Mini Review - Interventional Cardiology (2024) Volume 16, Issue 2
Alternative surgical techniques in the treatment of hydrocephalus
- Corresponding Author:
- Mircea Liţescu
Department of General Surgery, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania,
E-mail: mircea.litescu@umfcd.ro
Received date: 15-Apr-2024, Manuscript No. FMIC-24-132259; Editor assigned: 18-Apr-2024, PreQC No. FMIC-24-132259 (PQ); Reviewed date: 02-May-2024, QC No. FMIC-24-132259; Revised date: 09-May-2024, Manuscript No. FMIC-24-132259 (R); Published date: 17-May-2024, DOI: 10.37532/1755- 5310.2024.16(2).828
Abstract
Hydrocephaly, or hydrocephalus, is a pathological condition characterized by an excessive Cerebrospinal Fluid (CSF) accumulation within the cerebral ventricular system that leads to intracranial hypertension. This elevated pressure, known as intracranial hypertension, has a detrimental effect on the brain’s structure and function. As a result, the “noble substance” of the brain will suffer due to the pressure exerted by the accumulated CSF.
The severity of symptoms and the long-term damage depend on the levels of intracranial pressure and the duration before treatment. Critical levels of intracranial pressure and delayed therapeutic measures will lead to irreversible neurological changes and, finally, to death if left untreated.
While surgical interventions are often necessary for moderate to severe cases, drug treatments may offer a viable alternative for managing milder forms of hydrocephalus or as an adjunct therapy.
The long-term experience with the various procedures discussed below led to the conclusion that the most effective and durable method is the Ventriculoperitoneal (VP) shunt, followed by the transjugular ventricular or Ventriculoatrial (VA) shunt.
Sometimes, drainage system dysfunctions and complications require iterative re- interventions and alternate solutions for the patient’s well-being become mandatory.
In conclusion, effective management of hydrocephalus requires a personalized approach, considering the patient’s condition and response to previous treatments. As the field continues to evolve, ongoing research aims to improve surgical techniques, reduce the risk of complications, and explore new treatment modalities. Close postoperative monitoring is significant to identify and address any complications, ensuring the best possible outcomes for patients with hydrocephalus.
Keywords
Hydrocephalus • Ventriculoperitoneal shunt • Ventriculoatrial shunt
Introduction
Hydrocephalus is a condition marked by an abnormal accumulation of CSF in the brain’s ventricles, leading to increased intracranial pressure due to the disrupted balance between production and absorption. The increase in volume of CSF can expand the ventricles and press against the brain tissue [1]. The average pressure within the ventricular system is between 10 mmHg and 15 mmHg. Moderate and transient exceedances of these values typically have no pathological significance and can spontaneously correct. However, a consistent and significant increase in Cerebrospinal Fluid (CSF) pressure can lead to intracranial hypertension syndrome, affecting brain tissue and serving as a defining feature of hydrocephalus.
The severity of symptoms and the risk of long-term damage depend on the levels of intracranial pressure and the duration before medical intervention. If the intracranial pressure reaches critical levels and therapeutic measures are delayed, this will lead to irreversible neurological changes [2]. These changes may include motor and cognitive impairments, visual disturbances, or other serious complications, and in extreme situations, can lead to death if left untreated.
Literature Review
Hydrocephaly can manifest at any age, with causes and consequences varying significantly from one age group to another.
In newborns, the etiology of hydrocephalus often includes:
• Central nervous system malformations (e.g., malformities stenosis of the Sylvius aqueduct, neural tube defects like myelomeningocele, Dandy-Walker, and Arnold Chiari malformations).
• Infections (e.g., congenital toxoplasmosis, cytomegalovirus).
• Genetic causes (e.g., Bickers-Adams syndrome).
• Meningeal hemorrhages.
• Vascular malformations (e.g., vein of Galen malformations).
In children, causes can range from tumors (medulloblastoma, astrocytoma, ependymoma, choroid plexus tumors) to posttraumatic intraventricular bleeding, CNS infections (bacterial meningitis, tuberculous meningitis, cysticercosis), venous hyperpressure, iatrogenic hydrocephalus, and idiopathic hydrocephalus [3].
In adult and elderly groups, common causes include subarachnoid hemorrhage, brain trauma, various brain tumors, surgery in the posterior cranial fossa, spinal cord tumors, congenital vascular malformations or complicated brain aneurysms, and idiopathic hydrocephalus [4].
The clinical manifestations and consequences of hydrocephalus vary significantly based on the patient’s age and the severity of the condition, highlighting the importance of age-specific approaches to diagnosis and treatment. Here is an overview emphasizing these differences.
In younger patients, the flexibility and growth potential of the skull determines the physical manifestations of hydrocephalus, including increasing the cranial perimeter, suture dehiscence, broad anterior fontanelle as the skull expands to accommodate the excess Cerebrospinal Fluid (CSF), and mental retardation, “sunsetting” gaze, diminished visual acuity or growth retardation.
In older patients, the symptoms often reflect the damage to brain tissue and the loss of brain function, such as paresis of eyeballs and swelling of the optic disc, walking disorders, dementia, encephalomalacia, epileptic seizures, and extrapyramidal disorders.
Diagnosing hydrocephalus involves recognizing the clinical manifestations and imaging tests (e.g., MRI or CT scans) that reveal the extent of CSF accumulation and any impact on brain structures. Papilledema, or swelling of the optic disc visible during an eye exam, can also indicate increased intracranial pressure.
The therapeutic strategy for hydrocephalus must be rapid and precise. It focuses on relieving pressure before irreversible damage occurs and often involves surgical intervention, such as placing a shunt system to divert CSF or endoscopic third ventriculostomy to create a new pathway for fluid drainage. The patient’s age influences the choice of technique, the cause and severity of hydrocephalus, and the presence of any complications.
Early diagnosis and treatment are critical to preventing the longterm consequences of hydrocephalus. Given the variability in symptoms and outcomes depending on age, a tailored approach to each patient is essential for effective management. In all cases, the goal is to alleviate intracranial pressure and prevent irreversible changes that can significantly impact the patient’s quality of life [5].
Discussion
Cerebrospinal Fluid (CSF) diversion is among the most common neurosurgical procedures worldwide [1]. In the United States, neurosurgeons perform approximately 30,000 ventriculostomies annually [6]. The evolution of surgical interventions for hydrocephalus reflects a continual effort to refine procedures, reduce complications, and improve patient outcomes. Each surgical method has unique advantages, challenges, and suitability for different types of hydrocephalus. Modest efficacy, short median shunt survival time, and high rates of complications are the main reasons for the rare use of some procedures. From this chapter, we may remember some techniques such as ventriculopleural [6], ventriculocholecystic [7], ventriculo-ureteral [8], lumbo-ureteral [9], and ventriculomastoid shunts [10].
Here’s a summarized overview of the primary surgical strategies and considerations about their use:
• Endoscopic drainage is best suited for obstructive hydrocephalus due to issues like CSF circulation disorders, Dandy-Walker malformation, stenosis of the Sylvius aqueduct, skull base malformations, and posterior cerebral fossa tumors. This minimally invasive approach has fewer complications and directly addresses the obstruction in CSF flow.
• External drainage is typically used temporarily for emergencies or when the CSF is infected. Surgeons should avoid its longterm use because of the patient’s discomfort and the high risk of meningitis due to the possibility of infections entering along the drainage path.
• Internal drainage primary methods (VP and VA shunts) remain the primary surgical interventions for hydrocephalus. Despite their efficacy, they are prone to complications, sometimes repetitive, leading to therapeutic challenges.
• Ventriculoperitoneal (VP) shunt: Due to its good durability, tolerability, and low complication rate, this procedure became the gold standard for treating all types of hydrocephalus. Today, it is well standardized, but complications related to intraperitoneal organ involvement or shunt malfunction can occur, potentially necessitating multiple revisional surgeries [11].
• The ventriculoatrial shunt is an option when a VP shunt is not feasible due to peritoneal absorption issues or other complications. While the technique is generally effective, complications can also arise, potentially leading to alternative strategies being needed [12].
Surgical technique selection
The surgical team should customize a personalized technique to the type and severity of hydrocephalus, patient-specific factors, and the neurosurgeon’s experience and preference. When primary methods like VP or VA shunts fail or are unsuitable, one may consider alternative techniques based on the unique challenges presented by each case. The journey to optimize hydrocephalus treatment underscores the complexity of this condition and the necessity for continued innovation and adaptability in neurosurgical science.
Neurosurgery continues to evolve, exploring innovative surgical techniques to find effective treatments for hydrocephalus that minimize complications. These techniques provide alternatives when standard methods, such as Ventriculoperitoneal (VP) and Ventriculoatrial (VA) shunt, encounter complications or fail due to patient-specific issues.
Here’s a brief overview of these innovative approaches:
The ventriculoepiploic shunt: Technique modifies the VP shunt approach by directing the CSF into the greater omentum, which has a significant resorptive capacity. The aim is to limit the CSF’s contact with the peritoneal serosa, potentially reducing the risk of complications related to peritoneal absorption issues [13].
Transomphalic extraperitoneal ventricular shunt: This approach attempts to reroute excess CSF into the portal vein, thereby avoiding contact with the peritoneum. The pressure gradient between the ventricular and portal systems might benefit this method, facilitating adequate CSF drainage without engaging the peritoneal cavity [14].
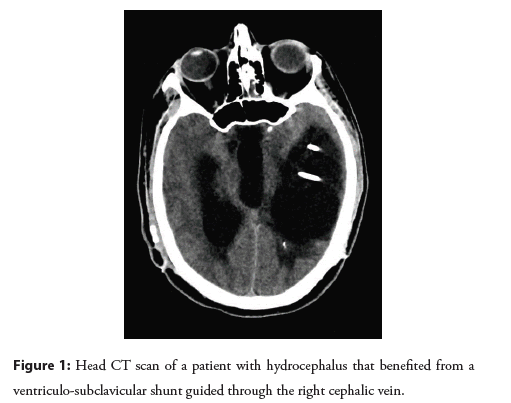
The right ventricular transcephalic shunt: The Figure 1, is designed as an alternative to the VA shunt, especially when the jugular vein is not viable due to conditions like thrombosis. This technique involves routing the drainage catheter to the subclavian vein, superior vena cava, or right atrium through a different vascular approach than the traditional transjugular route [15].
Figure 1: Head CT scan of a patient with hydrocephalus that benefited from a ventriculo-subclavicular shunt guided through the right cephalic vein.
The evolution of surgical techniques for hydrocephalus treatment underscores the importance of continual innovation and customization of treatment plans to individual patient needs and circumstances. As experience with these new methods grows, they may offer valuable alternatives for patients for whom traditional treatments are not viable or have failed.
As a key takeaway message, one should remember that effective management of hydrocephalus requires a personalized approach, considering the patient’s specific condition and response to previous treatments. On the other hand, the field continues to evolve, with ongoing research aimed at improving surgical techniques, reducing the risk of complications, and exploring new treatment modalities. Close postoperative monitoring is crucial to identify and address any complications early, ensuring the best possible outcomes for patients with hydrocephalus.
Conclusion
Introducing these innovative techniques signifies an adaptive and creative approach to managing hydrocephalus, especially in complex cases when standard interventions face limitations. While these techniques aim to bypass common complications associated with traditional shunting methods, the long-term effectiveness and potential unique complications of these new approaches remain under evaluation. Given the early implementation stage and the limited number of cases, the full spectrum of possible complications and efficacy of these innovative procedures is yet to be fully understood. However, they represent potential alternatives for overcoming therapeutic impasses in hydrocephalus treatment.
References
- Rekate HL. A contemporary definition and classification of hydrocephalus. Semin Pediatr Neurol. 16:9-15 (2009).
- Ahmad SR, Moss HE. Update on the diagnosis and treatment of idiopathic intracranial hypertension. Semin Neurol. 39(6):682-691 (2009).
- Thomale UW. Integrated understanding of hydrocephalus a practical approach for a complex disease. Childs Nerv Syst. 37(11):3313-3324 (2021).
- Del Bigio MR, Di Curzio DL. Nonsurgical therapy for hydrocephalus: A comprehensive and critical review. Fluids Barriers CNS. 13:3 (2016).
- Craven C, Asif H, Farrukh A, et al. Case series of ventriculopleural shunts in adults: A single-center experience. J Neurosurg. 126(6):2010-2016 (2016).
- Wong T, Gold J, Houser R, et al. Ventriculopleural shunt: Review of literature and novel ways to improve ventriculopleural shunt tolerance. J Neurol Sci. 428:117564 (2021).
- Smith GW, Moretz WH, Pritchard WL, et al. Ventriculo-biliary shunt: A new treatment for hydrocephalus. Surg Forum. 9:701-705 (1958).
- Waack AL, Hoyt AT, Schroeder JL, et al. Ventriculo-ureteral shunt: Narrative review of contemporary cases and its historical role in the development of renal transplantation. J Neurosci Rural Pract. 14:210-213 (2023).
- Smith JA, Lee RE, Middleton RG, et al. Ventriculoureteral shunt for hydrocephalus without nephrectomy. J Urol. 123(2):224-226 (1980).
- Lake CF. The ventriculomastoid shunt. Laryngoscope. 69(12):1469-1477 (1959).
- Paff M, Alexandru-Abrams D, Muhonen M, et al. Ventriculoperitoneal shunt complications: A review. Interdiscip Neurosurg. 13:66-70 (2018).
- Alnamlah MS, Umerani MS, Darwish AA, et al. Experience with ventriculoatrial shunt: A valid option. Pak j neurol surg. 24(4):376-380 (2020).
- Grigorean VT, Sandu AM, Popescu M, et al. Our initial experience with ventriculo-epiplooic shunt in treatment of hydrocephalus in two centers. Neurol Neurochir Pol. 51(4):290-298 (2017).
- Grigorean VT, Sandu AM, Popescu M, et al. Ventriculoportal shunt, a new transomphalic extraperitoneal surgical technique in treatment of hydrocephalus. Surg Innov. 24(3):223-232 (2017).
- Liţescu M, Cristian DA, Coman VE, et al. Right transcephalic ventriculo-subclavian shunt in the surgical treatment of hydrocephalus-an original procedure for drainage of cerebrospinal fluid into the venous system. J Clin Med. 12(15):4919 (2023).