Case Report - Clinical Investigation (2023) Volume 13, Issue 1
A report of short term spontaneous regression of herniated lumbar disc
- Corresponding Author:
- Ajaya Kumar Ayyappan Unnithan
Neurosurgeon, Muthoot Hospital, Kozhencherry, Kerala, India
E-mail: drajayakumara@gmail.com
Abstract
Introduction: Spontaneous regression of herniated lumbar discs over a course of time is well documented in literature. But the concomitant relief of symptoms is not seen always. The reports of regression within 3 months are a few. Kim ES et al reported about the peroperative identification of regression of an extruded disc fragment, during microdiscectomy 2 months after the Magnetic Resonance Imgaging (MRI).
Case presentation: A 58-year lady presented with backache, left leg pain, and weakness for 3 months. A Magnetic Resonance Imaging (MRI) scan of lumbosacral spine, taken three months back, showed L3-4 disc extrusion and canal stenosis and grade 1 listhesis at L5-S1. She had improvement with conservative treatment. But she had recurrence of symptoms 10 days back. Straight leg raising test was positive at 40Ë? on left side. Dorsiflexion was grade 4 on left side. Sensations of touch and vibration were reduced in L4 dermatomal region.
A repeat MRI scan was done to plan surgery. The disc extrusion at L3-4 had shrunk, with the residual listhesis at L5-S1. She was given gabapentin, methyl-cobolamine, and physiotherapy. She improved over 1 week.
Conclusions: Spontaneous regression of herniated lumbar disc can occur within three months, without corresponding symptomatic relief. So it is better to do a repeat imaging before planning surgery for a patient with a prior diagnosis of disc herniation. Thus an unnecessary surgery can be avoided.
Keywords
Intervertebral disc displacement • Magnetic resonance imaging • Spontaneous remission
Introduction
A large number of the extruded lumbar disc herniations have been found to regress over time. Kesikburun et al. have reported that about 3-4 of the patients with extruded lumbar disc herniation can have complete resolution in the repeat Magnetic Resonance Imaging (MRI) after an average followup period of 17 months [1]. Turk et al. found that the average time for disappearance of extruded discs in MRI was 26 weeks [2]. But they noted that the patients continued to be symptomatic and even with deficits in spite of radiological improvement. Spontaneous regression was more common in sequestrated fragments than subligamentous discherniations. Chiu et al. found that the rate of complete resolution of discherniation was 43% for sequestrated discs and 15% for extruded discs [3]. The mechanisms behind the regression are dehydration, shrinkage, retraction and resorption by inflammation [4]. Phagocytosis by macrophages has been observed.
But the reports of spontaneous regression within a short term are few. Kim SG et al. described two male patients with clinical and radiological regression of lumbar discs in 3 months [5].Albayraket al. published a report of regression of L5-S1 discsequestration of a 32-year-old man in 14 days [6]. Kim ES et al. reported about a 58-year-old woman with a large L2-3 disc extrusion [7]. She underwent microdiscectomy after 2 months. But the expected disc fragment was not found. Immediate MRI showed the absence of the fragment.
Case Presentation
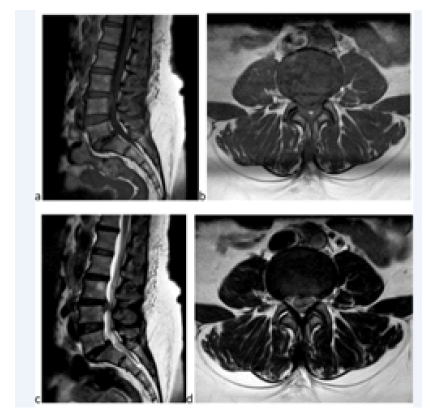
A 58-year lady presented with backache for 3 months, radiating to left leg, and weakness of left foot. She had severe pain 3 months back. A Magnetic Resonance Imaging (MRI) scan of lumbosacral spine was taken at that time. It showed L3-4 disc extrusion and canal stenosis and grade 1listhesis at L5-S1(Figures 1a-1d). Surgery was advised at that time. But the patient opted conservative treatment. She had significant improvement in symptoms.
Figure 1: (a) Sagittal T1-weighted MRI showing extrusion of L3-4 disc and grade 1 listhesis at L5- S1,(b) axial T1-weighted imaging showing extrusion of L3-4 disc, (c) sagittal T2-weighted MRI showing extrusion of L3-4 disc and grade 1 listhesis at L5-S1, (d) axial T2-weighted imaging showing extrusion of L3-4 disc and canal stenosis.
But she had recurrence of symptoms 10 days back. Straight leg raising test was positive at 40˚ on left side. Dorsiflexion was grade 4 on left side. Sensations of touch and vibration were reduced in L4 dermatomal region.
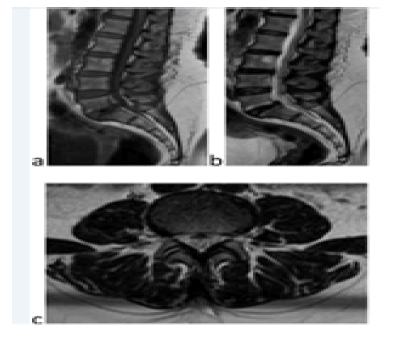
A repeat MRI scan was done to plan surgery. The disc extrusion at L3-4 had shrunk, with the residual listhesis at L5-S1(Figures 2a-2c). She was given another trial of conservative treatment with gabapentin, methylcobolamine, and physiotherapy. She improved over 1 week in pain, power, and sensation.
Discussion
Spontaneous regression of herniated lumbar discs over a course of time is well documented in literature. But the concomitant relief of symptoms is not seen always. The reports of regression within 3 months are a few. Kim ES et al reported about the peroperative identification of regression of an extruded disc fragment. But in this case, it was detected prior to surgery with a repeat MRI. So an unwanted surgery was avoided [7]. The probable mechanism of shrinkage may be either dehydration or resorption by inflammation, since the axial T2- weighted image shows a hypointense wrinkled fragment (Figure 2c). The knowledge of shrinkage of the extrusion helped in improvement of her symptoms, since psychological factors seem to play a major role in the outcome of low back pain as in the literature [8].
So, it is better to do a repeat imaging before planning surgery for a patient with a prior diagnosis of disc herniation. Thus an unnecessary surgery can be avoided.
Declarations
Funding
No external funding
Data availability
Not deposited.
Consent for publication
Informed consent was obtained for publication of details in anonymised manner.
Authors' contributions
Treated the patient and prepared the manuscript.
Competing interests
Nothing to be disclosed regarding funding or research support, employment , personal financial interests, stocks or shares in companies, consultation fees, patents, personal or professional relations with organizations and individuals, or regarding unpaid membership in a government or non-governmental organization. I am not one of the editorial board members or a reviewer of this journal.
Ethical approval
Obtained for retrospective analysis.
Acknowledgement
Nothing to be acknowledged
References
- Kesikburun B, Eksioglu E, Turan A, et al. Spontaneous regression of extruded lumbar disc herniation: Correlation with clinical outcome. Pak J Med Sci. 35(4):974-80(2019).
- Turk O, Antar V, Yaldiz C. Spontaneous regression of herniated nucleus pulposus: The clinical findings of 76 patients. Medicine. 98(8):e14667(2019).
- Chiu CC, Chuang TY, Chang KH, et al. The probability of spontaneous regression of lumbar herniated disc: a systematic review. ClinRehabil. 29(2):184-95(2015).
- Cunha C, Silva AJ, Pereira P, et al. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther. 20(1):251(2018).
[Google Scholar] [Crossref]
- Kim SG, Yang JC, Kim TW, et al. Spontaneous regression of extruded lumbar disc herniation: three cases report. Korean J Spine. 10(2):78-81(2013).
- Albayrak S, Durdağ E, Atçı İB, et al. Rapid Spontaneus Regression of Lumbar Disc Herniation Accompanying Neurological Recovery: Case Report. J Phys Med Rehabil Sci. 15(3):89-91(2012).
[Google Scholar] [Crossref]
- Kim ES, Oladunjoye AO, Li JA, et al. Spontaneous regression of herniated lumbar discs. J ClinNeurosci. 21(6):909-13(2014).
- Pincus T, McCracken LM. Psychological factors and treatment opportunities in low back pain. Best Pract Res ClinRheumatol. 27(5):625-35(2013).