Case Report - Interventional Cardiology (2021) Volume 13, Issue 3
An atypical presentation of pulmonary thromboembolism
- Corresponding Author:
- Lisa Ferraz
Department of Cardiology,
Centro Hospitalar do Baixo Vouga,
Aveiro,
Portugal,
E-mail: lisacostaf@gmail.com
Received date: April 19, 2021 Accepted date: May 03, 2021 Published date: May 10, 2021
Abstract
The pulmonary thromboembolism with free-floating right heart thrombus is associated with significant mortality. Echocardiography is essential for rapid diagnosis, helping in treatment decisions. A 79-year-old woman, with history of hypertension and hypercholesterolaemia. Medicated with atorvastatin and lercanidipine. She was admitted to hospital with progressive dyspnea for one week, with worsening in the last days. She was tachycardic, hypotensive and polyneic with oxygen desaturation. Arterial blood gas analysis revealed hypoxemia, hypocapnia and elevated lactates. The electrocardiogram showed sinus rhythm, 95/min. Transthoracic echocardiography revealed severe dilation of the right cavities, with severe dysfunction of the right ventricle and presence of multiple mobile echogenic, spindle-shaped, elongated masses swirling around in the right atria, consistent with multiple thrombus in transit (Video 1). A probable diagnosis of pulmonary thromboembolism was considered, however prior to the initiation of fibrinolytic therapy, the patient had cardiorespiratory arrest in pulseless electrical activity and the advanced life support maneuvers weren’t successful.
Keywords
Pulmonary thromboembolism • Intracardiac thrombus • Hemodynamic instability
Introduction
The pulmonary thromboembolism is associated with significant mortality, especially if free-floating right heart thrombus are present [1]. These thrombus are rare and usually represent travelling clots from the legs to the lungs. Echocardiography is essential for rapid diagnosis of acute massive pulmonary embolism associated with right atrial thrombus and cardiovascular collapse, helping in treatment decisions [2].
Case Presentation
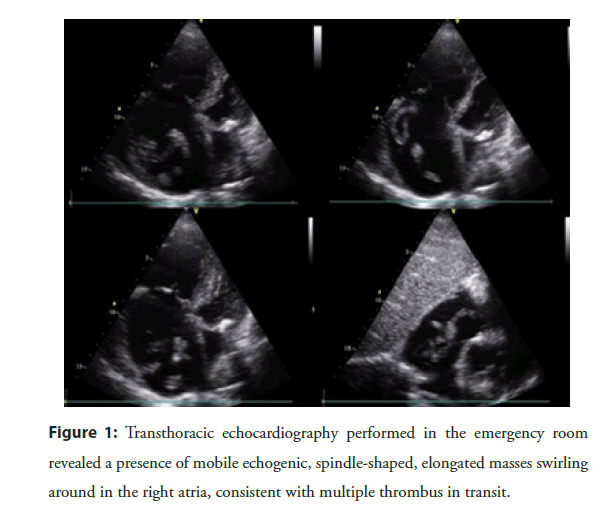
A 79-year-old woman, dependent for daily life activities, with a known history of multiple sclerosis, hypertension, hypercholesterolaemia, interauricular septum aneurysm and deep vein thrombosis of the left lower limb three years ago. Medicated with atorvastatin, pregabalin and lercanidipine. She was admitted to our emergency ward with progressive dyspnea for one week, with worsening in the last days. At physical examination she presented tachycardia, hypotension (blood pressure 80/50 mmHg), polypnea with oxygen desaturation and need for oxygen therapy with 5 L/min. Arterial blood gas analysis revealed hypoxemia (arterial oxygen pressure 76 mmHg, normal 80.0-100.0 mmHg), hypocapnia (arterial pressure of carbon dioxide 19.4 mmHg, normal 35.0-45.0 mmHg) and elevated lactates (9.3 mmol/L, normal <1.8 mmol/L). Her blood sample analysis revealed elevated d-dimers (4134 ng/mL, normal <500 ng/ mL), without other major changes. The ECG showed sinus rhythm, 95/min, S wave in DI, Q wave and flattened T wave in DIII. A transthoracic echocardiography was performed and revealed severe dilation of the right cavities, with severe dysfunction of the right ventricle and presence of multiple mobile echogenic, spindle-shaped, elongated masses swirling around in the right atria, consistent with multiple thrombus in transit (Figure 1). A probable diagnosis of pulmonary thromboembolism was considered and, due to hemodynamic instability and absence of contraindications for fibrinolysis, fibrinolytic therapy with alteplase was intended. Unfortunately, prior to the initiation of therapy, the patient had cardiorespiratory arrest in pulseless electrical activity, and the advanced life support maneuvers were not successful (Video 1).
.Video 1: Transthoracic echocardiography performed in the emergency room revealed a presence of mobile echogenic, spindle-shaped, elongated masses swirling around in the right atria, consistent with multiple thrombus in transit.
Figure 1: Transthoracic echocardiography performed in the emergency room revealed a presence of mobile echogenic, spindle-shaped, elongated masses swirling around in the right atria, consistent with multiple thrombus in transit.
Results and Discussion
The pulmonary thromboembolism is associated with significant mortality, especially if free-floating right heart thrombus are present [1]. These thrombus are rare and usually represent travelling clots from the legs to the lungs [2]. Echocardiography is essential for rapid diagnosis of acute massive pulmonary embolism associated with right atrial thrombus [3], which is sometimes difficult because of the lack of pathognomonic signs or symptoms [4-6], helping in treatment decisions.
The authors considered several conditions able to explain the occurrence of pulmonary thromboembolism in this patient, namely, baseline status of the patient (little mobility) and the occurrence of probable infection, given a history of fever in the previous days and elevated inflammatory parameters. Although the patient had a rapid COVID test that was negative, we cannot rule out the possibility of COVID infection, given the high occurrence of false negatives in this type of tests, the case has occurred during the COVID pandemic, the patient’s clinic and analytical values.
Pulmonary embolism interferes with circulation and gas exchange and ranking high among the causes of cardiovascular mortality. Right ventricular failure due to acute pressure overload is considered the primary cause of death in severe pulmonary embolism. There is an extensive collection of predisposing environmental and genetic factors to pulmonar embolism, such as major trauma, previous pulmonary embolism, cancer (namely pancreatic cancer, haematological malignancies, lung cancer, gastric cancer, and brain cancer) and infection. The clinical signs and symptoms of acute pulmonary embolism are non-specific. In most cases, pulmonary embolism is suspected in a patient with dyspnoea, chest pain, presyncope or syncope or haemoptysis. Haemodynamic instability is a rare but important form of clinical presentation, as it indicates central or extensive pulmonary embolism with severely reduced haemodynamic reserve. If the condition suddenly worsens and there are signs of overt hemodynamic instability (massive or high-risk pulmonary embolism with hypotension or sudden cardiac arrest), the most useful initial test in this situation is bedside transthoracic ecochardiography, wich will yield evidence of increased right-ventricular load with acute right ventricle dysfunction as the cause of the patient’s haemodynamic decompensation. In a highly unstable patient, echocardiographic evidence of right ventricle dysfunction and right heart thrombi is sufficient to prompt immediate reperfusion without further testing and the thrombolytic therapy should be initiated urgently. In case of refractory shock or cardiac arrest, extra corporeal membrane oxygenator could be an option, in combination with surgical embolectomy or catheter-directed treatment, as rescue initiatives. As soon as the patient is stabilized using supportive treatment, final confirmation of the diagnosis should be sought.
Coronavirus disease is an infectious disease caused by a newly discovered coronavirus. One of its most common manifestations is bilateral pneumonia, which, in its most severe forms, is associated with profound hypoxemia. This presentation is usually treated as a type of acute respiratory distress syndrome. However, since the emergence of coronavirus disease-2019, several reports have described significant procoagulant events, including lifethreatening pulmonary embolism, in patients with infection with Severe Acute Respiratory Syndrome Coronavirus 2. Because of the lack of large prospective studies, little is known about the epidemiology and the pathophysiologic mechanisms underlying coronavirus disease-2019 associated pulmonary embolism. The hypercoagulable state in coronavirus disease-2019 was confirmed with higher levels of D-dimer, fibrinogen, and fibrinogen degradation products, prolonged prothrombin time, international normalized ratio, and thrombin time noted in patients with coronavirus disease-2019, being associated with poor prognosis. Some studies show that cellular activation that is triggered by the vírus provocated a true thrombotic disease and a secondary systemic inflammation with very high D-dimer levels. The information about the most appropriate antithrombotic therapy after the acute infection phase is lacking. SARS-CoV-2 infection predispose patients to thrombotic disease, but it is uncertain how long the proinflammatory and prothrombotic state associated with COVID-19 persists for after apparent resolution of the disease with regard to physical symptoms for example, oxygen requirement, fever. There are few recommendations for extended thromboprophylaxis but the use of a structured approach on a patient-to-patient basis, balancing thrombotic and bleeding risks is necessary.
Conclusion
The case highlights the importance of echocardiography in the diagnosis of acute pulmonary embolism with the free floating right heart thrombi, which although rare, are associated with a high mortality and represent a therapeutic emergency.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Charif F, Mansour MJ, Hamdan R, et al. Free-floating right heart thrombus with acute massive pulmonary embolism: A case report and review of the literature. J Cardiovasc Echogr. 28(2): 146-149 (2018).
- Nkoke C, Faucher O, Camus L, et al. Free floating right heart thrombus associated with acute pulmonary embolism: An unsettled therapeutic difficulty. Case Rep Cardiol. 2015: 364780 (2015).
- Chartier L, Béra J, Delomez M, et al. Free-floating thrombi in the right heart diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 99(21): 2779-2783 (1999).
- Majidi A, Mahmoodi S, Baratloo A, et al. Atypical presentation of massive pulmonary embolism: A case report. Emerg (Tehran). 2(1): 46-47 (2014).
- Fisher WT, Reilly K, Salluzzo RF, et al. Atypical presentation of pulmonary embolism. Ann Emerg Med. 19(12):1429-35 (1990).
- Rehman H, John E, Parikh P. Pulmonary embolism presenting as abdominal pain: An atypical presentation of a common diagnosis. Case Rep Emerg Med. 2016: 7832895 (2016).