Research Article - Interventional Cardiology (2018) Volume 10, Issue 3
Achieving the Recommendations of International Guidelines in STelevation Myocardial Infarction Patients after Start of an OffSite Percutaneous Coronary Intervention Centre and a Network Focus Group: More Attention Must be Paid to PreHospital Delay
- Corresponding Author:
- K.A. Mol
Department of Cardiology VieCuri Medical Centre Venlo, the Netherlands
Tel:0773205555
Email: kmol@viecuri.nl
Received date: May 21, 2018; Accepted date: June 07, 2018; Published date: June 14, 2018
Abstract
Objective: Delays in the treatment of patients with ST-segment elevation myocardial infarction (STEMI) are still substantial and achieving the guideline recommendations is challenging. Specifically pre-hospital delays, including general practitioner (GP) and emergency medical transport (EMT) receive little scientific attention. Our objective is to achieve the international guideline recommendations for pre-hospital delay in STEMI patients.
Methods: This is a prospective, observational, cohort study evaluating the delays of STEMI patients. To diminish delays within the studied region an off-site percutaneous coronary intervention (PCI) centre and an acute coronary syndrome focus group comprising the Cardiology Departments, EMT service and GPs were set up. Delays before and after the start of the off-site PCI centre and focus group were analysed.
Results: The median system delay (from any first medical contact to start of PCI) significantly decreased from 80 to 65 minutes. Median electrocardiogram-to-PCI delay decreased from 64 to 48 minutes. The percentage of patients with a system delay <90 minutes improved from 73% to 85% and the percentage with an electrocardiogram-to-PCI delay <90 minutes improved from 92% to 96%. GPs play an important role within the STEMI network with 45% of the patients contacting the GP first, resulting in a slight increase in delays compared to EMT as first medical contact.
Conclusion: The guideline recommendations are achieved within the studied region after start of an off-site PCI centre and a focus group including Cardiologists, GPs and EMT service, demonstrating that focussed attention can effectively result in a decrease in pre-hospital delays
Keywords
STEMI; General practitioner; Percutaneous coronary intervention and Emergency medical services
Introduction
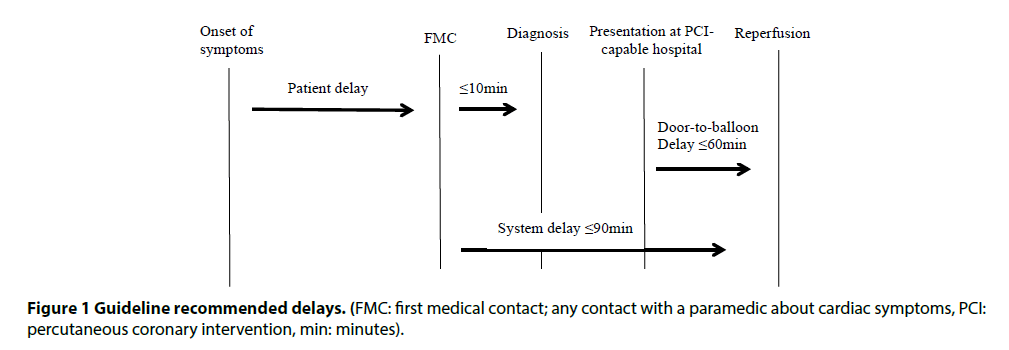
Delays in the treatment of patients with ST-segment elevation myocardial infarction (STEMI) should be kept as short as possible to limit extend of necrosis and to decrease the risk of heart failure and mortality [1,2]. Percutaneous coronary intervention (PCI) is the preferred reperfusion therapy in STEMI patients, if performed within guideline recommended timeframes. The guidelines advise that at least 90% of STEMI patients should have a system delay of 90 minutes or less. Other recommended delays are depicted in Figure 1 [3].
Despite decreased door-to-balloon as well as diminished emergency medical transport (EMT) delays [4], the recommendations in the guidelines are rarely met [5,6]. Most studies define the FMC as first ECG [1,7-9], neglecting the time from first call to the arrival of a paramedic or general practitioner (GP) and the triage of the EMT service. Contacting a GP first can increase the delay in reperfusion up to 95 minutes [10] and as studies report that 37% to 75% of STEMI patients contact a GP [11,12]; this is an important point of focus. It is recommended that the entire network involved in triage, transport and treatment of STEMI patients should work closely together [7,13].
To meet the increased demand of PCIs and to decrease the pre-hospital delays a focus group comprising of the Cardiology departments, EMT service and GPs was set up and an off-site PCI centre was started [14]. Off-site PCI centres, with no surgical back-up in the own hospital, have been proven to be safe [15,16], if they have high operator and intuitional volumes [17]. This study evaluates the effect of starting an off-site PCI centre and a focus group on the delays of STEMI patients.
Methods
Study design
This study is a prospective, observational, cohort study. To achieve the recommended delays in STEMI patients from North and Middle Limburg, the Netherlands, the Cardiology departments, EMT service (Ambulance Zorg Limburg Noord), and GPs (Cooperation Cohesie), set up the Acute Coronary Syndrome-Limburg North (ACS-LN) focus group. This focus group designed a protocol for the assessment and treatment of ACS patients (Supplementary Figure 1). They devised a questionnaire requesting time points in the STEMI network, filled in by EMT personnel, to evaluate the delays and protocol use. To limit the influence of human error, time stamps were used as much as possible. Data from patients, who were referred directly to the emergency department (ED), without any use of EMT, were retrospectively retrieved from the medical files. The system delay was defined as FMC to the start of the PCI procedure. The FMC was any contact with a paramedic about cardiac symptoms, including GPs, EMT and the ED.
The mortality of the study population was compared to the Thrombolysis in Myocardial Infarction (TIMI) risk score study [18].
Setting and population
All consecutive patients with a STEMI from North Limburg referred to a PCI-capable centre for primary PCI were included from June first 2011 until November first 2015. Until September 2013 the STEMI patients were referred to Catharina Hospital Eindhoven, the Netherlands, at that time the closest primary (on-site) PCI-capable hospital. In September 2013 VieCuri Medical Centre Venlo, the Netherlands, started as an off-site PCI centre, bypassing the 60 km transport of STEMI patients. This off-site PCI centre performs more than 1200 PCIs per year. The patient group who underwent their PCI at Catharina Hospital Eindhoven (the on-site group) and the patient group who underwent their PCI at VieCuri Medical Centre Venlo (the off-site group) all came from the same region (North Limburg), therefore the results given are not a representation of the system delay of Catharina Hospital Eindhoven.
Patients with an out-of-hospital resuscitation were excluded. STEMI patients treated with shocks for ventricular tachycardia or fibrillation from the EMT and/ or hospital with rapid conscience recovery were included.
Statistical analyses
All data were collected by an independent investigator and analysed with SPSS version 22. The categorical data are presented as number of patients and percentages. Continuous data are presented as means and standard deviations (SD) in case of normally distributed data and as medians and interquartile ranges (IQR) in case of skewed data. Patients with (some) missing data were included for analysis of non-missing values. Missing data were not replaced and are given per variable in the tables. The Student t-test was used for normally distributed continuous variables and the Mann-Whitney U-test was used for skewed distributed continuous variables. Categorical variables were analysed using a chi-square test. To check for possible confounding we analysed whether baseline variables that differed between the two groups (on-site and off-site group) correlated with the delays using the Pearson’s correlation coefficient.
A p-value of less than 0.05 was considered significant.
Results
Baseline
A total of 227 patients were included from June first 2011 until September first 2013 who were referred to Catharina Hospital Eindhoven for primary PCI (the on-site group) and 339 patients were included from September first 2013 until November first 2015 who were referred to VieCuri Venlo (the off-site group). Baseline characterisations are presented in Table 1. Gender, presentation during office hours, mortality and TIMI score were not significantly different between the groups. The patients referred to the off-site centre were significantly older (63 years and 62 years respectively), though there was no correlation found between age and the delays.
| On-site | Off-site | P-value | |
|---|---|---|---|
| Study population, n | 227 | 339 | - |
| Male gender, n (%) | 164 (72,2%) | 239 (70,5%) | 0,653 |
| Age, years (SD) | 62,0†(13,8) | 63,3†(12,7) | 0,036 |
| Presentation during office hours, n (%) | 76 (35,5%) | 133 (39,5%) | 0,160 |
| Mortality 30 day, n (%) | 6 (2,6%) | 7 (2,1%) | 0,578 |
| TIMI score, (IQR) | 2,2*(5,7) | 2,2*(5,7) | 0,310 |
TIMI: Thrombolysis in Myocardial Infarction risk score, SD: standard deviation
*median,
†mean
Table 1 Baseline characteristics
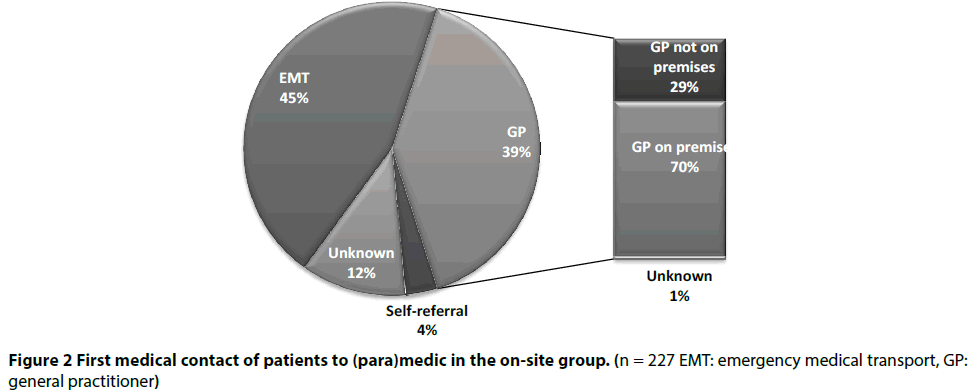
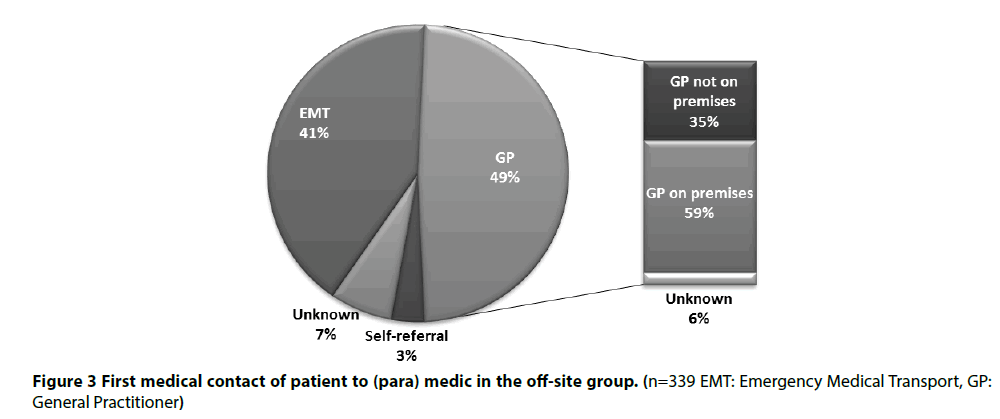
The FMC of the patients did not differ significantly between the two groups (Figures 2 and 3).
Guidelines adherence
The system delay, i.e. FMC to start PCI, significantly decreased from 80 minutes to 65 minutes. The delay between ECG diagnosis to the start of the PCI procedure, was also significantly lower in the off-site group (Table 2).
Patients contacted the GP more often in the offsite group than in the on-site group, namely 49% vs. 39%, although this difference was not significant. The delays associated with the GP did not differ either. The EMT delay, i.e. the time from calling the EMT until ambulance arrival, did increase from 8 to 9 minutes (Table 2). When comparing FMC as GP vs. FMC as EMT over the whole group (on- and off-site groups combined) the system delay was 68 min vs. 75 min (p=0,012).
| On-site | n (missing) | Off-site | n (missing) | P-value | |
|---|---|---|---|---|---|
| System delay: FMC until PCI start, min (IQR) | 80*(20) | 131 (96) | 65*(25) | 265 (74) | <0.001 |
| Percentage FMC until PCI start <90 min | 73.3% | 131 (96) | 85.3% | 265 (74) | 0.004 |
| ECG until PCI start, min (IQR) | 64*(19) | 147 (37) | 48*(19) | 302 (37) | <0.001 |
| Percentage ECG until PCI start <90 min | 89.1% | 147 (37) | 93.0% | 302 (37) | 0,155 |
| ECG until Cath lab, min (IQR) | 55*(18) | 195 (32) | 39*(22) | 298 (41) | <0.001 |
| GP | |||||
| Call-to-GP until GP- call-to-EMT, min (IQR) | 5*(18) | 63(19) | 5*(19) | 84 (53) | 0,447 |
| Call-to-GP until GP-call-to-EMT with GP on premises, min (IQR) | 10*(24) | 40 (17) | 9*(23) | 50 (35) | 0,523 |
| Call-to-GP until ECG diagnosis, min (IQR) | 20*(20) | 65 (17) | 25*(20) | 85 (52) | 0,206 |
| EMT | |||||
| Call-to-EMT until ambulance arrival, min (SD) | 8†(3) | 147 (31) | 9†(4) | 264 (6) | <0.001 |
| Call-to-EMT until ECG diagnosis, (IQR) | 13*(6) | 153 (25) | 15*(8) | 243 (27) | <0.001 |
| Departure-to- and arrival-at-Cath lab, (IQR) | 35*(10) | 140 (38) | 22*(15) | 252 (18) | <0.001 |
| Patient delay | |||||
| Patient delay: symptom onset to FMC, min (IQR) | 47*(98) | 161 (66) | 58*(190) | 237 (102) | 0,096 |
| Patient delay when FMC is GP, min (IQR) | 67*(141) | 66 (25) | 74*(207) | 96 (69) | 0,337 |
| Patient delay when FMC is not GP, min (IQR) | 32*(76) | 95 (15) | 42*(163) | 141 (10) | 0,098 |
Values are minutes or n
FMC: first medical contact; any contact with a (para)medic about cardiac symptoms, PCI: percutaneous coronary intervention, ECG:
electrocardiogram, Cath lab: catheterization laboratory, IQR: interquartile range, GP: general practitioner, EMT: emergency medical
transport
*median
†mean
Table 2 Delays
The off-hour presentation was not different between the groups and is therefore presented for both groups together. The overall delay in the off-hours did not significantly differ from the delay during daytime. Moreover the GP delay also did not differ between offhours and daytime (Table 3).
| Off-hour | n (missing) | On-hour | n (missing) | P-value | |
|---|---|---|---|---|---|
| System delay, min (IQR) | 70*(24) | 250 (104) | 72*(35) | 146(63) | 0,915 |
| System delay with FMC is GP, min (IQR) | 75*(35) | 84(48) | 77*(38) | 79(44) | 0,968 |
Values are minutes or n FMC: first medical contact; any contact with a (para)medic about cardiac symptoms, GP: general practitioner, IQR: interquartile range *median
Table 3 Off-hour presentation delay
Patient delay
The median patient delay was longer in the off-site group, although this difference was not significant (Table 2). The mean delay of the groups combined is almost 3 h (170 minutes) with 6% of the patients waiting more than 12 h before contacting a paramedic.
Patients contacting the GP waited significantly longer to contact a paramedic, than patients contacting the EMT directly.
Discussion
The most important finding in our study is that the guideline recommended system delays in STEMI patients were achieved. With the close collaboration of the entire ACS network involved in triage, transport and treatment of STEMI patients and the start of an off-site PCI centre the delay in STEMI patients has decreased. The system delay in our region from any FMC to initiation of PCI is 68 minutes, a much lower delay than reported in other studies [2,5,19]. Most studies moreover report ECG to initiation of PCI as system delay, varying from 60 to 210 minutes [7,20]. In our study we achieved a median ECG to initiation of PCI delay of only 48 minutes.
The percentage of patients with a system delay of 90 minutes or less also improved significantly from 73% to 85%, and thus the target of 90% is almost reached. When using the more frequently applied definition of system delay, from ECG to initiation of PCI, more than 90% of the patients are treated within 90 minutes, thereby reaching target. This is much higher than the 22% to 82% reported in other studies [5-8]. The mortality and TIMI scores of the two groups were identical and, as published before, the occurrence of procedural complications and MACE were low with no significant differences [21].
General practitioner
The findings in our study show that patients contacted the GP frequently with 39% in the on-site group and 49% in the off-site group, a non-significant difference. This is comparable to previous studies with 37 to 75% of the STEMI patients consulting the GP [10-12]. Within the study period the number of GP visits decreased over time: the GPs visited 74% of the patients who contacted the GP in the on-site group (from June first 2011 to September first 2013) and only 59% of the patients in the off-site group (from September first 2013 to November first 2015). This (non-significant) decrease might be due to the recent recommendation of the cardiac guidelines that STEMI patients should bypass the GP when experiencing chest pain [3].
The system delay was slightly, though significantly, longer when the GP was consulted first rather than the EMT (68 vs 75 min). These delays are lower than the delays in other studies [11,12]. Which might be a consequence of the recommendation within the cardiac guidelines to diminish GP participation within the network [3,22]. To advise all patients with chest pain to contact the EMT, and thus bypassing the GPs entirely in the STEMI network is not feasible, as not all patients with chest pain have a STEMI or even ACS. Up to 80% of the patients within the primary care setting with chest pain do not have ACS and therefore without GP triage the EMT and hospitals would be overcrowded [23].
As this study shows that the guidelines can be achieved with GP involvement, we recommend regular meetings with all participants in the ACS network including Cardiology departments, EMTs and GPs to improve the delays in STEMI patients, but not dismiss GPs from the ACS network.
Emergency transport delay
The EMT delay was low with 8 and 9 minutes response time, well within the recommended target of 15 minutes [24]. Although the one minute increase was statistically significant, it is unlikely to be clinically relevant. Possible explanations of this difference could be the changes in shift hours and ambulance locations during the study.
Off-hour presentation
Off-hour presentation of STEMI patients is reported to be associated with longer delays and higher mortality [25]. In our study, off-hour presentation did not result in significant longer delays. Off-hour presentation to a GP also did not significantly delay PCI. Studies suggest that the delaying factor of off-hour presentation can be improved with a multidisciplinary and protocol driven network with a high-volume PCI-centre [26,27], as is the case in our region.
Patient delay
The above mentioned delays are all organization related delays; however a crucial part of the pre-hospital delay includes patient delay. In this study we have found median patient delays of 47 and 58 minutes, a non-significant increase and lower than reported in previously published studies [28,29]. However a small group of patients waited more than 12 h making the mean delay almost three hours, a substantial delay which needs to be diminished.
Patients contacting the GP, waited longer to call for help, than patients contacting the EMT. Patients contacting the GP might have less typical symptoms, not recognize a heart attack and thus not contact the EMT immediately. This could increase the GP delay as well, as it is more difficult to diagnose these patients.
Reducing the patient delays has proven to be complex, with most studies not leading to a reduction of the delays [29,30]. The patient delays depicted in this study are much lower than the earlier studies and comparable to other, more recent studies [19]. There may be improvements within patient delay that have already taken place, such as increased awareness. However, as any delay increases the risks and some patients wait more than twelve hours, these delays are too long, and should still be a point of focus.
Conclusion
This study shows that the delays of STEMI patients can be improved by focussing on pre-hospital delays and thus achieving the recommended delays in the guidelines. The guideline recommendations are met within the studied region after the start of an off-site PCI centre and with a multidisciplinary and protocoldriven network, including the Cardiology departments, GPs and EMT service.
Strengths and Limitations
The strength of our study is that we included the FMC to any (para) medic, as most other studies do not report the pre-hospital delays before ECG. Missing data, mainly due to handwritten forms, are a limitation. Patients with a STEMI but not referred to the hospital are not part of this study. Patients with out-of-hospital resuscitation were excluded, however these patients also benefit of decreased delays and more research should be conducted within this group.
Acknowledgements
We would like to thank the EMT service Limburg North and Middle, the GPs at Cohesie and the Cardiology Department of Laurentius Hospital Roermond for the collaboration within the focus group. We would like to give special thanks to the EMT service for providing data. We would also like to thank the Department of Cardiology at the Catharina Hospital Eindhoven for their support.
Funding
The authors received no financial support for the research.
Conflict of Interests
None declared
References
- Koul S, Andell P, Martinsson A, et al. Delay from first medical contact to primary PCI and all-cause mortality: a nationwide study of patients with ST-elevation myocardial infarction. J Am Heart Assoc. 3(2): e000486 (2014).
- Terkelsen CJ, Sorensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 304(7): 763-71 (2010).
- Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 33(20): 2569-619 (2012).
- Nam J, Caners K, Bowen JM, et al. Systematic review and meta-analysis of the benefits of out-of-hospital 12-lead ECG and advance notification in ST-segment elevation myocardial infarction patients. Ann Emerg Med. 64(2): 176-86 (2014).
- Helve S, Viikila J, Laine M, et al. Trends in treatment delays for patients with acute ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. BMC Cardiovasc Disord. 14:115 (2014).
- Sandouk A, Ducasse JL, Grolleau S, et al. Compliance with guidelines in patients with ST-segment elevation myocardial infarction after implementation of specific guidelines for emergency care: results of RESCA+31 registry. Arch Cardiovasc Dis. 105(5): 262-70 (2012).
- Tra J, van der Wulp I, de Bruijne MC, et al. Exploring the treatment delay in the care of patients with ST-elevation myocardial infarction undergoing acute percutaneous coronary intervention: a cross-sectional study. BMC Health Serv Res. 15: 340 (2015).
- Vermeulen RP, Jaarsma T, Hanenburg FG, et al. Prehospital diagnosis in STEMI patients treated by primary PCI: the key to rapid reperfusion. Neth Heart J. 16(1): 5-9 (2008).
- Boer MJ, Zijlstra F. STEMI time delays: a clinical perspective: Editorial comment on the article by Verweij et al. Neth Heart J. 23(9): 415-9 (2015).
- Bleeker JK, Simoons ML, Erdman RA, et al. Patient and doctor delay in acute myocardial infarction: a study in Rotterdam, The Netherlands. Br J Gen Pract. 45(393): 181-4 (1995).
- Birkhead JS. Time delays in provision of thrombolytic treatment in six district hospitals. Joint Audit Committee of the British Cardiac Society and a Cardiology Committee of Royal College of Physicians of London. BMJ. 305(6851): 445-8 (1992).
- Hitchcock T, Rossouw F, McCoubrie D, et al. Observational study of prehospital delays in patients with chest pain. Emerg Med J. 20(3): 270-3 (2003).
- NVVC Connect [Available from: http://www.nvvcconnect.nl/.
- Mol KA, Rahel BM, Eerens F, et al. The first year of the Venlo percutaneous coronary intervention program: procedural and 6-month clinical outcomes. Neth Heart J.21(10): 449-55 (2013).
- Peels JO, Hautvast RW, Swart JB, et al. Percutaneous coronary intervention without on site surgical back-up; two-years registry of a large Dutch community hospital. Int J Cardiol. 132(1): 59-65 (2009).
- Ting HH, Raveendran G, Lennon RJ, et al. A total of 1,007 percutaneous coronary interventions without onsite cardiac surgery: acute and long-term outcomes. J Am Coll Cardiol. 47(8): 1713-21 (2006).
- Dutch guidelines for interventional cardiology. 2016 [Available from: https://www.nvvc.nl/media/richtlijn/188/2016_Praktijkdocument_interventiecardiologie.pdf.
- Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 284(7): 835-42 (2000).
- Thilo C, Bluthgen A, Scheidt W. Efficacy and limitations of a STEMI network: 3 years of experience within the myocardial infarction network of the region of Augsburg - HERA. Clin Res Cardiol. 102(12): 905-14 (2013).
- Widimsky P, Wijns W, Fajadet J, et al. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur Heart J. 31(8): 943-57 (2010).
- Koolen K, Mol KA, Rahel BM, et al. Off-site primary percutaneous coronary intervention in a starting centre is safe: comparing clinical outcomes with a hospital with surgical backup. Neth Heart J. 24(10): 581–588 (2016).
- Rutten F, Backx JC, Bruins Slot, et al. NHG-Standaard Acuut coronair syndroom (eerste herziening). 10-02-2016
- Mol KA, Rahel BM, Meeder JG, et al. Delays in the treatment of patients with acute coronary syndrome: Focus on pre-hospital delays and non-ST-elevated myocardial infarction. Int J Cardiol. 221: 1061-6 (2016).
- Rijksinstituut voor Volksgezondheid en Milieu [Available from: www.volksgezondheidenzorg.info.
- Sorita A, Ahmed A, Starr SR, et al. Off-hour presentation and outcomes in patients with acute ischemic stroke: a systematic review and meta-analysis. Eur J Intern Med. 25(4): 394-400 (2014).
- Casella G, Ottani F, Ortolani P, et al. Off-hour primary percutaneous coronary angioplasty does not affect outcome of patients with ST-Segment elevation acute myocardial infarction treated within a regional network for reperfusion: The REAL (Registro Regionale Angioplastiche dell'Emilia-Romagna) registry. JACC Cardiovasc Interv. 4(3): 270-8 (2011).
- Sorita A, Lennon RJ, Haydour Q, et al. Off-hour admission and outcomes for patients with acute myocardial infarction undergoing percutaneous coronary interventions. Am Heart J. 169(1): 62-8 (2015).
- Naegeli B, Radovanovic D, Rickli H, et al. Impact of a nationwide public campaign on delays and outcome in Swiss patients with acute coronary syndrome. Eur J Cardiovasc Prev Rehabil. 18(2): 297-304 (2011).
- Tummala SR, Farshid A. Patients' understanding of their heart attack and the impact of exposure to a media campaign on pre-hospital time. Heart Lung Circ. 24(1): 4-10 (2015).
- Neubeck L, Maiorana A. Time to get help? Acute myocardial infarction and delay in calling an ambulance. Heart Lung Circ. 24(1): 1-3 (2015).