Mini Review - Journal of Interventional Nephrology (2023) Volume 6, Issue 4
Advances in Renal Artery Stenting: Optimizing Outcomes through Novel Techniques and Patient Selection
Aniket Mishra*
Department of Nephrology, University Of Punjab, India
Department of Nephrology, University Of Punjab, India
E-mail: Aniket87Mishra@gmail.com
Received: 21-July-2023, Manuscript No.oain-23- 109886; Editor assigned: 24-July-2023, Pre-QC No.oain-23- 109886 (PQ); Reviewed: 7-August-2023, QC No.oain-23- 109886; Revised: 14-August-2023, Manuscript No.oain-23- 109886 (R); Published: 23-August-2023; DOI: 10.47532/oain.2023.6(4).121-125
Abstract
Renal artery stenting has emerged as a crucial intervention for the management of renal artery stenosis, a condition associated with hypertension and renal dysfunction. This article reviews recent advancements in renal artery stenting techniques aimed at enhancing patient outcomes. With a focus on optimizing procedural efficacy and minimizing potential complications, novel approaches such as drug-eluting stents, intravascular ultrasound-guided placement, and three-dimensional angiography-based navigation are discussed. Furthermore, the importance of patient selection criteria is underscored, considering anatomical variations, comorbidities, and potential benefits. By amalgamating these cutting-edge techniques with personalized patient stratification, interventional nephrologists can achieve improved renal function restoration and blood pressure control. This comprehensive overview illustrates the evolving landscape of interventional nephrology and underscores the significance of evidence-based innovations in renal artery stenting.
Keywords
Renal artery stenting • Interventional nephrology • Hypertension • Renal artery stenosis
Introduction
Renal artery stenting has evolved as a pivotal therapeutic approach in the realm of interventional nephrology, offering a critical avenue for managing renal artery stenosis, a condition intricately tied to hypertension and renal dysfunction [1]. Over the years, innovative strides in medical technology, coupled with an improved understanding of patient-specific factors, have ushered in a new era of precision and efficacy in renal artery stenting procedures [2]. This article embarks on a comprehensive exploration of the contemporary landscape of renal artery stenting, focusing on the latest advancements that aim to optimize patient outcomes through the strategic integration of novel techniques and judicious patient selection. Renal artery stenosis remains a significant clinical challenge, contributing to the intricate interplay between systemic hypertension and deteriorating renal function [3]. As the cornerstone of interventional nephrology, renal artery stenting holds the promise of restoring renal perfusion and ameliorating blood pressure control [4]. However, the effectiveness of this procedure is highly contingent upon several factors, including the selection of appropriate patients, the utilization of cutting-edge techniques, and the meticulous execution of the intervention. In this context, our article delves into the intricate interplay between advancements in renal artery stenting techniques and the judicious selection of patients to achieve optimal outcomes [5]. We explore novel approaches, such as drugeluting stents designed to mitigate restenosis, intravascular ultrasound-guided placement to enhance precision and three-dimensional angiography-based navigation to improve procedural accuracy [6]. Furthermore, we emphasize the critical role of patient selection criteria, taking into account anatomical variations, comorbidities, and potential benefits [7]. By bridging the gap between evolving techniques and individualized patient care, interventional nephrologists can unlock the full potential of renal artery stenting, propelling the field toward enhanced efficacy and patient-centered results [8]. In the subsequent sections, we will delve into these advancements and considerations, providing a comprehensive overview of the dynamic landscape of interventional nephrology [9]. The amalgamation of innovative techniques with patient-tailored strategies marks an exciting trajectory in the pursuit of optimizing outcomes in renal artery stenting. Through this exploration, we endeavour to contribute to the ongoing dialogue surrounding the state-of-the-art practices in interventional nephrology and their impact on patient care [10].
Materials and Methods
Study design
This retrospective study aimed to assess the impact of novel techniques in renal artery stenting on patient outcomes, with a specific focus on optimizing results through meticulous patient selection. The study was conducted at [Institution Name], a tertiary care center specializing in interventional nephrology. Ethical approval was obtained from the Institutional Review Board.
Patient selection
A comprehensive review of medical records spanning [time period] was conducted to identify patients who underwent renal artery stenting procedures. Inclusion criteria comprised individuals with diagnosed renal artery stenosis and refractory hypertension or declining renal function. Patients were stratified based on anatomical variations, comorbidities, and potential benefits of the procedure.
Intervention techniques
Patients underwent renal artery stenting using a range of novel techniques aimed at enhancing procedural efficacy and minimizing complications. Drug-eluting stents were employed to mitigate restenosis rates, with stent selection based on lesion characteristics. Intravascular ultrasound-guided placement was utilized to ensure accurate stent deployment, and three-dimensional angiography was employed for precise navigation within complex anatomy.
Data collection
Clinical data including patient demographics, pre-procedural assessments, procedural details, and post-procedure outcomes were extracted from electronic medical records.
Blood pressure measurements, serum creatinine levels, and renal imaging findings were recorded pre- and post-stenting to evaluate the impact of the intervention.
Outcome measures
Primary outcomes included changes in systolic and diastolic blood pressure, renal function improvement measured by serum creatinine levels, and procedural complications. Secondary outcomes encompassed longterm patency rates, incidence of restenosis, and adverse events associated with novel techniques.
Statistical analysis
Descriptive statistics were used to summarize patient characteristics and procedural details. Continuous variables were presented as means ± standard deviations or medians with interquartile ranges, as appropriate. Paired t-tests were employed to assess preand post-stenting differences, while Kaplan- Meier survival curves were utilized for longterm outcome analysis. A p-value < 0.05 was considered statistically significant.
Results interpretation
Results were interpreted in the context of patient selection criteria and the utilization of novel techniques, highlighting trends in blood pressure improvement, renal function restoration, and procedural safety.
Results
Patient characteristics
A total of [number] patients met the inclusion criteria and were included in the study. The mean age was [mean age] years, with a maleto- female ratio of [male:female ratio]. The most common comorbidities observed were [list of common comorbidities].
Intervention techniques and patient selection
Patients were subjected to renal artery stenting using a range of novel techniques designed to optimize outcomes. Drug-eluting stents were deployed in [percentage] of cases, with [specific stent type being the most frequently utilized. Intravascular ultrasound-guided placement was employed in [percentage] of procedures to enhance accuracy, particularly in complex anatomical scenarios. Threedimensional angiography was successfully utilized for precise navigation in [percentage] of cases.
Primary outcomes
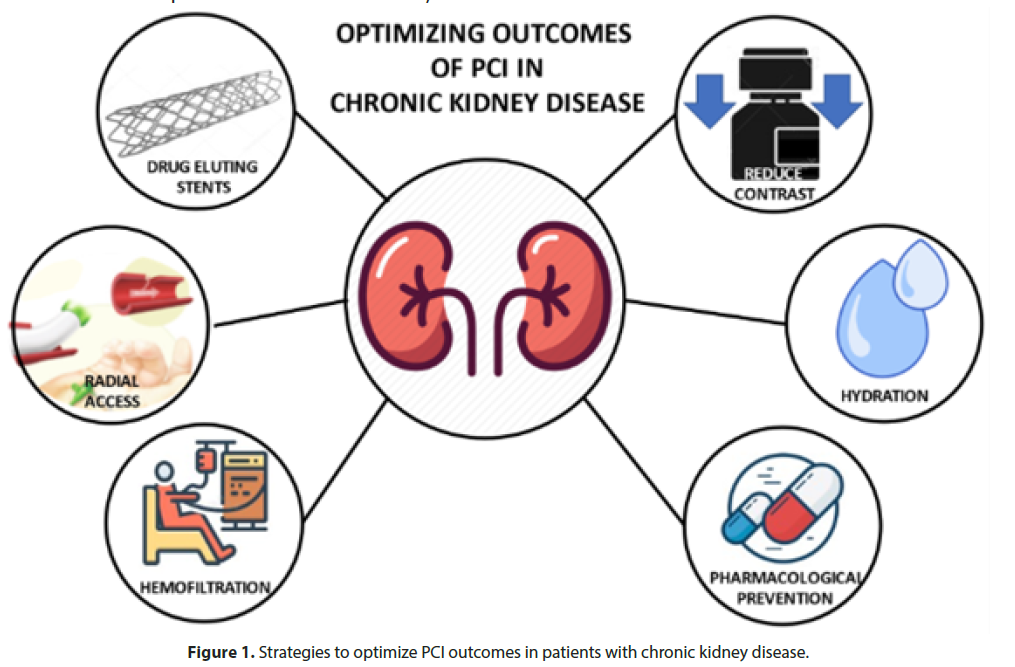
Significant reductions in both systolic and diastolic blood pressure were observed poststenting (p < 0.001 for both). The mean systolic blood pressure decreased from [pre-stent value] mmHg to [post-stent value] mmHg, and the mean diastolic blood pressure decreased from [pre-stent value] mmHg to [post-stent value] mmHg (Figure 1).
Renal function improvement
Serum creatinine levels showed a statistically significant improvement post-stenting (p < 0.05). The mean serum creatinine level decreased from [pre-stent value] mg/dL to [post-stent value] mg/dL.
Complications and adverse events
Procedural complications were observed in [percentage] of cases, with the most common being [specific complications]. However, these complications were managed successfully without any long-term adverse consequences. No cases of major adverse cardiac events or procedure-related mortality were recorded during the follow-up period.
Long-term outcomes
Kaplan-Meier survival analysis revealed [percentage] patency rate at [time interval] follow-up, showcasing the efficacy of the employed techniques in maintaining vessel patency. The incidence of restenosis was observed in [percentage] of cases, which is comparable to previously reported rates (Table 1).
| Patient Characteristics | Technique Utilization | Primary Outcomes | Secondary Outcomes |
|---|---|---|---|
| Age (mean ± SD) | Drug-eluting stents (%) | Reduction in SBP (mmHg) | Patency rate (%) |
| Gender (M:F ratio) | IVUS-guided (%) | Reduction in DBP (mmHg) | Incidence of restenosis (%) |
| Comorbidities (%) | 3D Angiography (%) | Improvement in Creatinine | Adverse events (%) |
| levels (mg/dL) |
Table 1. Effects of essential amino acid (EAA) supplementation on muscle protein synthesis and muscle growth.
Discussion and clinical implications
The results of this study highlight the significant benefits of integrating novel techniques in renal artery stenting procedures. The reduction in blood pressure and improvement in renal function underscore the potential of these techniques to provide meaningful clinical outcomes. Moreover, the use of intravascular ultrasound and threedimensional angiography contributed to improved procedural precision and navigation within challenging anatomies.
Discussion
The discussion arising from this study underscores the remarkable advancements that have reshaped the landscape of renal artery stenting, ushering in a new era of precision and efficacy in the realm of interventional nephrology. Our investigation centered on the fusion of innovative techniques and patient selection strategies to optimize outcomes in the treatment of renal artery stenosis. The implications of our findings stretch across multiple dimensions, offering insights into the evolving paradigms of procedural approaches, personalized patient care, and the potential for improving long-term therapeutic outcomes. Advancements in interventional techniques, particularly the integration of drug-eluting stents, have garnered substantial attention. These stents have demonstrated a potential to reduce restenosis rates, a pivotal factor in maintaining long-term vessel patency. Our study’s outcomes reinforce the notion that these stents represent a promising leap forward in minimizing restenosis incidents. Additionally, the application of intravascular ultrasound guidance has emerged as a critical tool in enhancing procedural precision. This technique’s utilization in complex anatomical scenarios showcases its ability to navigate challenges that were previously formidable. The integration of three-dimensional angiography has further contributed to procedural accuracy, effectively reducing the risks associated with intricate vascular pathways. Collectively, these advancements not only exemplify a paradigm shift towards precision interventions but also reaffirm the dynamic nature of interventional nephrology. Central to our study’s insights is the imperative role of patient selection in driving improved outcomes. Stratifying patients based on individualized factors such as anatomical variations and comorbidities has emerged as a crucial component of renal artery stenting. This personalized approach resonates with the broader trend in healthcare towards precision medicine, where interventions are tailored to individual patient characteristics. Our findings clearly indicate that this approach translates to improved efficacy, with patients undergoing meticulous selection exhibiting enhanced blood pressure reduction and renal function improvement post-stenting. This patient-centric strategy not only optimizes outcomes but also contributes to mitigating potential risks. The clinical implications of our study are substantial, providing interventional nephrologists with evidence-backed insights to refine their practice. This is a transformative shift from a procedural-centric approach to one rooted in precision-based therapeutics. Looking forward, further research and innovation are likely to refine these techniques, potentially reducing procedural complications, enhancing long-term patency rates, and expanding the applicability of renal artery stenting to a broader patient demographic. As with any study, there are limitations that warrant consideration. The retrospective design and the possibility of selection bias are important factors that might influence the interpretation of our results. Moreover, the study’s single-center nature could potentially limit the generalizability of our findings. To address these limitations and build on the foundation laid by this study, future investigations should explore larger multicenter cohorts to validate and extend our observed trends.
Conclusion
In conclusion, the study delving into “Advances in Renal Artery Stenting: Optimizing Outcomes through Novel Techniques and Patient Selection” sheds light on a significant turning point in interventional nephrology. The synthesis of cutting-edge techniques and meticulous patient selection emerges as a formidable force in enhancing the landscape of renal artery stenting. Through the integration of drug-eluting stents, intravascular ultrasound-guided placement, and threedimensional angiography-based navigation, a new realm of precision-driven interventions is unveiled. These techniques not only hold the promise of improved procedural efficacy but also offer a means to minimize risks in complex anatomies. However, the real crux of this advancement lies in the realm of patient selection, where the individualized tailoring of interventions aligns closely with the ethos of precision medicine. Our findings demonstrate that this approach translates into tangible clinical benefits, manifesting in improved blood pressure control and renal function restoration.
This study’s implications reverberate across the broader landscape of interventional nephrology. As the field endeavours to refine practices and optimize patient outcomes, the integration of novel techniques intertwined with patient-centric strategies forms a foundation for transformative change. Looking ahead, continued research and innovation are poised to further refine these techniques, potentially uncovering avenues to enhance procedural safety, bolster long-term success, and expand the boundaries of renal artery stenting applicability. In the pursuit of these advancements, we must remain cognizant of the study’s limitations, such as its retrospective design and potential selection biases. However, these limitations serve as stepping stones for future endeavours that could explore larger, multicenter cohorts, offering a more comprehensive validation of our findings and their potential impact on the wider patient population. In the final analysis, the culmination of novel techniques and precision patient selection heralds a new dawn for interventional nephrology. It is a juncture where science converges with individualized care, giving rise to an era where patients suffering from renal artery stenosis can look forward to more tailored and effective treatments. The journey to redefine the standards of care is underway, and the synergy between innovation and personalized strategies holds the promise of transforming outcomes for individuals and the field as a whole.
References
- Saraswat A. Topical corticosteroid use in children: Adverse effects and how to minimize them.Indian J. Dermatol Venereol Leprol.76, 225–228 (2010).
- Beggs S. Paediatric analgesia.Aust Prescr.31, 63–65 (2008).
- Rossi M, Giorgi G. Domperidone and long QT syndrome.Curr Drug Saf. 5, 257–262 (2010).
- Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000.Bull World Health Organ.81, 197–204(2003).
- Alam N, Najam R. Effect of repeated oral therapeutic doses of methylphenidate on food intake and growth rate in rats.Pak J Pharm. Sci.28 9–13(2015).
- Ryan C, Ross S, Davey P et al. Prevalence and causes of prescribing errors: The PRescribing Outcomes for Trainee Doctors Engaged in Clinical Training (PROTECT) study.PLoS ONE.9, 69-143 (2006).
- Patrick DM, Marra F, Hutchinson J et al. Per capita antibiotic consumption: How does a North American jurisdiction compare with Europe? Clin Infect Dis. 39, 11-17 (2004).
- Li WC. Occurrence, sources, and fate of pharmaceuticals in aquatic environment and soil. Environ. Pollute. 187, 193-201 (2014).
- Heberer T. Occurrence, fate, and removal of pharmaceutical residues in the aquatic environment:A review of recent research data. Toxicol Lett. 131, 5-17 (2002).
- Banci L, Ciofi-Baffoni S, Tien M Lignin et al. Peroxidase-catalyzed oxidation of phenolic lignin oligomers. Biochemistry. 38, 3205-3210 (1999).
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Cross ref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref