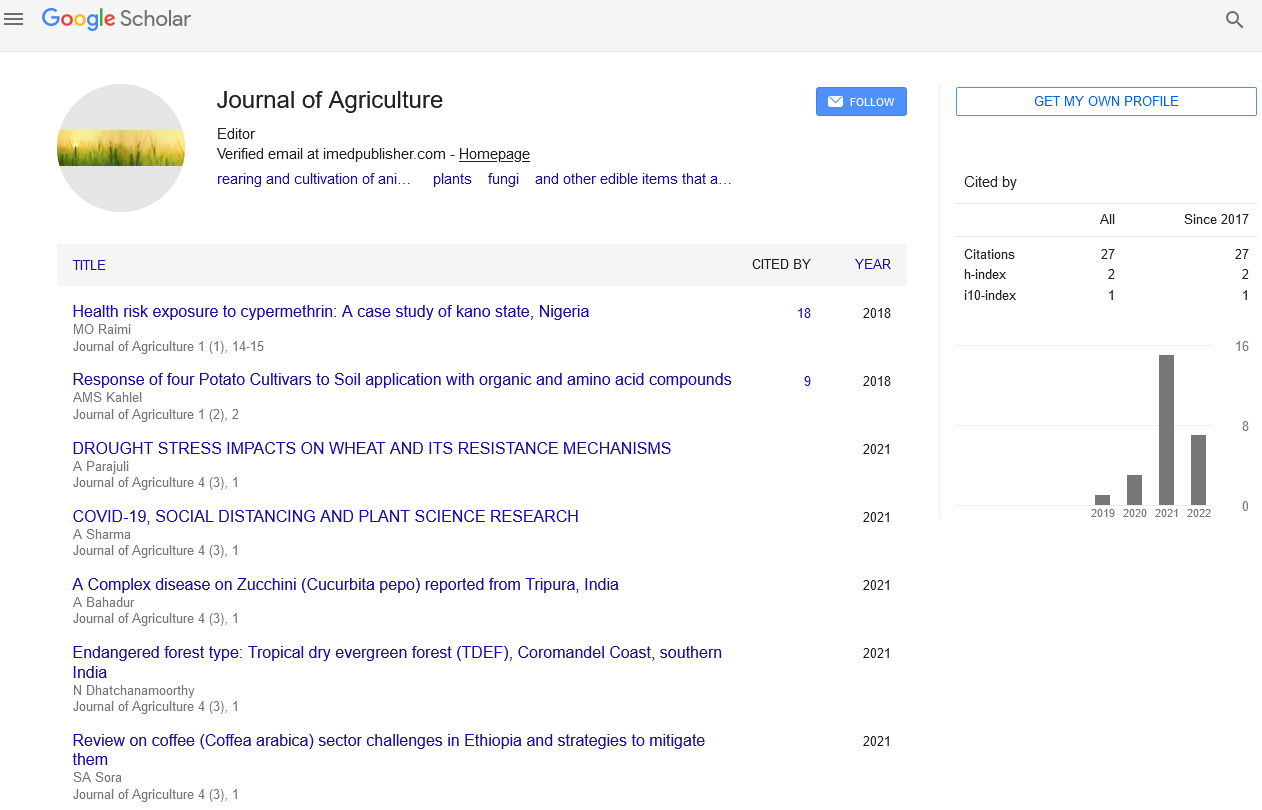
Commentary - Journal of Agriculture (2022) Volume 5, Issue 3
A Novel Intra-body Sensor for Vaginal Temperature Monitoring
Sunali Mahajan*
Division of Statistics and Computer Science, India
Received: 02-Jun-2022, Manuscript No. jagri-22-42453; Editor assigned: 06-Jun-2022, PreQC No. jagri-22- 42453(PQ); Reviewed: 20-Jun-2022, QC No. jagri-22-42453; Revised: 23-Jun-2022, Manuscript No. jagri- 22-42453(R); Published: 30-Jun-2022, DOI: 10.37532/jagri.2022.5(3).56-57
Abstract
Many researchers in this domain have been striving to find relationships between intravaginal temperature and certain female health conditions, such as ovulation and fertile period since woman’s intra-vaginal temperature is one of the body parameters most preferred in such studies. However, due to lack of an appropriate technology, medical research devoted to studying correlations of such body parameters with certain woman’s’ body phenomena could not obtain better results. This article presents the design and implementation of a novel intra-body sensor for acquisition and monitoring of intravaginal temperatures. Over the years some medical studies have tried to better understand the internal behavior of human beings. Many researchers in this domain have been striving to find relationships between intra-vaginal temperature and certain female health conditions, such as ovulation and fertile period since woman’s intra-vaginal temperature is one of the body parameters most preferred in such studies.
Keywords
e-Health • intra-body sensor • ovulation • temperature Monitoring
Introduction
This article presents the event of a completely unique intra-body device that’s ideal for precise medical study for the acquisition of human body physiological parameters. in step with the studies administered over the past years, there’s a detailed relationship between sure material body states and completely different body temperatures (e.g. metastasis, shortening, intake of food, and a few disease’s symptoms). Even throughout the day (24 hours) and for constant individual, the temperature varies by about 0.5 degree Centigrade (ºC) [1].
The observation of the human physiological parameters might facilitate medical employees in correlating temperature readings with some pathology. Intra-vaginal temperature is one in all the feminine body’s physiological parameters that’s the foremost controlled and helpful for observation in fertility medical studies. for each lady, the characterization of this parameter might facilitate in establishing a pattern for the correlation of intra-vaginal temperature readings and oscillation stage. This could help females to observe their biological process and fertile periods such it might be simple to grasp the most effective time to urge pregnant. Conversely, it might conjointly facilitate females avoid maternity if they’ll recognize the occurrence of this era.
To the most effective of our data, none of the present biosensors will gather continuous, long-term measurements of feminine intra-vaginal temperatures that square measure used for estimation and detection of ovulation and fertile periods. All studies supported basal temperature management used an awfully painful method for the females, during which their basal temperatures got to be gaga a basal body thermometer at specific times (6:30 AM is recommended). Each reading is then accustomed fill out a fertility chart. With the continual filling of this chart, females might observe their stage by observing the increasing of their basal temperature. Besides the delineated issues, another debatable issue during this technique is that the validity of the info gathered [2]. Typically the activity of the temperature, performed by every feminine, won’t be taken in Associate in nursing applicable approach. Possibly, the temperature readings might be wrong on inappropriate handling of the measuring device, therefore leading to incorrect knowledge on the chart. Our aim was to produce a medical study with a usable device to assemble intra-vaginal temperature values throughout a particular time (e.g. emission cycle) outlined by the medical employees. This study tried to establish a correlation between intra-vaginal temperature and a few stages of the feminine fruitful system. The information gathered by this device won’t solely be accustomed monitor intra-vaginal temperature, but also, to develop studies that might facilitate medical employees gain higher data of the connection between intravaginal temperature and a few maternity problems. Therefore, the most goal of this work Sensors 2009, 9 2 7 9 9 was the proposal, creation, testing and validation of a replacement intra-body device for duct temperature acquisition and observation [3].
Description
To the most effective of our data, none of the present biosensors will gather continuous, long-term measurements of feminine intra-vaginal temperatures that square measure used for estimation and detection of ovulation and fertile periods. All studies supported basal temperature management used a awfully painful method for the females, during which their basal temperatures got to be gaga a basal body thermometer at specific times (6:30 AM is recommended). This study tried to establish a correlation between intravaginal temperature and a few stages of the feminine fruitful system. The info gathered by this device won’t solely be accustomed monitor intra-vaginal temperature, but also, to develop studies that might facilitate medical employees gain higher data of the connection between intra-vaginal temperature and a few maternity problems [4].
Conflict of Interests
None
Acknowledgments
None
References
- Patel S, Lorincz K, Hughes R et al .Analysis of feature space for monitoring persons with parkinson's disease with application to a wireless wearable sensor system. In Engineering in Medicine and Biology Society. EMBS. 29th Annual International Conference of the IEEE, Lyon, France. 6290-6293(2007).
- Chan CH, Poon CCY, Wong RCS et al. A hybrid body sensor network for continuous and long-term measurement of arterial blood pressure. In International Summer School and Symposium on Medical Devices and Biosensors, Cambridge, U.K., 4th IEEE/EMBS, pp. 121-123(2007).
- Taylor HW, Shidler SE, Lasley BL et al. FSH biosensor to detect postpartum ovarian recrudescence. In Conference Proceeding 26th Annual Internationaz Conference of the IEEE Engineering in Medicine and Biology Society (IEMBS '04). San Francisco, CA, USA; pp. 1998-2001(2004).
- Pantelopoulos A, Bourbakis N. A survey on wearable biosensor systems for health monitoring. In Conf. Proc. IEEE Eng. Med. Biol. Canada. 4887-4890(2008).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref