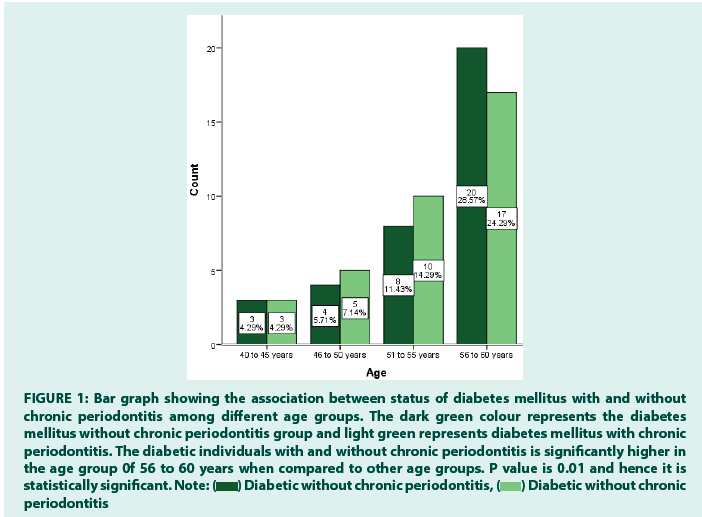
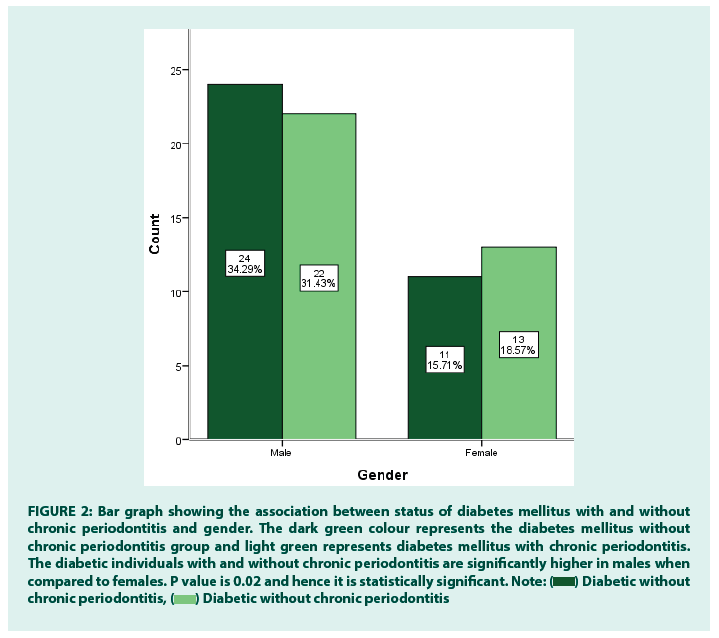
Diabetic patients without chronic periodontitis reported in the age group of 40 to 45 years include 4%, 5% in 46 to 50 years, 11% in 51 to 55 years and 28% in 56 to 60 years. In diabetes mellitus with chronic periodontitis patients, 4% reported in the age group of 40 to 45 years, 7% in the age group of 46 to 50 years, 14% in the age group of 51 to 55 years and 24% in the age group of 56 to 60 years (FIGURE 1). The gender distribution among diabetic individuals with and without chronic periodontitis shows that 34%, 31% males reported with diabetes without chronic periodontitis and diabetic with chronic periodontitis respectively. 15% females reported being diabetic without chronic periodontitis and 18% with diabetes and chronic periodontitis (FIGURE 2).
Figure 1: Bar graph showing the association between status of diabetes mellitus with and without chronic periodontitis among different age groups. The dark green colour represents the diabetes mellitus without chronic periodontitis group and light green represents diabetes mellitus with chronic periodontitis. The diabetic individuals with and without chronic periodontitis is significantly higher in the age group 0f 56 to 60 years when compared to other age groups. P value is 0.01 and hence it is statistically significant. 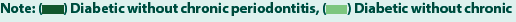

Figure 2: Bar graph showing the association between status of diabetes mellitus with and without chronic periodontitis and gender. The dark green colour represents the diabetes mellitus without chronic periodontitis group and light green represents diabetes mellitus with chronic periodontitis. The diabetic individuals with and without chronic periodontitis are significantly higher in males when compared to females. P value is 0.02 and hence it is statistically significant. 

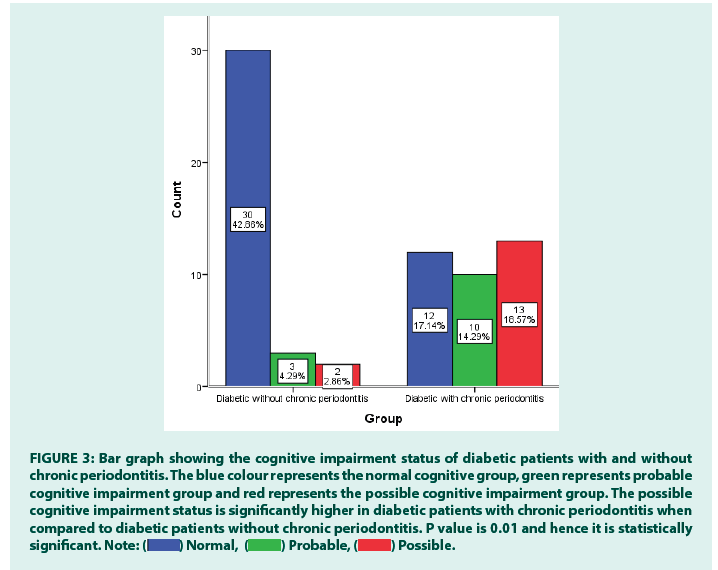
The cognitive impairment status among diabetic individuals shows that 42% of diabetic patients without chronic periodontitis have normal cognitive status and 17% of diabetic patients with chronic periodontitis have normal cognitive status whereas 4% of patients without periodontitis have probable cognitive impairment and 14% of diabetic patients with periodontitis have probable cognitive impairment. 3% of diabetic patients without periodontitis have possible cognitive impairment whereas 18% of diabetic individuals with chronic periodontitis have chances of cognitive impairment (FIGURE 3).
Figure 3: Bar graph showing the cognitive impairment status of diabetic patients with and without chronic periodontitis. The blue colour represents the normal cognitive group, green represents probable cognitive impairment group and red represents the possible cognitive impairment group. The possible cognitive impairment status is significantly higher in diabetic patients with chronic periodontitis when compared to diabetic patients without chronic periodontitis. P value is 0.01 and hence it is statistically significant. 
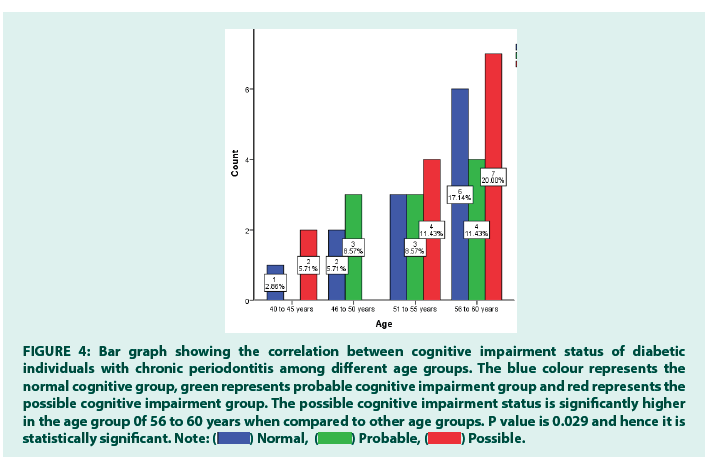
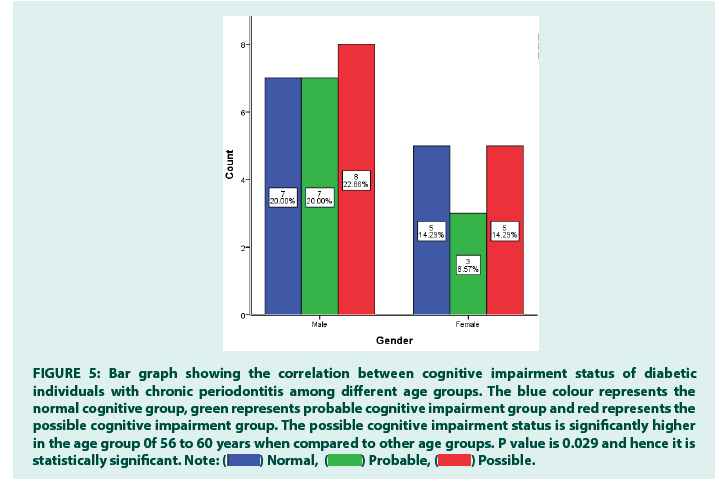
Similarly in the age group of 40 to 45 years, 2% patients have chances of normal cognitive impairment with diabetes mellitus and chronic periodontitis, 5% with possible chances of cognitive impairment. In the age group of 46 to 50 years, 5% patients had normal cognitive development, 8% patients had probable chances of cognitive impairment. In the age group of 51 to 55 years, 8% of patients had normal and probable cognitive impairment status. 11% had possible chances of cognitive impairment. In the age group of 56 to 60 years, 17% had normal cognitive status, 11% with probable cognitive impairment and 20% with possible cognitive impairment (FIGURE 4). The gender distribution among patients with cognitive impairment, type 2 diabetes mellitus and chronic periodontitis shows that 20% male patients have normal cognitive status, 20% probable cognitive impairment and 22% with possible cognitive impairment. Similarly, 14% females have normal cognitive impairment, 8% have probable cognitive impairment and 14% have possible cognitive impairment (FIGURE 5).
Figure 4: Bar graph showing the correlation between cognitive impairment status of diabetic individuals with chronic periodontitis among different age groups. The blue colour represents the normal cognitive group, green represents probable cognitive impairment group and red represents the possible cognitive impairment group. The possible cognitive impairment status is significantly higher in the age group 0f 56 to 60 years when compared to other age groups. P value is 0.029 and hence it is statistically significant. 
Figure 5: Bar graph showing the correlation between cognitive impairment status of diabetic individuals with chronic periodontitis among different age groups. The blue colour represents the normal cognitive group, green represents probable cognitive impairment group and red represents the possible cognitive impairment group. The possible cognitive impairment status is significantly higher in the age group 0f 56 to 60 years when compared to other age groups. P value is 0.029 and hence it is statistically significant. 
Discussion
The results of the present study have shown that the diabetic individuals with chronic periodontitis have increased chances of cognitive impairment when compared to non-diabetic individuals. It is also revealed that increased severity of both type 2 diabetes mellitus and periodontitis coexisted with the presence of cognitive impairment. Extensive research has been conducted in the past to explore the associations between diabetes mellitus and cognitive impairment as well as between periodontitis and cognitive impairment. Very few studies have correlated cognitive impairment, diabetes mellitus and chronic periodontitis. In this study we have tried correlating the cognitive impairment with age, gender in patients with diabetes mellitus and chronic periodontitis.
Cognitive impairment in elderly individuals can be due to various reasons, including medication side effects, metabolic derangements, long term illness, depression. With aging, the physical strength is reduced, thus compromising an individual’s ability to practice regular oral hygiene practices. As a result of reduced physiological functioning, oral care is ignored by the elderly patients. In our study, we have shown that possible chances of cognitive impairment is higher in the age group of 56 to 60 years. P value is 0.029 and hence it is statistically significant. This finding is also in agreement with a few earlier studies conducted correlating age and dementia. Aging is also independently associated with impaired wound healing, especially in the elderly diabetics, and this ignorance may prove detrimental by compromising the periodontal healing. These factors act like an acute exacerbation of already existing chronic inflammation, leading to systemic inflammation and its effects on the brain. Therefore, a routine periodontal treatment should be mandatory in the elderly diabetic patients to prevent the worsening of periodontal disease.
There was another interesting finding in this study, showing males having higher possible chances of cognitive impairment when compared to females. P value is 0.014 and hence it is statistically significant. This finding is also in accordance with earlier studies. Cognitive abilities include perception, attention, memory, motor, language, visual and spatial processing, and executive functions. These mental attributes are different in males and females. In addition, studies have also shown that oestrogen and testosterone accentuate cognitive functions in a similar fashion. Earlier studies have proved that due to hormonal changes they have better motor skills when compared to males.
It has been shown that the possible chance of cognitive impairment is higher among the patients with diabetes mellitus and chronic periodontitis when compared to the patients without periodontitis. P value is 0.01 and hence it is statistically significant. This finding is in accordance with few earlier studies which correlated diabetes mellitus and cognitive impairment. Diabetes involves hypercholesterolemia, APOE-ε4 allele genetic predisposition, hyperinsulinemia, macrovascular and microvascular pathologies, and increased systemic inflammatory mediators, all of which are responsible for causing neurodegeneration associated with cognitive impairment. Hyperglycemic state is known to cause end organ damage through increase in reactive oxygen species which leads to increased polyol pathway activation, increased formation of AGEs and activation of increased protein kinase C, acute changes in blood glucose are said to alter cerebral blood flow and causes osmotic changes in cerebral neurons. All these factors induce changes in the cognitive action of patients of diabetes mellitus.
Although the current research provides information about the correlation between dementia, diabetes mellitus and chronic periodontitis, it is still a hypothesis and requires further longitudinal studies to establish its feasibility. This study will have a huge impact in public health and will be helpful in creating awareness about the bidirectional relationship of diabetes mellitus with cognitive impairment and chronic periodontitis. The findings of this study will assist the clinician to be prepared for any treatment in the diabetic patients by knowing its prevalence. The current crosssectional research has its own inherent limitations. There is a geographic limitation to the study as it predominantly covers the South Indian population. This can be modified by performing longitudinal and periodic studies on comparatively younger individuals having diabetes and periodontitis should be conducted in the future as a target group to further strengthens the interrelated mechanism. The exact interrelated mechanisms between periodontitis and diabetes that participate in neurodegenerative effects need future studies. In the future, a larger population with different ethnicity can be included to provide better results and for precise diagnosis in the future studies. This study gives valuable information to oral health planners in proposing strategies for the development of oral health management.
Conclusion
The present study has shown that there is significant correlation between diabetes mellitus, chronic periodontitis and cognitive impairment. The treatment of periodontitis can be an important modifying treatment approach to reduce the systemic inflammatory burden and other mechanisms in patients who have uncontrolled diabetes liable to develop neurodegeneration. It is very important to diagnose, monitor, and treat periodontitis in patients with pre-existing cognitive impairment to limit its development and progression.
Author Contributions
Author 1: Vaishnavi Devi B, carried out the study by collecting data and drafted the manuscript after performing the necessary statistical analysis and in the preparation of the manuscript.
Author 2: Arthi Balasubramaniam, aided in conception of the topic, designing the study and supervision of the study, correction and final approval of the manuscript.
Acknowledgements
The authors would like to acknowledge the help and support rendered by the Department of Community Dentistry of SIMATS for their constant assistance with the research.
Conflict of Interest
The authors declare no potential conflict of interest.
Funding
The present project is sponsored by Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University.
References
- Gauthier S, Reisberg B, Zaudig M, et al. Mild Cognitive Impairment. Lancet. 367(9518): 1262-1270 (2006).
[Crossref]
- Ritchie K. Mild Cognitive Impairment: An Epidemiological Perspective. Dialogues Clin Neurosci. 6(4): 401-408 (2004).
- Xue M, Xu W, Ou Y-N, et al. Diabetes Mellitus and Risks of Cognitive Impairment and Dementia: A Systematic Review and Meta-analysis of 144 Prospective Studies. Ageing Res Rev. 55(9):100944 (2019).
- Palmer K, Fratiglioni L, Winblad B. What Is Mild Cognitive Impairment? Variations in Definitions and Evolution of Nondemented Persons with Cognitive Impairment. Acta Neurol Scand Suppl. 107(179):14–20 (2003).
- Ryan CM, Geckle MO, Orchard TJ. Cognitive Efficiency Declines over Time in Adults with Type 1 Diabetes: Effects of Micro- and Macrovascular Complications. Diabetologia. 46(6):940–948 (2003).
- Watts A, Gatz M, Crimmins EM. Inflammation as a Potential Mediator for the Association Between Periodontal Disease and Alzheimer’s Disease. Neuropsychiatr Dis Treat. 4(5):865-876 (2008).
- Burke SL, Maramaldi P, Cadet T, et al. Associations Between Depression, Sleep Disturbance, and Apolipoprotein E in the Development of Alzheimer’s Disease: Dementia. Int Psychogeriatr. 28(9):1409–1424 (2016).
- Wang H-K, Lin S-H, Sung P-S, et al. Population Based Study on Patients with Traumatic Brain Injury Suggests Increased Risk of Dementia. J Neurol Neurosurg Psychiatry. 83(11):1080–1085 (2012).
- Roher AE, Esh C, Kokjohn TA, et al. Circle of willis atherosclerosis is a risk factor for sporadic Alzheimer’s disease. Arterioscler Thromb Vasc Biol. 23(11):2055–2062 (2003).
- Vijayakumar TM, Sirisha GBN, Farzana Begam MD, et al. Mechanism Linking Cognitive Impairment and Diabetes Mellitus. Eur J Appl Physiol. 4(1):01–05 (2012).
- Huber JD. Diabetes, Cognitive Function, and the Blood-brain Barrier. Curr Pharm Des. 14(16):1594–1600 (2008).