Editorial - Research on Chronic Diseases (2023) Volume 7, Issue 3
A Review on dentistry and oral medicine and Impact of Common Oral Health
Wei Kurano*
College of Auxologico IRCCS, Department of biological Science of Japan Universitya
College of Auxologico IRCCS, Department of biological Science of Japan Universitya
E-mail: welkurano@gmail.com
Received: 01-5-2023, Manuscript No. oarcd-23-99537; Editor assigned: 03-5-2023, Pre QC No. 99537; Reviewed: -17-5-2023, QC No. 99537; Revised: 23-5-2023, Manuscript No. oarcd-23-99537 (R); Published: 30-5-2023; DOI: 10.37532/ rcd.2023.7(3).054-056
Abstract
Although maintaining oral health is definitely challenging and different in old age, oral health is not distinct from general health. Even though only a small number of elderly people have physical or mental conditions that necessitate a special interest in the dental office, one should not assume that all elderly people share these conditions. Understanding a few aspects of old age is necessary to achieve health. Tissues in the body become harder with age, and the accumulation of waste products in cells and the loss of lubrication impair the functions of various organs. The plan and execution of far reaching preventive dentistry conventions for seniors gives the dental calling many difficulties. Even though a specific protocol must be tailored to each patient’s specific requirements, there are some elderly-specific factors that may influence these protocols. Periodontal disease and dental caries, particularly root caries, are two of the most common oral diseases among them. Frequently, these systemic issues are connected to these oral diseases. Meta-examination detailed diabetes expands the rate and movement of periodontitis by 86%. Older adults who take multiple medications frequently experience a decrease in salivary output. According to a review, a low resting pH and a low stimulated salivary flow rate raise the risk of dental caries in older adults by 60%. Dementia and depression affect a lot of older people, making it harder to provide dental care. Legitimate oral cleanliness practice and dental consideration at prostrate position are frequently hard to be completed in the event that they have rheumatoid joint pain. With the rising need of old dental consideration, dental specialists and other dental staff ought to comprehend joined oral and general wellbeing to give an effective dental consideration plan for more seasoned grown-ups. The point of this study is to give an outline of the normal ailments and dental issues and their effects on more established grown-ups.
Keywords
Elderly • Oral health • Home dentistry tooth loss • Older adults
Introduction
Ongoing non-transmittable infections are becoming normal since individuals have a more drawn out life range. Older adults are more prone to oral diseases due to these chronic conditions and degenerative changes [1]. Systemic diseases like diabetes increase the incidence and progression of periodontitis by 86%, while rheumatoid arthritis and other diseases make it difficult to practice oral hygiene [2]. Multiple non-communicable diseases can have negative effects on oral health, with xerostomia being the most common issue. Other oral issues like dental caries, periodontal disease, and infections are also linked to xerostomia. Caries and periodontal disease may eventually result from the increased risk. However, there are oral and systemic diseases that are intertwined [3]. Since the constant fundamental infections and their therapy can expand the gamble of oral issues and interrelationship has been found among a few fundamental and oral issues, dental experts ought to refresh with the ongoing information about normal ailments of more seasoned grown-ups and their effects on the oral cavity [4]. In order to provide elderly patients with safe and effective dental care, they should be aware of the connection between oral and systemic diseases and the complexities of aging-related changes. Dentists should also work with other medical professionals to tailor dental care to the needs and health conditions of the elderly [5]. The purpose of this review is to provide a summary of the most common medical conditions and dental issues that affect older adults [6]. Aging is a normal part of life. Advanced age ought to be viewed as a typical, unavoidable natural peculiarity. In the second half of the 20th century, advances in medicine and public health measures led to a significant increase in man’s lifespan [7]. During the latter half of the 20th century, the age composition of the population changed dramatically, with more people living to older ages and the older population getting older. As a result, elderly people (those over 65) have health issues that require special consideration. The providers of general and oral health care, as well as the delivery of these services, will be significantly impacted by this demographic shift [8]. Even though some older adults have physical and/or psychological conditions that necessitate special care in a dental office setting, it is not necessary to assume that all older adults have these conditions. People over the age of 60 make up 76 million of India’s over one billion inhabitants, or 7.6% of the country’s total population. India has the highest incidence of oral cancer, a disease of old age [9]. The presence of systemic disease, which not only affects the patient’s ability to maintain oral hygiene and promote oral health but may also be linked to the occurrence of certain oral diseases, may also be cause for concern. However hindrances are not hazardous, they influence an individual’s personal satisfaction. Consequently, arranging therapy for the senior dental patient incorporates a comprehension of the constant illnesses the patient lives with every day, as this assume a basic part in the acknowledgment and outcome of the dental treatment plans [10].
Impact of common oral health
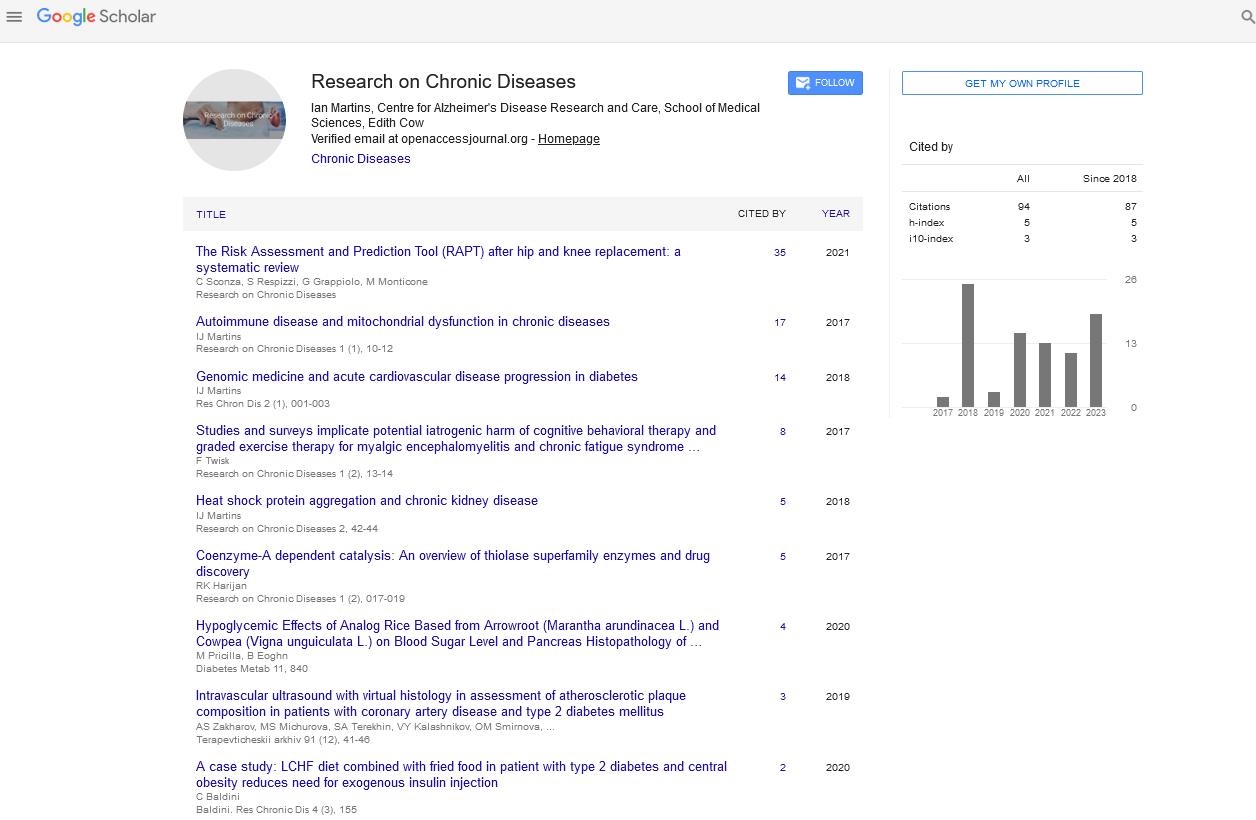
On current global oral and systemic health issues, the authors relied on information from the World Health Organization’s websites. They additionally utilized PubMed and Google Researcher data sets to recognize writings in English including precise audits, meta-examination, surveys and clinical examinations on normal clinical and dental issues of more seasoned grown-ups with no time limitation. Although this study developed an updated global oral and systemic health issues based on the information provided by the World Health Organization and two of the most common databases, the included literature may not be comprehensive because it is a narrative review. However, this study identified six prevalent systemic diseases that are common causes of morbidity and mortality and increase with age. In three to four months, periodontal therapy and good home oral health care helped type 2 diabetic patients improve their glycemic control, according to studies. It demonstrates the significance of good oral hygiene practices for this patient group. According to the findings of each of these studies, diabetes and periodontitis are linked in two ways, and how well they are controlled affects one another. Oral cleanliness care is significant for them not exclusively to forestall periodontal infection yet in addition for better glycemic control.
Hypertension is perhaps of the most widely recognized cardiovascular condition, which can cause heart disappointment and stroke whenever left untreated. The condition affects more than a billion people worldwide. Anti-hypertensive medications, such as diuretics, calcium channel blockers, beta-blockers, angiotensin-converting enzyme inhibitors, alpha 2 blockers, and angiotensin II receptor blockers, are the primary cause of oral manifestations of hypertension. Dry mouth, gingival hyperplasia, lichenoid reactions, and altered taste are the most common oral cavity side effects of these medications. These side effects can primarily be treated by addressing the symptoms, such as increasing fluid intake for dry mouth patients or receiving localized periodontal therapy for gingival hyperplasia patients.
Conclusion
The significant block in oral medical services of old and the occupants would be the misjudgment of the oral medical care need by them. The residents’ dental care is typically limited to treating emergencies and does not aim to retain teeth. On the other hand, the goal of oral health should include: Keeping their teeth, keeping their teeth solid and keeping their teeth pretty. Home dentistry or domiciliary dental care” would be the best option for serving the locals, but it is still uncommon in India. In this sector, surveys should be conducted frequently to identify residents who require oral care in nursing homes, ashrams, senior living communities, secure units, and community households. Oral and general wellbeing are interrelated and now and then in a bidirectional relationship. Diseases like diabetes, high blood pressure, rheumatoid arthritis, Alzheimer’s, Parkinson’s, and depression are common ailments that get worse with age. Older adults are more likely to develop oral conditions like periodontal disease, dental caries, and even oral precancerous and cancerous lesions because of these systemic diseases and the medications for them. Degenerative changes in older people get worse as they get older. Numerous of them have significant dental and medical issues. They might experience the ill effects of xerostomia and tooth wear. Their systemic issues are frequently connected to their oral conditions and diseases. In order to meet the growing demand for dental care for the elderly, dentists should keep up with the latest techniques and knowledge in geriatric dentistry.
References
- Suddick, RP, Harris. Historical perspectives of oral biology: a series. Critical Reviews in Oral Biology and Medicine. 1, 135-151(1990).
- Gambhir RS. Primary care in dentistry – an untapped potential. Journal of Family Medicine and Primary Care. 4, 13-18(2015).
- Pastore L, Carroccio A, Compilato D et al. Oral manifestations of celiac disease. J Clin Gastroenterol. 42, 224-232 (2008).
- Slavkin, Harold C. Evolution of the scientific basis for dentistry and its impact on dental education: past, present, and future. Journal of Dental Education. 76, 28-35(2012).
- Leggat PA. Occupational hygiene practices of dentists in southern Thailand. International Dental Journal. 51, 11-16(2001).
- Gelbier, Stanley. Dentistry and the University of London. Medical History. 49, 445-462(2005).
- Capper S. Book Review: Silent Victories: The History and Practice of Public Health in Twentieth-Century America. Inquiry. 44, 128-129(2007).
- Le P, Dempster L, Limeback H et al. Improving residents' oral health through staff education in nursing homes. Special Care in Dentistry. 32, 242-50(2012).
- Lennon MA. One in a million: the first community trial of water fluoridation. Bulletin of the World Health Organization. 84, 759-760(2006).
- Leggat PA. Occupational Health Problems in Modern Dentistry: A Review. Industrial Health. 45, 611-621 (2007).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref