Case Report - Imaging in Medicine (2017) Volume 9, Issue 4
A rare case of incidentally detected renal replacement lipomatosis
Sanjib Kumar Das*SCB Medical College, Cuttack, Odisha, India
- Corresponding Author:
- Sanjib Kumar Das
SCB Medical College
Cuttack, Odisha, India
E-mail: sanjib1988@gmail.com
Abstract
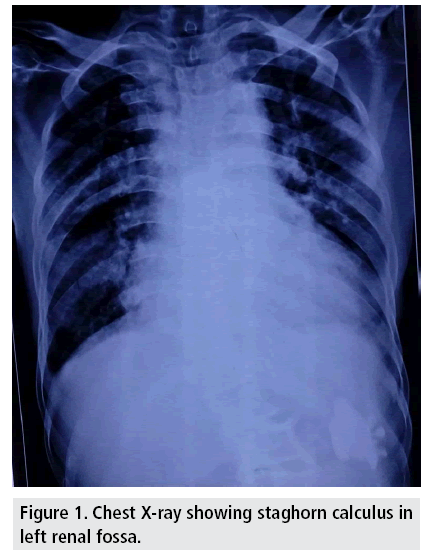
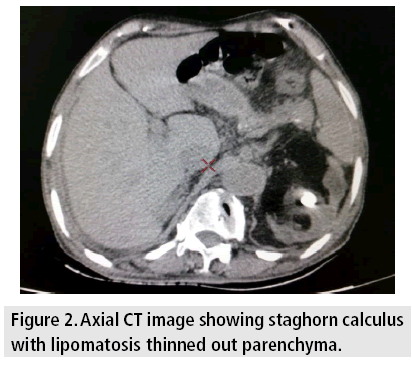
We present a case of incidentally detected renal replacement lipomatosis in an Indian patient of 90 years who presented to us for chest evaluation. On Chest X-ray, we didn't find any chest abnormality except scoliosis. A staghorn calculus of size 5.5*3.7 cm was noted in left kidney for which a noncontrast CT scan was ordered. NCCT revealed a staghorn calculus in left renal pelvis with replacement lipomatosis, atrophic cortical parenchyma and patchy areas of low attenuation in renal parenchyma.
Keywords
staghorn calculus • cortical atrophy • replacement lipomatosis
Introduction
A 90 years old Indian patient presented to our department for chest evaluation referred from dept. of medicine with complaints of left lower chest pain and discomfort for 1 month. PA Chest X-ray was done which revealed no chest abnormality except scoliosis. Left pleural space appeared free. But incidentally a radioopaque calculus was noted in left renal fossa. The patient was then referred for Noncontrast CT scan as the patient had impaired renal status. CT scan showed a staghorn calculus in left renal pelvis with replacement of renal parenchyma with fatty tissue. Thinning of renal cortex suggestive of atrophy was also noted with patchy areas of low attenuation in the cortex (FIGURES 1-3).
Renal sinus lipomatosis, renal replacement lipomatosis and fibrolipomatosis represent a spectrum of changes denoting a common underlying pathology which include replacement of renal parenchyma by fatty tissue and cortical atrophy, with renal sinus lipomatosis forming the mildest form of the spectrum and replacement lipomatosis being the severest [1-3].
Renal sinus lipomatosis representing the mildest form of the spectrum usually presents at sixth to seventh decades of life. It represents a degenerative process thought to be associated with ageing, obesity or use of exogenous steroids. It does not have any clinical significance with most being detected at autopsy. However it can sometimes mimic renal mass leading to misdiagnosis. Radiologically it appears as increase in radiolucency in renal sinus with stretching of renal infundibula [1,3,4].
Renal replacement lipomatosis being the severest form of the spectrum shows extreme cortical atrophy secondary to renal calculus, infection and long standing hydronephrosis but with preservation of reniform shape of kidney. It is associated with ageing, obesity, use of exogenous steroids, calculus and tuberculosis can be seen after transplantation. It is usually unilateral [5].
Clinical features are usually nonspecific, may present with flank pain, fever or weight loss.
Imaging Findings
Radiographs help to demonstrate the calculus if any. Sometimes there is increased lucency in the affected renal fossa indicating increased amount of fat. The kidney is usually enlarged which on intravenous pyelography shows decreased function [6]. The presence of a lucent mass surrounding a large calculus characterizes renal replacement lipomatosis [7]. On ultrasonography, there is presence of calculus showing posterior acoustic shadowing. Ill-defined hyperechoic mass is often visualized representing the lipomatous tissue in renal sinus. The residual parenchyma is usually poorly delineated on USG, for which CT scan is indicated. CT scan is the modality of choice being most accurate in distinguishing the characteristic features of renal replacement lipomatosis [8]. CT scan shows the presence of calculus with characteristic distribution of fat in renal sinus and peronephric space and cortical atrophy. CT scan can be useful prior to surgery as a modality to distinguish any abscess or fistula formation which can help in preoperative planning.
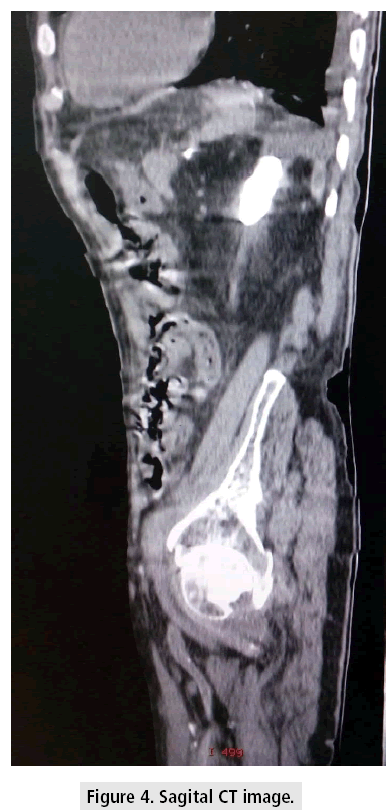
The major differential includes xanthogranulomatous pyelonephritis where lipid laden macrophages will be present inside the parenchyma in contrary to replacement lipomatosis which shows fat outside the parenchyma [5,8]. Other differentials include fat containing neoplasms like lipoma, angiolipoma and liposarcoma . Parenchymal atrophy and staghorn calculus are not the features of these neoplasms [5,6] (FIGURE 4).
Discussion
The patient was diagnosed as case of Renal Replacent Lipomatosis which is an extreme form of renal sinus lipomatosis with possible existence of xanthgranulomatous pyelonephritis. But contrast enhanced CT scan could not be done as the patient had impaired renal function. So confident diagnosis of xanthogranulomatous pyelonephritis could not be made.
Conclusion
Renal replacement lipomatosis is a rare condition associated with staghorn calculus. It may mimic renal neoplasm. CT scan is the main modality of choice to differentiate it from renal neoplasms. Coexistent xanthogranulomatous pyelonephritis may be present but the combined entity appears to be extremely rare.
References
- Faegenburg D, Bosniak MA, Evans JA. Renal sinus lipomatosis: its demonstration by nephrotomography. Radiology. 83, 987-997 (1964).
- Olsson 0, Weiland P. Renal fibrohipomatosis. Acta. Radiol. 1, 1061-1070 (1963).
- Marjorie A, Morton B, Richard G et al. Replacement lipomatosis of kidney. Am. J. Roentgenol. 130, 1087-1091 (1978).
- Shah VB, Rupani AB, Deokar MS et al. Idiopathic renal replacement lipomatosis: A case report and review of literature. Indian. J. Pathol. Microbial. 52, 522-523 (2009).
- Stephen K, Richard W. Replacement Lipomatosis of the Kidney. Radiology. 215, 754-756 (2000).
- Kullendorff B, Nyman U, Aspelin P. Computed tomography in renal replacement lipomatosis. Acta. Radiol. 1851 (2016).
- Posadas MA, Chua E, Thomas B et al. Allograft dysfunction in a patient with an odd-looking kidney: Case of renal lipomatosis and review of literature. Clin. Kidney. J. 359-361 (2012).
- Subramanyam BR, Bosniak MA, Horii SC et al. Replacement lipomatosis of the kidney: diagnosis by computed tomography and sonography. Radiology. 148, 791-792 (1983).