Case Report - Imaging in Medicine (2017) Volume 9, Issue 2
Acute achilles tendon rupture sustained during exertional squash play
Mohamud A Verjee*Associate Professor of Family Medicine in Clinical Medicine Doha, Qatar
- Corresponding Author:
- Mohamud A Verjee
Associate Professor of Family Medicine in Clinical Medicine Doha, Qatar
E-mail: mov2002@qatar-med.cornell.edu
Abstract
The Achilles tendon or heel cord, also commonly known as the calcaneal tendon, is a thickest tendon of the back of the leg in the human body. It serves to connect the plantaris, gastrocnemius (calf) and soleus muscles to the calcaneus (heel) bone. These muscles, acting by means of the tendon, cause plantar flexion of the foot at the ankle, and (aside from soleus) flexion at the knee. Achilles tendon rupture is the point at which the achilles tendon breaks. The achilles is the most commonly injured tendon. A break can happen while performing activities requiring increasing acceleration, for example, pushing off or jumping. The male to female proportion for Achilles tendon break fluctuates in the vicinity of 7:1 and 4:1 across various studies.
Keywords
achilles tendon open reparative surgery post-operative infections
Introduction
The largest and strongest tendon in the body is involved in all foot movements. Constant tendon flexion and extension occurs without a second thought in walking, running or jumping. Preparation for vigorous exercise is not a first thought for the occasional sportsman, especially in squash [1]. Sudden tendon contraction due to rapid acceleration can place extreme force with movement following a single step. The soleus and gastrocnemius muscles are part of the contraction anatomy. The blood supply at the union of these two muscles, 2.16 cm above their insertion, is the weakest point [2]. A tear or rupture is most commonly at this site with the resulting loss of plantar flexion. Studies show an incidence of about 7 per 100,000 in the general population [3]. Approximately 10% of all Achilles tendon injuries have a pre-existing tendon disorder [4].
Case study
A 54 year old obese man playing squash could not continue after he felt a “snap” in his right lower leg, with acute severe pain in his lower leg and heel. An Emergency Department physician confirmed a diagnosis of an acute right Achilles tendon rupture and the patient subsequently underwent immediate open reparative surgery. No radiology reports were available. The patient was not at increased risk other reaching an age over 45 years and allowing for natural degeneration of tendinous tissue with time. There was no mention of soft tissue calcification being observed.
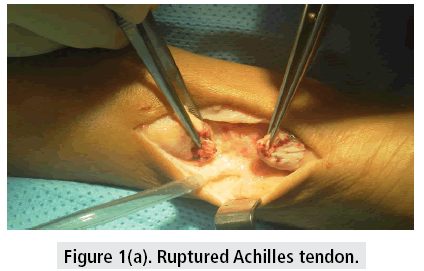
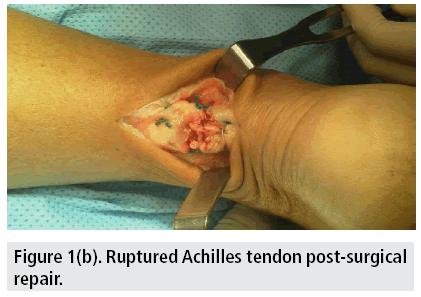
Post-surgical repair images are displayed. (FIGURES 1A-B) Outcomes are good in most cases where the tissue retains sufficient quality for suture repair.
Discussion
Autologous tendon transplants provide another repair method but with mixed recovery results with full rehabilitative physiotherapy. Lower leg incisions with primary repair now compete with percutaneous or minimally invasive surgery and endoscopy. Conservative approaches for example with an immobilizing cast are alternatives. Patients with co-morbidities such as diabetes mellitus with nerve degeneration, or rheumatological disorders e.g. psoriatic arthritis and ankylosing spondylitis accept such management plans [5]. While significant pain on occurrence is most usual, some injuries are painless, estimated at a third of all incidents. Patient delay in presenting to a physician impairs the better long-term outcomes.
Controversy still exists about techniques of surgical repair [6], the timing of surgery, the procedure to follow, age considerations, professional athletic status, and general fitness [7]. The patient may express wishes to return to the same sport so rehabilitation and graduated return to the game needs a particular protocol with appropriate advice. Some Achilles tendon ruptures, once repaired, are at risk of further damage, and even a quick repair may not restore normality. A valgus foot variant increases the risk of tendon damage with the exertion of high forces. Sudden fast movements and twisting or pivoting actions of the lower leg also add to the same risk. Longer-term oral steroids impact the predisposition to weaker tissue and ruptures [8].
While the peak incidence of damage is between 30-40 years, age above 45 years is a predisposing factor to tendon damage. However, less than 20% of all such injuries occur in athletes less than 45 years of age. Inelasticity and loss of tensile strength lead to progressive degeneration, accompanied by tendinopathy and a degree of shortening. Overuse, cold weather [9], poor footwear [10] increases the risk as well as in sedentary “weekend warrior” participation. Men are five times more likely than women to sustain Achilles tendon damage [3].
Major complications of Achilles tendon surgery include damaged nerves, post-operative infections causing wound healing delays and persistent pain on walking again [11]. The lower leg may not regain full muscle strength, and going down steps requiring plantar flexion may be more difficult.
Rehabilitative care after complete wound healing is best started soon with a gradual increase in mobilization according to ability. Patients need strengthening and stretching exercises in the form of concentric and eccentric prescriptions. Highly motivated patients have a better chance of returning to sporting activity with near normal functional leg restoration. A tear at the hypo-vascular point of the tendon may pre-empt full recovery [12].
The patient whose repair photos are shown made a full recovery from the aspect of pain, and regained normal walking. He preferred to use an elevator when possible although he managed a few steps at a leisurely pace. He lacked the confidence to return to playing squash. Given the higher chance of re-injury with his age with renewed tendon stress, he decided he would not risk further damage and was content to retire from the game. The general rule is that a return to sporting activity should not resume for at least six months after injury or surgical intervention. In the case of squash, rehabilitative exercises are essential to minimize the chance of a subsequent injury and a period of a year is advisable before a return to full-fledged play [13-15].
Acknowledgement
The photographs included were donated to the author for educational purposes, with fullunrestricted consent.
Conflict of interest
None
References
- Alfredson H, Lorentzon R. Chronic Achilles tendinosis: Recommendations for treatment and prevention. Sports. Med. 29, 135 (2000).
- Józsa L, Kvist M, Bálint BJ et al. The role of recreational sport activity in Achilles tendon rupture. A clinical, pathoanatomical and sociological study of 292 cases. Am. J. Sports. Med.17, 338 (1989).
- Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta. Orthop. Scand. 67, 277 (1996).
- Kujala UM, Sarna S, Kaprio J. Cumulative incidence of Achilles tendon rupture and tendinopathy in male former elite athletes. Clin. J. Sport. Med. 15, 133 (2005).
- Borman P, Koparal S, Babaoğlu S et al. Ultrasound detection of entheseal insertions in the foot of patients with spondyloarthropathy. Clin. Rheumatol. 25, 373 (2006).
- Choi GW, Kim HJ, Lee TH et al. Clinical comparison of the two-stranded and four-stranded double Krackow techniques for acute Achilles tendon injuries. Knee. Surg. Sports. Traumatol. Arthosc. (2016).
- Wilkins R, Bisson LJ. Operative versus non-operative management of acute Achilles tendon ruptures: A quantitative systematic review of randomized controlled trials. Am. J. Sports Med. 40, 2154 (2012).
- Holmes GB, Lin J. Etiologic factors associated with symptomatic Achilles tendinopathy. Foot. Ankle. Int. 27, 952 (2006).
- Milgrom C, Finestone A, Zin D et al. Cold weather training: a risk factor for Achilles paratendinitis among recruits. Foot. Ankle. Int. 24, 398 (2003).
- Leppilahti J, Korpelainen R, Karpakka J et al. Ruptures of the Achilles tendon: Relationship to inequality in length of legs and to patterns in the foot and ankle. Foot. Ankle. Int. 19, 683 (1998).
- Barp EA, Erickson JG. Complications of tendon surgery in the foot and ankle. Clin. Podiatr. Med. Surg. 33, 163-175 (2016).
- Spennacchio P, Vascellari A, Cucchi D et al. Outcome evaluation after Achilles tendon ruptures. A review of the literature. Joints. 4, 52-61 (2016).
- Brumann M, Baumbach SF, Mutschler W et al. Accelerated rehabilitation following Achilles tendon repair after acute rupture-Development of an evidence-based treatment protocol. Injury. 45, 1782-1790 (2014).
- Olsson N, Petzold M, Brorsson A et al. Predictors of clinical outcome after acute Achilles tendon ruptures. Am. J. Sports. Med. 42, 1448-1455 (2014).
- Horstmann T, Lukas C, Merk J et al. Deficits 10 years after Achilles tendon repair. Int. J. Sports. Med. 33, 474-479 (2012).