Research Article - Clinical Practice (2019) Volume 16, Issue 3
Adherence to treat to target strategy in rheumatoid arthritis: Development of a tool for it assessment
- Corresponding Author:
- Garcia Salinas Rodrigo
Rheumatology Unit, Hospital Italiano de La Plat
Buenos Aires, Argentina
E-mail: gsalinasrodrigo@gmail.com
Abstract
Introduction/Objective: The purpose of the treat to target (T2T) in Rheumatoid Arthritis (RA) is to achieve remission or Low Disease Activity (LDA) according to results from objective activity measurements. To assess the adherence of T2T and to evaluate the application of a tight control T2T-70 and T2T-100 tool, and its association with sustained low disease activity as a measure of outcome. Methods: Sustained LDA (sLDA) was defined when the patient had the Clinical Disease Activity Index (CDAI) lower than 10 during at least 6 months. Measures of adherence to T2T were defined as follows: T2T-70, when therapeutic decisions were accompanied by the measurement of activity by 70% and the interval between visits did not exceed 6 months; And T2T-100, when 100% of the decisions were accompanied with the activity measurement. Results: One hundred and two patients were included. A total of 526 visits were recorded. In 270 visit treatment adjustment was done and 208 (77%) of them were performed according to the CDAI. The frequency of LDAS was 20% (IC95: 12-30). The frequency of T2T-70 and 100 was 62.5% and 42% respectable; that compliance presented a statistically significant association to the achievement of sLDA (p<0.001). Compliance with T2T-70 was also associated with early diagnosis (p:0.009). Conclusion: A global adherence of T2T was 77%. This led to a sustained decrease in disease activity during follow-up. T2T-70 and 100 adherence tool were good, patients who met these criteria reached more sLDA.
Keywords
Rheumatoid arthritis, treatment, managed competition
Introduction
Rheumatoid Arthritis (RA) is a chronic systemic inflammatory disease of unknown etiology characterized by symmetric polyarthritis of small and large joints [1].
Our understanding in terms of prognosis and treatment in RA has changed in the last two decades, due to the development of new therapeutic options and demonstration that tight control of the disease leads to better outcomes [1-3].
The “destructive” effects of RA become evident for the patient after 5 years of disease. However, this process begins at least as early as clinical disease onset and early intervention is associated with a better prognosis [4,5].
Treat to Target (“T2T”) strategy in RA aims to achieve control of the disease, targeting remission or low disease activity; tailoring treatment according to objective disease activity measures, defined by validated scores that enable prediction of joint damage and functional capacity. That strategy is tailored to a patientcentered approach [6,7].
The aim of this study was to perform an integral analysis of T2T strategy implementation in real life practice; to estimate the prevalence of adherence to T2T defined as treatment adjustment according to CDAI (clinical disease activity index); to evaluate the application of a tight control measure to T2T: T2T-70 and T2T-100 and its association with sustained low disease activity (sLDA) as patient outcome.
Methods
Prospective study: Including consecutive patients ≥ 18 years old, evaluated between 2014 and 2016, with a diagnosis of RA and a followup time between 6 and 24 months with at least three visits during that time.
Clinical data were obtained from the electronic clinical records from our center and each visit was constituted as an analysis unit.
Main outcome variable: Adherence to T2T defined as treatment adjustment according to CDAI. To evaluate the application of a tight control measure to T2T: T2T-70 and T2T-100 and its association with sustained low disease activity (sLDA) as patient outcome.
T2T-70, when therapeutic decisions were accompanied by the measurement of activity by 70% and the interval between visits did not exceed 6 months; And T2T-100 when 100% of the decisions were accompanied with the activity measurement. Sustained LDA (sLDA) was defined when the patient had Clinical Disease Activity Index (CDAI) lower than 10 during at least 6 months Study factors T2T-70, when therapeutic decisions were accompanied by the measurement of activity by 70% and the interval between visits did not exceed 6 months; And T2T-100, when 100% of the decisions were accompanied by the activity measurement.
■Other variables
Gender, age, time of evolution of the disease, early arthritis (less than 2 years), seropositivity for RF and ACPA, CDAI at baseline, HAQ at baseline, baseline treatments: methotrexate (dose), leflunomide, hydroxychloroquine, TNF blockers, and other bDMARs.
“T2T characteristics” for this study they were defined as: total follow-up visits, visits with treatment adjustment, CDAI determinations, use of ultrasound (US) to assess disease activity.
■Procedures
Demographics (age, gender), disease characteristics (time of evolution, early diagnosis, seropositivity) and basal treatment were evaluated.
“T2T characteristics” were assessed. For this study they were defined as: total follow-up visits, visits with treatment adjustment, CDAI determinations, use of ultrasound (US) to assess disease activity and achievement of sLDA.
For each visit, the following data was obtained: treatment adjustment, CDAI score, HAQ score and the time lapse between followup visits. In patients fulfilling four visits, median CDAI was compared.
The present study was in accordance with the current Helsinki statement, resolution 1480/11 of our National Health Ministry and local legislation. Patient´s data confidentiality was respected complying with local law and was summited to an institutional board of ethics.
Statistical Analysis
Descriptive statistical analysis was performed. Continuous variables were expressed as a median and Interquartile Range (IQR) or as mean and Standard Deviation (SD) and categorical variables were expressed as percentage and 95% confidence interval (CI 95%). Comparison between categorical data was performed using the chi2 test and Fisher´s exact test and between continuous data using Student´s t-test or Mann Whitney, according to the sample´s distribution.
A multivariate logistic regression analysis was performed, using achievement of LDA as the dependent variable and including as independent variables those with a p<0.1 and those variables considered biologically as poor prognostic factors. A p<0.05 was considered statistically significant.
■ Compliance with ethical standards
The present study was in accordance with the current Helsinki statement, resolution 1480/11 of our National Health Ministry and local legislation. Patient´s data confidentiality was respected complying with local law and was summited and approved to an institutional board of ethics.
Results
A total of 102 patients were included, with a mean follow-up time of 15 months (DS ± 7.8 months), equivalent to 123.6 patients/year. Our patient sample basal characteristics and treatment are shown in TABLE 1.
| Basal Characteristics | N: 102 |
|---|---|
| Female | 80% |
| Age (years) | 53.7 (SD±13) |
| Evolution (months) | 36 (IQR 12-52) |
| Early RA (<2 years) | 64% |
| RF (+) | 85% |
| ACPA (+) | 75% |
| CDAI | 19 (SD±10) |
| HAQ | 1.06 (SD±0.6) |
| Basal Treatment | |
| Methotrexate | 70% |
| MTX dose | 20 mg (IQR 15-20) |
| Corticosteroids | 44% |
| Leflunomide | 9% |
| Hydroxychloroquine | 16% |
| TNF inhibitors | 19% |
| Other b-DMARS | 7% |
TABLE 1. Integral analysis of T2T characteristics in our patient sample.
Median CDAI and HAQ determinations for each patient during follow-up was 2 (IQR 1-3) and 1 (IQR 0-2), respectively, and the median time interval between follow-up visits was 3 months (IQR 2-5). In 32.3% of follow-up visits the US was used to determine an adjustment of treatment and in 14.6% visits treatment adjustment was due to adverse events.
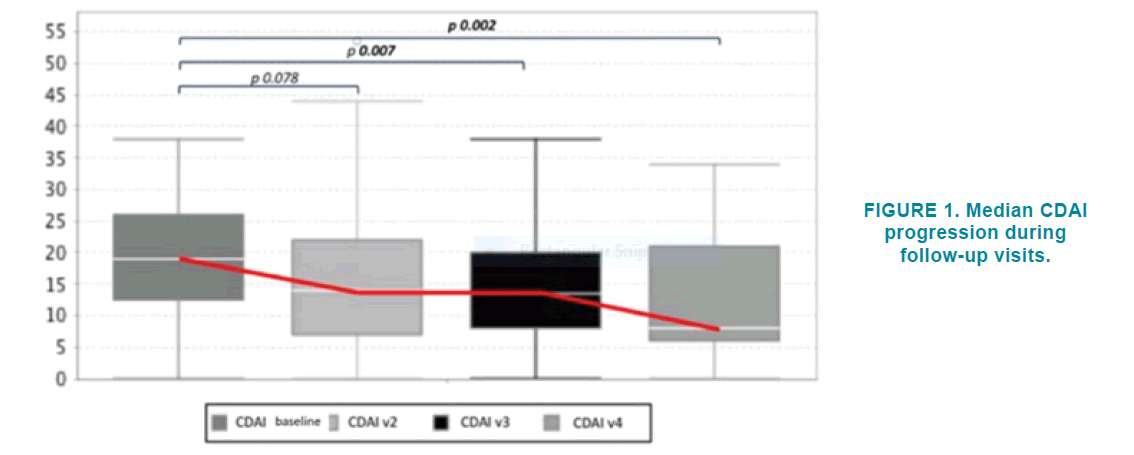
Forty-seven percent of included patients achieved low disease activity as determined by CDAI (CDAI<10) in some point during followup. FIGURE 1 show median CDAI progression in patients fulfilling at least 4 follow-up visits.
The most frequent treatment adjustment in each follow-up visit was the modification of corticosteroid dose (increase or decrease).
When treatment adjustment according to disease activity was analyzed, it was observed that treating physicians tended to be conservative in 60% of patients in LDA and did not change current treatment; however, in 26% patients, a bDMARD was initiated if the target had not been met (TABLE 2).
| Therapeutic Action | Global | LDA | Non LDA |
|---|---|---|---|
| No change | 0.3 | 0.6 | 0.25 |
| Corticosteroid modification | 32.20% | 21% | 20% |
| DMARI) modification | 0.181 | 0.117 | 0.18 |
| bDMARD initiation | 19% | 1.30% | 26% |
Table 2. Frequency of therapeutic adjustments.
Achievement of LDA at any point during follow-up was associated in univariate analysis with: longer time of disease duration (p=0.006), higher number of follow-up visits (p=0.003), higher number of disease activity determinations (p<0.001), longer time interval between followup visits (median months LDA 4.2 vs Non LDA 2.2, p<0.001) and double seropositivity (p=0.04). In the multivariate analysis, an independent association was found between LDA and with a higher number of disease activity determinations and the longer time interval between follow-up visits (TABLE 3).
| Variable | OR | CI (95,0 %) | p value | |
|---|---|---|---|---|
| Time of evolution | 1005 | 0,992 | 1019 | 0,438 |
| Number of Follow-up visits | 0,978 | 0,859 | 1113 | 0,731 |
| Number of disease activity determinations | 2116 | 1330 | 3365 | 0,002 |
| Time interval between visits (months) | 1373 | 1027 | 1837 | 0,033 |
| Female gender | 0,695 | 0,185 | 2615 | 0,591 |
| Double ,S, Q, Q,kivy | 1374 | 0,434 | 4344 | 0,589 |
| Smoking (ever) | 0,620 | 0,197 | 1956 | 0,415 |
Table 3. Logistic regression multivariate analysis. Dependent variable: LDA.
■Adherence to T2T strategy in total follow-up visits analysis
A total of 526 follow-up visits were registered, 270 of which were for treatment adjustment. Of those, 208 (77%) were performed using CDAI determination for that adjustment. We considered this value the absolute adherence to T2T strategy.
We observed a median CDAI 16 (SD ± 10) and 37% (CI 95%: 30-44%) were in LDA.
■ Evaluation of a tool to assess adherence to T2T strategy
During follow-up, the frequency of sLDA was 20% (CI 95%, 12-30%). The frequency of T2T-70 compliance was 62.5% (IC95: 52-72) and T2T-100 was 42% (IC95: 32-52).
Achievement of T2T-70 and T2T-100 were associated with sLDA in univariate analysis (p=0.001, RR 15 CI95% 1.9-118 and p=0.008, RR 4 CI 95% 1.3-11, respectively). T2T-70 was also associated with early diagnosis of RA (<2 years) and fewer follow-up visits than those not meeting this definition.
Both T2T-70 and T2T-100 were independently associated with sLDA in logistic regression analysis. Both models are shown in TABLE 4.
| Variable | Coeficient | EE | Wald | P value | OR | CI (95,0 %) | |
|---|---|---|---|---|---|---|---|
| Number of follow-up visits | -0,149 | 0,063 | -2,386 | 0,017 | 0,861 | 0,762 | 0,974 |
| Number of disease activity determinations | -0,044 | 0,16 | -0,275 | 0,784 | 0,957 | 0,699 | 1,31 |
| Female sex | -0,754 | 0,724 | -1,04 | 0,298 | 0,471 | 0,114 | 1,947 |
| Early RA | 1,455 | 0,553 | 2,631 | 0,009 | 4,286 | 1,45 | 12,673 |
| LDA | 3,136 | 1,154 | 2,717 | 0,007 | 23,013 | 2,397 | 2,20,981 |
| Double seropositivity | 0,437 | 0,595 | 0,734 | 0,463 | 1,548 | 0,482 | 4,97 |
| Logistic regression : dependent variable T2T100 | |||||||
| Age | -0,015 | 0,018 | -0,875 | 0,382 | 0,985 | 0,951 | 1,019 |
| Early RA | 0,708 | 0,482 | 1,47 | 0,141 | 2,031 | 0,79 | 5,221 |
| LDA | 1,497 | 0,584 | 2,565 | 0,01 | 4,468 | 1,424 | 14,025 |
| Female sex | -0,16 | 0,549 | -0,292 | 0,77 | 0,852 | 0,291 | 2,497 |
| Double seropositivity | 0,511 | 0,49 | 1,044 | 0,296 | 1,668 | 0,638 | 4,356 |
Table 4. Logistic regression models for T2T-70 and 100.
Discussion
The initial step to possible success in the management of RA is to treat the patient during the “window of opportunity”, a short time-lapse near the disease onset in which specific treatment with DMARDs may change the prognosis [6]. The next step, whether the patient was treated during the window of opportunity or it was missed, is to maintain tight control of the disease during follow-up using joint count, validated questionnaires to assess functional status, X-rays to evaluate radiographic progression and biochemical markers of inflammation [7,8]. The benefits of the tight control strategy using objective parameters in terms of clinical evolution, functional status, and radiographic progression was demonstrated in the TICORA and CAMERA trials [9-11].
This “good treatment practices” had been resumed in what is known today as the “Treat to Target” (T2T) strategy and in current times tending of patients with RA should not be done without following these premises. The treatment should aim to remission as a target or at least LDA [12,13].
The basic premises to attain this objective are tight control using objective and validated scores and intensive treatment with DMARDs. In our study, we used CDAI as an objective measure to assess disease activity in spite of DAS-28 (most frequently utilized score) because it is the score recommended by EULAR and ACR to assess patients in daily practice and is a more stringent measure to define remission [14,15].
In the present study, we observed in our practice a median of 2 disease activity measures during follow-up with a 3 months interval between follow-up visits, considering this admissible to a T2T strategy. The adequate control of the disease reflects on the lower CDAI reduction during successive visits.
In terms of treatment, T2T recommendations are included in the RA treatment guidelines of the main scientific societies, including EULAR and ACR, and in our local guidelines of the Sociedad Argentina de Reumatología (SAR) [16- 18]. Therefore, we could say that T2T guides our therapeutic decisions, tailoring treatment according to objective validated measures. In our experience, the most frequent therapeutic action was the modification of the corticosteroid doses; however when the patient was in LDA the most frequent conduct was to maintain the current treatment without changes. In patients with active disease during follow-up (CDAI>10) the most frequent therapeutic change was to initiate a biologic DMARD, probably because most patients were already on treatment with conventional DMARDs.
T2T strategy adherence is always a difficult topic to discuss, as there are different ways to define and measure it. In our country, Waismann et al evaluated T2T adherence in the “Consorcio Argentino de Arthritis Temprana” (Early Arthritis Argentine Consortium), defining strategy adherence as treatment adjustment when the patient was not in remission as defined by DAS-28. In that study, treatment was adjusted in 42% follow-up visits. In our experience, we conducted a retrospective analysis of clinical records where 270 followup visits in which treatment was adjusted were detected and 77% of those adjustments were made based on CDAI. Of these patients, 47% achieved LDA [19,20].
Achievement of LDA was independently associated with the number of follow-up visits and a higher number of disease activity determinations which can be interpreted as tight control of the disease. The association of LDA and the longer time interval between follow-up visits we believe is due to a selection bias, as patients who are doing better with the treatment tend to delay the follow-up visit with the rheumatologist. This we see as a weakness of the present study.
The development of T2T-70 and T2T-100 definitions are a rational approach to assess tight control of the disease, as they include both treatment adjustment based on a composite score and a time interval between follow-up visits, in line with international treatment recommendations. Therefore it does not come as a surprise that patients fulfilling this definition fare better, attaining sLDA more frequently.
In our practice, we found that both the followup and therapeutic decisions are made based on the principles of T2T strategy, with a global adherence of 77%. This led to a sustained decrease in disease activity during follow-up.
T2T-70 and T2T-100 fulfillment was 62% and 42%, respectively. Patients meeting any of these definitions were more often in sLDA.
References
- Kelley WN, Harris ED Jr, Ruddy S, et al. Text book of Rheumatology. Philadelphia,WB Saunders (1989).
- Mc Carty DJ. Arthritis and Allied Conditions. A text book of Rheumatology. Philadelphia, Lea & Ferbirger, (1985).
- O'Sullivan JM, Cathcart ES: The prevalence of rheumatoid arthritis:Follow- up evaluation of the efect of criteria on rates in Sudbury, Massachusetts. Ann Intern Med. 76(4), 573-577 (1972).
- Lard LR, Visser H, Speyer I, et al. Early vs delayed treatment in patients with recent onset rheumatoid arthritis. Comparison of two cohorts who receive diferent treatment strategies. Am J Med. 111(6), 446-51 (2001).
- Van AJ, Lard LR, Cessie S,et al. Radiological outcome after four years of early vs delayed treatment strategy in patients with recent onset rheumatoid arthritis. Ann Rheum Dis. 63(3), 274-279 (2004).
- Smolen JS, Aletaha D, Bijlsma JW, et al. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 69(4), 631-637(2010).
- Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 75:3-15 (2016).
- Finch A, Liery H, van Herckenrode CA, et al. Long term impact of early treatment on radiological progression in rheumatoid arthritis. A metaanalysis. Arthritis Rheum. 55(6), 864-72 (2006).
- Mottonen T, Hannonen P, Korpela M, et al. Delay to institution of therapy and induction of remission using single drug or combination diseases modifying antirheumatic drug therapy in early rheumatoid arthritis. Arthritis Rheum. 46(4), 894-898 (2002).
- Grigor C, Capell H, Stirling A, et al. Efect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single blind randomised controlled trial. Lancet. 364(9430), 263-269 (2004).
- Verstappen SM, Jacobs JW, Heurkens J, et al. Intensive treatment with methotrexate in early rheumatoid arthritis: aiming for remission. Computer Assisted Management in Early Rheumatoid Arthritis (CAMERA, an open-label strategy trial). Ann Rheum Dis. 66(11), 1443-1449 (2007).
- Garcia SR. Clinical measurements in rheumatoid arthritis. Rheumatoid Arthritis. 1-6 (2010).
- Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 388(10055), 2023-2038 (2016).
- Felson DT, Smolen JS, Wells G. American College of Rheumatology/European League against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis. 70(3), 404-413 (2011).
- Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 388(10055), 2023-2038 (2016).
- Smolen JS, Landewe´ R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 76(6), 960-977 (2017)
- Singh JA, Saag KG, Bridges SL Jr, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol. 68(1), 1-25 (2016).
- Argentine Society of Rheumatology: Update of clinical practice guidelines in the treatment of rheumatoid arthritis. Argentine Journal of Rheumatology, 2013.
- Marcos J, Waimann CA , Dal PF, et al. General characteristics of an early arthritis cohort in Argentina. Rheumatology. 50(1), 110-16 (2011).
- Waimann CA, Citera G, Dal PF, et al. Adherence to a Treat-to- Target (T2T) strategy in early rheumatoid arthritis. Is it feasible in daily clinical practice? Arthritis Rheum. 66, S1037 (2014).