Research Article - Neuropsychiatry (2018) Volume 8, Issue 3
A Journey from Hospital to Home: A Grounded Theory Study of Family Caregivers of Hospitalized Persons with Cognitive Impairment
- Corresponding Author:
- Yi-Chen Chiu
School of Nursing, College of Medicine, Chang Gung University, No. 259, Wen-Hwa 1st Rd., Kwei-Shan, Tao-Yuan 33302, Taiwan, ROC
Tel: +886 (03) 2118800 ext 5148 (office), (02)23631184 (Home)
Fax: (03) 2118400
Abstract
ABSTRACT
Background:
Hospitalization rates for persons with cognitive impairment are projected to increase in Taiwan. They are more likely to use inpatient services, psychotropic drugs, and have higher in-hospital mortality than persons without cognitive impairment. When this population is hospitalized, their family caregivers often experience strain, anxiety, and stress in their relationships with the care recipient and healthcare providers.
Objectives:
This study purposes were: (1) to explore experiences of family caregivers of persons with cognitive impairment during hospitalization, and (2) to develop a model explaining the patientcaregiver dyads’ acute hospitalization and discharge process from the caregivers’perspectives.
Methods:
Grounded theory was used to generalize a model. We recruited 11 caregivers and 10 persons with cognitive impairment. Data were collected in individual semi-structured interviews with caregivers. Interviews occurred during patients’ hospital stay or at home in the first year of discharge. Data were audio-taped and analysed by content analysis and constant comparative analysis.
Results:
The dyads’ hospitalization and post-discharge experiences were captured by four main themes: 1) early planning, 2) hospitalization issues piling up, 3) preparing for discharge, and 4) post-discharge experiences. During early planning, caregivers prepared for postdischarge caregiving and performed health-related and support tasks for the patient. During hospitalization, issues piled up, e.g. i.e. patients’ challenging behaviours, unfamiliar hospital environment, difficulty distinguishing patients’ delirium from cognitive impairment, and dissatisfaction with nursing care. When preparing for discharge, caregivers were concerned about the patients’ readiness for discharge and their self-efficacy for managing patients’ needs. If patients were not adequately prepared to return home, after discharge the patients’ condition rapidly spiralled down leading to unplanned re-admissions, which negatively affected caregivers’ health.
Conclusions:
Caregivers and cognitively impaired patients were challenged by the patients’ hospitalization due to factors that could have been minimized by skilled nursing dementia care. Nursing education to improve caregivers’ self-efficacy in patient care, could also have reduced postdischarge challenges.
Keywords
Acute care, Cognitive impairment, Discharge planning, Family caregivers, Hospitalization, Patient-caregiver dyads
Introduction
The prevalence of dementia is increasing worldwide, with a new case diagnosed every 3 seconds; in 2015 Asia had the largest number of persons estimated to have cognitive impairment [1]. Cognitively impaired persons have higher rates and different patterns of comorbidity than those without dementia or cognitive impairment [2]. They often visit hospitals due to acute events that may be preventable, e.g. acute cardiac ischaemia, falls, respiratory infections, pneumonia, dehydration, and urinary tract infections [3]. Persons with cognitive impairment have two to four times the hospitalization rates than other older adults [4] and hospitalization costs are higher, as a result of a greater number of complications and poorer outcomes [5]. For example, persons with cognitive impairment are at increased risk for sustaining a serious injury as a result of a fall, a three-fold increase in hip fracture, and an almost two-fold increase in mortality [6]. In addition, there is a greater likelihood of patients requiring residential care following discharge [7].
In Taiwan, the incidence rate for Alzheimer’s disease increased from 5.63/1,000 persons in 2005 to 8.17/1,000 persons in 2010, the mean number of hospitalizations (for any cause) per person with Alzheimer’s disease ranged from 1.78 to 2.42 annually, and hospitalization represented the largest component of annual cost [8]. In Scotland, older hospitalized persons with cognitive impairment had higher mortality and readmission rates than those without cognitive impairment [9]. In the UK, a hospital stay for persons with dementia was reported by their caregivers to negatively affect their dementia symptoms and general physical health [10].
As the numbers of persons with cognitive impairment increase, there is a higher demand for services, which impacts formal health care and increases the burden of informal caregivers, such as family members [11]. Although family caregiving can be meaningful and rewarding [12] the behaviours exhibited by persons with cognitive impairment can be detrimental to a caregivers’ health [13] and wellbeing [12]. Stress is experienced particularly at the time the person with cognitive impairment is undergoing the journey of from hospital to home [14].
Family caregivers in Taiwan play a significant role in caring for hospitalized persons, with or without cognitive impairment, due to Taiwan’s unique medical culture. Indeed, hospitals in Taiwan expect that family members will take care of patient needs usually covered by nurse aides or licensed practical nurses in western hospitals [15]. Family caregivers worldwide play important roles in older adults’ transition from hospital to home [16]. Caregivers not only assist this population in their activities of daily living, but also offer essential information to providers on these patients and perform health-related care tasks [16].
However, caregivers’ contributions are seldom recognized by healthcare professionals, and they are not often integrated into healthcare plans [17]. Furthermore, little is known about the experiences of family caregivers of persons with cognitive impairment during their transition from hospital to home in Taiwan. These knowledge gaps are relevant because caregivers often experience strain, anxiety, and distress in their relationships not only with cognitively impaired persons who are acutely ill, but also with their healthcare providers.
Despite family caregivers’ health directly impacting the care quality and survival of persons with cognitive impairment, most related studies on caregivers have been conducted in western countries, whose healthcare systems and cultures differ from those in Taiwan. Given these differences, we conducted a grounded theory study in Taiwan with two purposes: (1) to explore the experiences of family caregivers of persons with cognitive impairment during their hospitalization, and (2) to develop a model explaining the patientcaregiver dyads’ acute hospitalization and discharge process up to one year post-discharge from the caregivers’ perspectives.
Methods
▪ Design
A grounded theory method was chosen to develop a model focusing on family caregivers’ experiences when caring for acutely ill persons with cognitive impairment. Grounded theory is a fluid, interactive research process, which can identify problems in order to inform the initial methodological choices for data collection. Grounded theory is an inductive process; the researcher can develop theories and concepts to explain a phenomenon through observation and understanding of the experience of participants. We employed the process developed by Charmaz, which focuses on flexible guidelines [18] to study family caregiving related issues.
▪ Participants and ethics
Prior to recruiting patients, the study was approved by the Institutional Review Board of Chang Gung Memorial Hospital (number 98- 4092B). Patients were recruited by a snowball approach from two settings in northern Taiwan. One was a 3500-bed teaching hospital, and the other was a 312-bed area hospital. Potential patient-caregiver dyads were identified by hospital nurses who had been contacted by the first and second authors. Family caregivers of cognitively impaired patients who met our study criteria (had been hospitalized within the previous year) were referred to the first author by the participating neurologist.
Patients were included by these criteria: (1) cognitive impairment observed by nurses or identified in patients’ chart, and (2) had a family caregiver who spent at least 4 hours with or visited them three times during their hospital stay. Patients were excluded by these criteria: (1) in critical condition or (2) had acute neuropsychological symptoms. Caregivers were included by these criteria: (1) could communicate verbally; (2) spent at least 4 hours with or visited patients three times during their hospital stay. Caregivers were excluded if they were < 18 years old.
Of 13 caregiver-patient dyads contacted, 11 met the study criteria and agreed to participate. However, one person with cognitive impairment died during the study, leaving a sample of 11 caregivers and 10 cognitively impaired persons. The mean age of the patients with cognitive impairment was 73 years (SD=9.30; range=63-85), six were diagnosed with dementia, two had stroke, two had head injuries, and one had epilepsy. The caregivers had a mean age of 60.7 years (SD=9.46, range=50-69), mean years of education were 11.5 (SD=6.5; range=6-22); they had been caregivers from 3 months to 28 years. Five family caregivers were spouses, five were adult children, and one was a daughter-inlaw.
▪ Data collection
Before data collection, dyad participants were informed of the study procedures, their rights to refuse to answer any questions or to withdraw from the study at any time, and the confidentiality of their identities. All participants then signed informed consent forms. Data on caregivers’ experiences were collected through individual interviews by the first and second authors. The first author was a registered nurse with 22 years of gerontological nursing experience and 15 years’ experience in teaching/ research on dementia care. The second author was a registered nurse with 17 years’ experience in neurological and gerontological nursing.
Interviews were conducted using a semistructured guide developed by the first and second authors, reviewed by two gerontological nursing experts with extensive dementiacare experiences, and pre-tested on six family caregivers without further revision. The interview guide included questions about 1) caregivers’ experiences of patients’ hospitalization; 2) caregivers’ caregiving tasks, patients’ symptoms and caregivers’ understanding/perception of what caused these symptoms; 3) caregivers’ experiences with healthcare workers (nurses, physicians, nurses aides), including both positive and negative examples; and 4) the patients’ discharge planning experiences. Caregivers were interviewed in the hospital while patients were hospitalized or at home after patients had been discharged for less than 1 year. During the interviews, patients were present as much as possible. All interviews were audio-taped with participants’ permission. All interviews lasted between 45 to 90 minutes. Observations of spontaneous non-verbal expressions and gestures by the caregivers were captured with field notes immediately after the interview.
▪ Data analysis
All audio-taped interviews were transcribed verbatim. Following the grounded theory approach [18,19], we collected and analysed data simultaneously with content analysis and constant comparison among different sources of data such as interviews of physicians and case managers of the dementia centre in the participating hospital and in both individual and across transcripts [18-20]. Analysis began with identifying initial codes or naming a segment of data. For example, when a caregiver described a cognitively impaired person’s major symptoms, such as opening and closing drawers repetitively, we coded these data according to the caregivers’ description as patient’s repetitive behaviours. Then we used focused coding to concentrate on the most frequent and significant initial codes to sort, synthesize, integrate and organize a large amount of data [20]. For example, we combined several behavioural problems as challenging behaviours. Finally, we condensed the core themes with a focus on the hospitalization process for the person with cognitive impairment [20]. For example, we identified major themes and conceptualized the process as ‘a journey from hospital to home’. Theoretical coding was used to identify relationships among different concepts [21]. For example, a caregiver described how he lacked confidence to take his mother home (a patient with Alzheimer’s disease), when his mother was repetitively re-admitted due to functional decline, then a theoretical code of ‘the perceived low self-efficacy of caregivers impacts patients’ outcomes such as functional decline and unplanned readmission’ was recorded to assist the authors identifying the relationships between different concepts. To ensure study consistency and fidelity, the research team held regular monthly meetings, and the first author (principal investigator) met with research assistants biweekly to supervise participant recruitment and review and discuss transcripts. As a means of increasing the first author’s theoretical sensitivity toward the data [21], the thoughts of the research team and discussions were recorded after the meetings in addition to conducting intensive readings from nursing, psychology, sociology, medicine and epidemiology literature.
▪ Rigour
The trustworthiness of this study was promoted by meeting four criteria: credibility, dependability, transferability and confirmability [19]. Credibility was ensured by three authors having formal training in qualitative research methods and > 10 years extensive gerontological or clinical experiences. Credibility was also strengthened by the two interviewers working as an associate research fellow and a registered nurse, respectively, at the study hospitals, where they knew the healthcare environments. To avoid bias, the interviewed dyads were not interviewers’ cases. We also sent the transcripts back to one family caregiver for member checking. Confirmability was safeguarded by the first author identifying initial codes and the second author double coding the same data sets. Saturation was determined when the model generated from the findings was developed and revised with the help of the third author, a PhD-prepared scholar who was familiar with qualitative research methods until the research team all agreed with the sufficiency of the final model [22]. The transferability of the data was strengthened by rich description and the context of the dyads’ hospitalization experience [19]. The final model explains dyads’ experience from prior hospital admission through 1-year post discharge.
▪ Findings
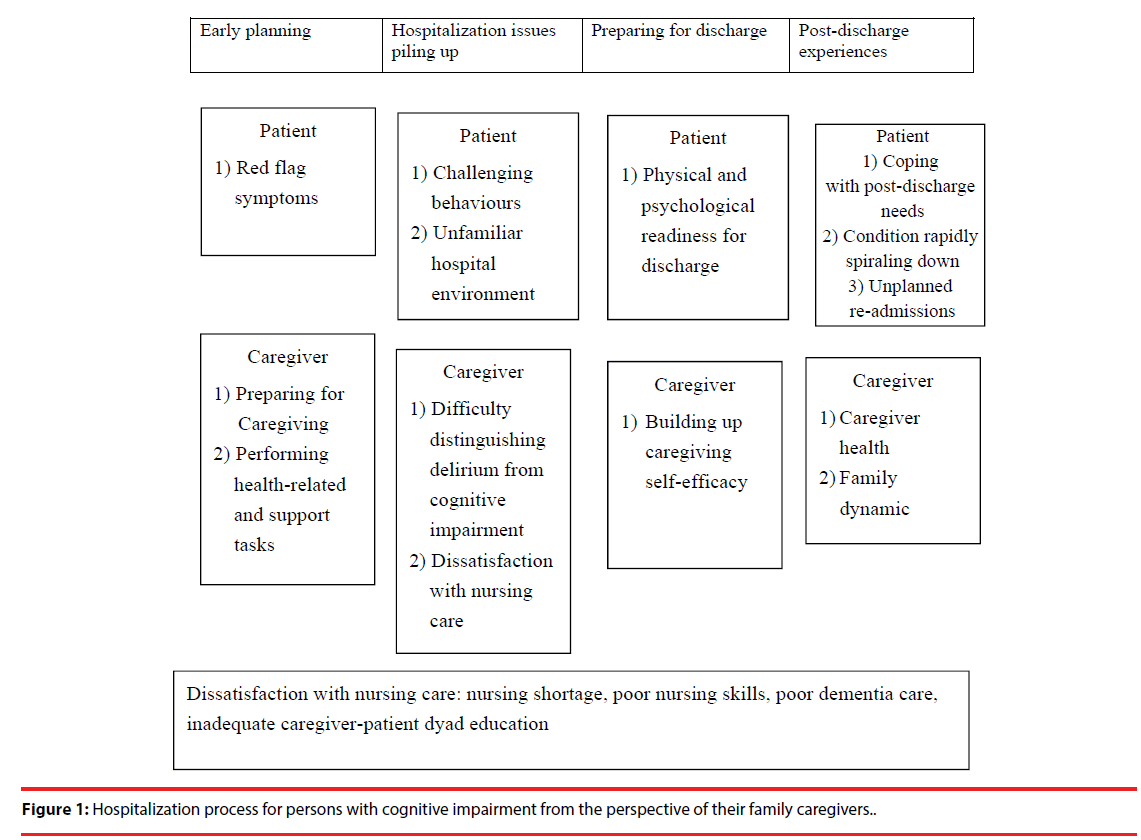
The core theme for family caregiver-patient dyads’ experience of hospitalization through 1-year post-discharge was ‘the journey from hospital to home’ (Figure 1). The model describing this journey had four components: early planning, hospitalization issues piling up, preparing for discharge, and post-discharge experiences. Each component had different aspects for caregivers and patients, revealing that the needs of the dyads varied depending on the changing needs of the person with cognitive impairment.
Early planning occurred before hospital admission. Families engaged in consultations to learn about proactive symptom management, such as red flag symptom identification and developed a care plan, which included understanding how to access primary care and help control chronic disease as well as a tentative working plan based on patients’ preference if persons with cognitive impairment need acute care.
This care plan was generated through family meetings, formal and/or informal. When persons with cognitive impairment were admitted for hospital care, caregivers prepared to take caregiving responsibility, which included direct care and health-related care tasks. During this phase, caregivers reported a need for various types of information, such as...manage patient behaviour, adapting to a hospital environment that seemed unfriendly, and training in distinguishing between delirium and cognitive impairment. Caregivers demanded a high quality of nursing care and instructions for taking care of patients with cognitive impairment. They preferred specialized nurses to fulfil the needs of the person with cognitive impairment. During the discharge preparation process and before returning home, caregivers needed instructions on specific tasks for handling the patients’ conditions post discharge as well as information on social resources. They believed good nursing instructions and training should be tailored to each dyad’s needs, with the centre for focus being the person with cognitive impairment and the family (Figure 1).
▪ Early planning
The early planning component of our model included three themes: 1) identifying patients’ red flag symptoms, 2) preparing for caregiving, and 3) performing health-related and support tasks for patients.
▪ Identifying red flag symptoms of persons with cognitive impairment
A salient predictor of older adults’ functional performance at hospital discharge is their preadmission ability to perform activities of daily living. Indeed, the days preceding hospitalization are often associated with functional loss related to acute illness. However, some of our caregivers did not observe any pre-admission functional decline or pain in care recipients. For example, caregiver F04-2 said, ‘My dad ... kept telling us [caregiver and his brothers] that he was in pain, but he couldn’t tell us where the pain came from and how it felt.’ Similarly, another caregiver [F03-2] said,
His legs became weaker and weaker, but I thought it was due to his age or gout. He has a history of gout, so I gave him gout medicine. On the morning of my scheduled bus tour, I asked him if he’d be all right at home without me, and he said he’d be fine. Then, I went out for the tour, but around 10 o’clock in the morning my daughter called and told me that Dad might have had a stroke that affected his leg... I told her to bring him to the hospital immediately.
▪ Preparing for caregiving
Most caregivers and persons with cognitive impairment had vague ideas about what to expect at the hospital, e.g. undergoing medical examinations and treatment, but some prepared by checking online information about hospitals’ and physicians’ reputations. For example, one caregiver (F06-2) said, ‘My son checked the internet and found your hospital and Doctor Lin who later arranged for my husband’s (cognitively impaired patient) physical examination and consultations with a psychiatrist and other specialists.’
Some families formed a consensus goal and a working plan to care for the patient with a team of family members, relatives, friends, or hired helpers. This team-care approach allowed caregivers to share the caregiving load, information about social resources, treatment options, financial considerations, patients’ preferences, and home modification to accommodate the patient’s disability. One caregiver (F03-2) said, ‘Before he [patient] was hospitalized this time, I’d already thought of a plan to modify our home to accommodate his walking problems.’ Similarly, another family caregiver explained:
My older sister, younger brother and I [all adult children] got together to form a consensus goal and developed a team care plan before Dad was admitted … We just wanted Dad to have surgery to remove the colon cancer and then receive chemotherapy, nothing fancy or advanced… I convinced my younger brother to apply for a foreign helper who could take care of Dad at home after his surgery. The time frame for hiring a foreign helper was perfect. When the hospital was about to discharge him, the foreign helper could stand by to take care of Dad at home if everything was on schedule … Then Dad could eat and enjoy the food he liked. [F01-4]
▪ Performing health-related and support tasks for patients
Caregivers played critical roles at home and in the hospital. They provided not only assistance for patients’ personal care, but also health-related care tasks for cognitively impaired patients, including direct care (e.g., monitoring medication doses and recording patients’ input and output), coordinating caregiving, maintaining financial security, and emotionally supporting patients. One caregiver (F04-2) said, ‘We [son caregivers] monitored the IV drip. When the IV bottle was empty, we’d notify the nurses’ Another caregiver (F02-2) said, ‘My son was worried that I [spouse caregiver] would burn out. He promised to wire some money into my bank account to hire a halfday helper.’ A third caregiver (F03-2) said, ‘When he [patient] became emotional or was in bad mood, I [spouse caregiver] would leave him alone for a while. After his stroke, I learned that he easily got angry. I’d endure his anger.’
▪ Hospitalization issues piling up
While cognitively impaired patients were hospitalized, their challenging behaviours and tendency towards delirium were exacerbated by the unfamiliar hospital environment. The accumulations of these issues left caregivers feeling hospital issues were piling up on them. Some caregivers faced challenging behaviours of patients who resisted care, the lack of appropriate support from healthcare staff, and the impacts of the unfamiliar hospital environment.
▪ Challenging behaviours of patients with cognitive impairment
One caregiver (F06-1) shared,
‘He [patient] didn’t sleep at night, but during the day. He slept all day long. He yelled at me and at the other patients; he made noises. The other patients couldn’t sleep, either… He kept walking around and pulling out the IV line.’ The same caregiver (F06-1-2) later said, ‘… My husband was running away. He was in the elevator, pushing the button, and a nurse held the elevator door to stop him…..’
Similarly, another caregiver (F06-2) said,
His [patient’s] son came to visit him, but he was in bad mood. Then he refused to take any medications. They argued with each other from 2 to 5 pm and till 10 pm. He [patient] finally took 4 pills, not all at once but one by one.
▪ Unfamiliar hospital environment
Staying in the unfamiliar and confusing hospital environment magnified the challenging behaviours of patients with cognitive impairment. These behaviours embarrassed caregivers who worried about bothering nearby patients and interrupting health professionals’ care routines. Therefore, caregivers stayed awake in the hospital to be vigilant and monitor patients’ movements and actions. As one caregiver (F02-1) said,
The hospital environment was new to my mom. She’d get lost … When I went home to take a break, she became very anxious and fearful. She told the neighbour patient that she had no money to go home. She couldn’t find the bathroom, even though it was next to her … Familiarizing her with the hospital environment was essential. For example, we walked my mom’s around to preserve her walking ability. She liked to walk around outside. Therefore, introducing her to the hospital environment was important to avoid her confusion.
▪ Difficulty distinguishing patients’ delirium from cognitive impairment
During hospitalization, patients with cognitive impairment have a higher chance of developing delirium, of their physical condition deteriorating, of experiencing sudden cognitive changes, and of losing functional ability. Caregivers had difficulty distinguishing patients’ delirium from cognitive impairment. For example, one caregiver (F01- 1) said, ‘If he [patient] didn’t get enough sleep, he would get confused ... he wouldn’t know where he was.’ [F01-1]. Another caregiver (F06-2) said, ‘When he [patient] talked, no one understood him. He created his own language.’
▪ Nursing care challenges
Some caregivers complained about the nursing shortage and poor nursing care, they mentioned that few nurses were available, care for patients with cognitive impairment was inadequate, and patient education needed improvement.
▪ Insufficient number of nurses
Caregivers complained about the need for more nurses. One (F01-01) said, ‘Nurses were busy.’ Another caregiver said, ‘I couldn’t find my nurse! I didn’t know where she was.…When I found a nurse, she was not in charge of my mom’s patient with cognitive impairment care. She wouldn’t help me. This was the worst part of my mom’s hospitalization.’
▪ Inadequate nurse training
Some caregivers viewed dementia care as a professional specialty and urged hospitals to train nurses appropriately. One caregiver (F04-2) said,
When my mum was admitted to the orthopaedic surgery ward, she had severe pain … the nurse’s aide that I hired helped my mum to roll over all by herself, and my mum didn’t feel a bit of pain. The nurse’s aide was skilled and experienced. I thought she was better than the nurses.
Another caregiver (F02-1) said, ‘The specialized nurses with lots of experience were good at dementia care. … The number of these specialized nurses should be considerably increased. We need an adequate number of nurses to provide high quality dementia care.’
▪ Nurse education for patient-caregiver dyads
Caregivers believed good nurses showed compassion and a caring attitude toward the dyads and taught caregivers strategies to care for and assist patients with cognitive impairment. For example, one caregiver (F01-2) said, ‘Nurses taught me how to feed my husband patient with cognitive impairment how to change his bed sheets and diapers. However, if a nurse spoke too fast, I [69-year-old spouse caregiver] couldn’t understand her.’
▪ Preparing for discharge
▪ Building up caregivers’ self-efficacy
Caregivers with a high perception of self-efficacy had confidence in their ability to handle dementia caregiving tasks effectively and were likely to assume the primary caregiver role once the cognitively impaired patient was discharged from the hospital. These caregivers tended to persist in providing care rather than seek institutional care when the patient’s condition worsened and caregiving tasks became increasingly difficult; they handled the caregiving role with relatively little emotional distress, and required relatively little support to maintain their own physical and mental health. These caregivers discovered caregivingrespite strategies and related information from various sources such as newspapers, nursing aides, nurses, and physicians. For example, one caregiver (F06-2) said,
I asked hospital nursing aides to show me how to care for patients like my husband who wandered around, didn’t sleep, and refused to take medicine. They taught me to grind the pills into powder and add it to his drinking water and favorite foods. I could find a way to solve the problem. I considered myself a person who can handle challenging situations by myself. … When I faced his sleep problems, I told myself that I must be persistent in facing these difficulties…
On the other hand, caregivers with low selfefficacy beliefs dwelled on their personal deficiencies, the difficulties of the task, and the negative consequences of failure. One caregiver (F04-2) said,
‘I knew my mum [patient] wasn’t a cooperative patient. Since she has Alzheimer’s disease, her thoughts are confused. Therefore, I didn’t think I could take care of her very well [after discharge home].’ This caregiver also said, I asked for a neurologist to evaluate my mom. While we were waiting for his visit, we were told that my mum would be discharged home soon. I got the impression that they wanted to discharge my mom as soon as possible … I wondered why a nurse came to tell me that we could go home if we wanted. Didn’t the patient’s condition need to be carefully assessed and the discharge plan formally approved by the doctor? ... This short discharge notice really surprised me…’
Sometimes, care coordination did not go smoothly, and caregivers felt a discontinuity of care from hospital to home. Caregiver F04-2 said,
The physical therapist came to evaluate my mum, but she wasn’t sensitive to my mum’s condition. There wasn’t any rehabilitation plans.… I’d like to learn how to take care of my mum if nurses taught me how to do it. I also asked the nurses to train the foreign helper I hired, but the appointment was messed up. My helper went home to care for my dad [also with cognitive impairment]. She didn’t receive any dementia care training.
▪ Post-discharge experiences
The immediate outcome of adequate discharge preparation was readiness for discharge. In this case, cognitively impaired patients’ needs were fulfilled, and their condition was stabilized. Therefore, their caregivers felt ready to go home.
▪ Being ready for discharge
Readiness for discharge was described by caregivers as patients’ physical and emotional conditions being stable on or near the day of discharge. Caregiver F06-2 said,
My husband [patient] has improved to 80 or 90%. When he came to the hospital, he kept opening drawers and picking up things. I put them back, but he opened the drawers again and picked up things. Now, he can sit for over an hour when his sister and son come to visit him … He couldn’t do this when he first arrived at the hospital.
When patients’ conditions were not stabilized, caregivers did not feel comfortable about their being discharged home. As one caregiver (F01- 2) said,
I was so worried whether my husband [patient] had anaemia that I kept asking the doctor to double check on that. If my husband still had anaemia … and fever, I didn’t feel it was all right to go home. The doctor was responsible for treating anaemia, right? Even though the doctor told me that my husband could go home, I was still very worried. What if the anaemia impacted my husband’s health? Would he be all right?
▪ Coping with post-discharge needs
When cognitively impaired patients were ready to go home, their caregivers expected intermediate outcomes: coping with post-discharge needs, such as managing patient care, visiting outpatient rehabilitation, ensuring financial security, and coordinating formal and/or informal support. One spouse caregiver (F03-2) said,
We [caregiver and two daughters] thought he [patient] was ready to go home. He’d learned the rehabilitation exercises and promised that he’d do his exercises at home. … Now he’s much better, he can brush his teeth, and has resumed his favourite pastime of studying Chinese calligraphy.
▪ Unplanned re-admissions
If family caregivers were not prepared, they had difficulty coping with transitional stresses and returning to the hospital or emergency department for unresolved physical problems or accidents such as falls. One caregiver (F04-2) who did not feel confident to take his mother home said,
My mum [patient] was first admitted to the emergency room on September 30th because of a fall. Then she was in and out of the hospital four times within one and half months -all for fall-related consequences, such as dehydration/malnutrition, urinary tract infection and unidentified pain. Last time, we went to the emergency room because of her urinary tract infection.
▪ Patients’ condition rapidly spiraling down
When patients were repeatedly admitted to hospital, their functioning and behavioural problems seemed to deteriorate even more rapidly, as if spiralling down. As one caregiver (F03-2) said,
When my mom [patient] was hospitalized for the first time [due to a fracture after falling], she was all right. However, when she was admitted the second time, she was confused. She didn’t understand that she was in the hospital. She thought she was in the hallway of her house. Suddenly she thought she was in a war, fighting. She tried to find the washroom which was next to her, but she couldn’t get to it. Her mind was totally disturbed… totally.
▪ Family caregiver outcomes
During the hospitalization process, caregivers’ health (physical and emotional) was sometimes impacted due to multiple caregiving stresses. Some caregivers also worked outside the home, leading to conflict between caregiving and work. However, the patient’s illness sometimes changed family dynamics.
▪ Caregivers’ health
After I came here [the hospital] to take care of my husband [patient], I felt that my health deteriorated. I lost weight, felt tired, worried.…. I am a breast cancer survivor. Last time, you [the interview nurse] told me that my blood pressure was a little bit higher. Usually I’d exercise, but now that I’m spending so much time in the hospital, I don’t do any exercise. [F01-02]
Some caregivers were still employed outside the home. Therefore, when patients were discharged home, they had difficulty maintaining a balance between life and work while caregiving. These caregivers sometimes responded negatively to cognitively impaired patients and caring for the patient at home; they even considered themselves patients. For example, caregiver F01-1 said,
I [son caregiver] have to work every day as the family bread winner. Therefore, my caregiving stress was high, and I felt depressed [when I had to work] … Sometimes, I lost my patience. I had no time to listen and talk to my dad (patient with cognitive impairment). Our conversations were cut short. When I got back home from work, I was exhausted. I just talked to him briefly, fixing him some food ...That’s all. There was no real conversation. Sometimes, I forgot to put a diaper on him since I was busy preparing meals for the family. Then I had to clean the floor all day. Busy, very busy.
▪ Family dynamics
Sometimes, family support helped. When caregivers faced multiple stresses, those with support from other family members became even closer to their family after the patient was discharged home. For example, one caregiver (F03-2) said,
After he [patient with cognitive impairment] was discharged home, I felt tied up. I couldn’t go anywhere … However, my four daughters came to visit us more often to help me out on taking care of him. My daughters and I felt closer after he came home.
Discussion
This study contributes to knowledge about the hospitalization process for persons with cognitive impairment from the perspective of their family caregivers in Taiwan by describing their experiences over the journey from hospital to home up to 1 year after discharge. Our Taiwanese caregivers contributed extensively to the health-related care tasks of cognitively impaired patients during their hospital stay, since hospitals in Taiwan expect that family members will take care of patient needs usually covered by nurse aides and licensed nurses in western hospitals [15].
We found that caregivers could not identify cognitively impaired persons’ red flag symptoms before admission due to patients’ inability to specify where they feel pain and caregivers’ lack of training. Indeed, 42% of geriatric Italian patients experienced functional decline 2 weeks before hospitalization, with older age and dementia significantly predicting this decline [23], while pain in cognitively impaired patients was poorly managed [24,25]. Even though chronic conditions are more prevalent in older persons with cognitive impairment than without, those with cognitive impairment did not have the same access to treatment and disease monitoring as those with similar comorbidities but without cognitive impairment [24]. Therefore, healthcare providers need to educate caregivers on noticing cognitively impaired patients’ red flag symptoms and managing their comorbidities to avoid functional decline and unnecessary hospital admissions. Another strategy for avoiding unnecessary admissions is to provide a 24-hour/7-day hot line for family caregivers to consult with geriatric and dementia-care experts.
We also found that during hospitalization, caregivers faced several issues that piled up, such as the unfamiliar hospital environment, cognitively impaired patients’ challenging behaviours, difficulty distinguishing delirium and cognitive impairment, and dissatisfaction with nursing care. Most of the nursing staff had not received appropriate dementia-care training and lacked adequate resources to provide personand family-centred care. Nurses’ education of caregiver-cognitively impaired-patient dyads was not tailored to meet their needs. Our caregivers’ dissatisfaction with nursing care for patients with cognitive impairment echoes a report that 77% of UK caregivers were dissatisfied with the quality of nursing care for their loved one with dementia [10].
At discharge, the unmet needs of cognitively impaired older adults and their caregivers included negotiating care with multiple providers, managing the patient’s illness (e.g. identifying and managing physical and psychological symptoms, adhering with prescribed therapies, managing problem behaviours, and lack of awareness of community resources), and psychosocial support and coping (e.g. patients’ depression and caregivers’ burden, depression, isolation and fear) [25,26]. The emotional distress experienced by family caregivers during the care recipient’s hospital stay is also supported by Boltz et al. [27] who found that caregivers of persons with dementia in the US experienced consistent fatigue, anxiety, depression and sleep disturbance while the care receiver was hospitalized. Meeting the discharge needs of this caregiver-patient population has plenty of room for improvement in hospital environment, nurse training, nursing care and nurse education.
We also found the participating hospitals had no formalized discharge planning for caregivercognitively impaired patient dyads, a process which requires a proactive and multidisciplinary approach led by higher- or executive-level administrative staff. Our findings are consistent with reports that medical students in clerkship observations reported discharge planning as rushed or premature due to poor communication, insufficient time planning the discharge, and no patient education [28]. Our findings confirm evidence from a 39-study integrated review, which demonstrated preparation for discharge should begin before admission and that staff nurses having the most contact with patients should play a critical role in preparing caregiverpatient dyads’ journey from hospital to home [29]. Discharge planning which is rushed, does not include a multidisciplinary approach, and fails to educate patients leads to little attention being paid to the needs of caregiver-cognitively impaired-patient dyads, which was apparent in the present study and in some mixed-methods research studies [28,30]. Taken together, these results indicate the need to establish a standardized protocol for systematic discharge planning tailored to the post-discharge needs of caregivers and cognitively impaired patients.
Our findings indicate that not all nursing care was unsatisfactory. Those caregivers who received good nursing care education developed higher levels of perceived self-efficacy, and their care recipients seemed readier for discharge home, with stable physical and psychological conditions. These patients encountered less adverse outcomes such as unplanned readmissions. Caregivers who felt ready to go home with patients who were physically and psychologically stable were less likely to experience stress, which may have resulted in lower negative impacts on caregivers’ physical and emotional health. Our results on caregivers’ perceived self-efficacy echo a study showing caregivers of persons with dementia who received coaching from health staff improved perceived self-efficacy with regards to managing the care receiver’s behavioural problems, seeking help from others, and attending to their own health needs [31]. These results suggest that teaching/ coaching caregivers to improve their selfefficacy in managing the symptoms of cognitive impairment may improve both patients’ and caregivers’ post-discharge outcomes.
We also generated a conceptual model for the hospitalization to discharge process for caregivers of cognitively impaired patients. This model is supported by a similar theoretical framework developed for family caregivers of hospitalized frail patients during the transition from hospital to home, which also reveals similar patterns of need changes for the dyads [15]. However, our theoretical framework highlights the demands on family caregivers to perform health related tasks and face the effects of hospital issues piling-up: unfriendly hospital environments on patients with cognitive impairment and their manifestation of challenging behaviours, delirium and lack of medical health professional support. Most importantly, our study extends the postdischarge period up to one year and identifies the changing needs of cognitively impaired patients and their caregivers as well as the long-term outcomes of patients with cognitive impairment such as functional decline, pain and unplanned re-admission. We also found a poor outcome for the patient could result in a deteriorated health outcome for the caregiver, as well as changing the dynamics for the family. Therefore, nursing interventions should focus on the changing needs of the dyads and integrate primary care with acute care for the patients with cognitive impairment. Most importantly, the patient and family should be placed at the centre of care when developing a tailored care plan for the dyads.
Several study limitations were found. First, transferability of the results of our study to all caregiver-cognitively impaired-patient dyads is limited by our sample being Taiwanese people living in northern areas of the island. However, our grounded theory study provides data on the in-depth experiences of the journey from hospital to home from the perspective of caregivers for cognitively impaired individuals from northern Taiwan. Second, although observations of spontaneous non-verbal expressions were conducted, the interviews were the primary form of data collection. Without more structured observations, some of the experiences of caregivers or patients with cognitive impairment, which were difficult to articulate, might be missing. Future studies should be conducted with a combination of dyad interviews and structured observations in different areas of Taiwan as well as other countries, and different cultures, to fully explore the experiences of the journey from hospital to home for patients with cognitive impairment and their caregivers. In addition, the findings of this study are consistent with those in other countries; therefore, our model may offer a guide which could be used to develop effective interventions in order to provide better care for the dyads in different cultures, which merit future research.
Acknowledgements
The authors are grateful to the research participants for their invaluable help by sharing their experiences with our research team and the grand support from the CMRPD 1A0042 and NSC 97-2420-H-002- 203.
Funding sources
CMRPD 1A0042 and NSC 97-2420-H-002- 203
Conflicts of Interest
The authors declare no competing financial interests of any kind.
References
- Alzheimer ’s disease International. World Alzheimer Report 2015. The Global Impact of Dementia. An analysis of prevalence, incidence, cost and trends.
- Bauer K, Schwarzkopf L, Graessel E, et al. A claims data-based comparison of comorbidity in individuals with and without dementia. BMC. Geriatr 14:10 (2014).
- Phelan EA, Borson S, Grothaus L, et al. Association between incident dementia and risk of hospitalization. Journal. of. American. Medical. Association 307(2), 165-172 (2012).
- Feng Z, Coots LA, Kaganova Y, et al. Hospital and ED use among Medicare beneficiaries with dementia varies by setting and proximity to death. Health. Affairs (Millwood) 33(4), 683–690 (2014).
- Bail K, Goss J, Draper B, et al. The cost of hospital-acquired complications for older people with and without dementia; a retrospective cohort study. BMC. Health. Services. Research 15(1), 91 (2015).
- Baker NL, Cook MN, Arrighi HM, et al. Hip fracture risk and subsequent mortality among Alzheimer’s disease patients in the United Kingdom, 1988–2007. Age. And. Ageing 40(1) 49–54 (2011).
- Zekry D, Herrmann FR, Grandjean R, et al. Does dementia predict adverse hospitalization outcomes? A prospective study in aged inpatients. Int. J. Geriatr. Psychiatry 24(3), 283-91 (2009).
- Hung YN, Kadziola Z, Brnabic AJM, et al. The epidemiology and burden of Alzheimer’s disease in Taiwan utilizing data from the National Health Insurance Research Database. CEOR 8(1), 387-395 (2016).
- Reynish E, Hapca SM, De Souza N, et al. Epidemiology and outcomes of people with dementia, delirium, and unspecified cognitive impairment in the general hospital: prospective cohort study of 10,014 admissions. BMC. Medicine, 15, 140 (2017).
- Alzheimer’s Society. Counting the cost: caring for people with dementia on hospital wards (2009).
- Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues. Clin. Neurosci 11(1), 217-228 (2009).
- Shyu YI, Yang CT, Huang CC, et al. Influences of mutuality, preparedness, and balance on caregivers of patients with dementia. J. Nurs. Res 18(3), 155-63 (2010).
- Chiu YC, Lee YN, Wang PC, et al. Family caregivers’ sleep disturbance and its associations with multilevel stressors when caring for patients with dementia. Aging. And. Mental. Health 18(1), 92–101 (2014).
- Sadak T, Zdon SF, Ischado E, et al. Potentially preventable hospitalizations in dementia: family caregiver experiences. International. Psychiatrics 29(7), 1201-1211 (2017).
- Shyu YI. The Needs of family caregivers of frail elders during the transition from hospital to home: A Taiwanese Sample. J. Adv. Nurs, 32(3), 619-625 (2000).
- Gibson MJ, Kelly KA, Kaplan AK. Family caregiving and transitional care: a critical review. Family Caregiver Alliance (2012).
- Graham CL, Ivey SL, Neuhauser L. From hospital to home: assessing the transitional care needs of vulnerable seniors. Gerontology 49(1), 23-33 (2009).
- Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis, 1st ed. Sage, Thousand Oaks, CA (2012).
- Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA, Sage (1985).
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook (2nd ed.). Thousand Oaks, CA: Sage (1994).
- Glaser BG. Theoretical Sensitivity. Sociology Press, Mill Valley, California (1978).
- Dey I. Grounding grounded theory. San Diego, CA: Academic Press (1999).
- Palleschi L, Fimognari FL, Pierantozzi A, et al. Acute functional decline before hospitalization in older patients. Geriatr. Gerontol. Int 14(4), 769-777(2014).
- Bunn F, Burn A, Goodman C, et al. Comorbidity and dementia: a scoping review of the literature. BMC Medicine 12(1), 192 (2014).
- Naylor M, Brooten D, Jones R, et al. Comprehensive discharge planning for the hospitalized elderly: a randomized clinical trial. Ann. Intern. Med 120(1), 999–1006 (1994).
- Naylor M, Hirschman KB, Bowles KH, et al. Care coordination for cognitively impaired older adults and their caregivers. Home. Health. Care. Service. Quality 26(4), 57-78 (2007).
- Boltz M, Chippendak, T, Resnick B, et al. Anxiety in family caregivers of hospitalized persons with dementia: contributing factors and responses. Alzheimer. Dis. Assoc. Disord 29(3), 236-241 (2015).
- Block L, Morgan-Gouveia M, Levine RB, et al. We could have done a better job: a qualitative study of medical student reflections on safe hospital discharge. J. Am. Geriatr. Soc 62(6), 1147-1154 (2014).
- Nosbusch JM, Weiss ME, Bobay KL. An integrated review of the literature on challenges confronting the acute care staff nurse in discharge planning. J. Clin. Nurs 20(5/6), 754-774 (2011).
- Boltz M, Chippendak T, Resnick B, et al. Testing family-centered, functional focused care in hospitalized persons with dementia. Neurodegener. Dis. Manag 5(3), 203-215 (2015).
- Chenoweth L, Stein-Parbury J, White D, et al. Coaching in self-efficacy improves care responses, health, and well-being in dementia carers: a pro/post-test/follow-up study. BMC Health Service Research 16(1), 166 (2016).