Review Article - Clinical Practice (2023) Volume 20, Issue 3
An Evidence-Based Review of Analgesics for Pain Management in Minor Oral Surgical Procedures for Patients Predisposed to Gastritis
- Corresponding Author:
- Keerthana Ponvel
Department of Oral and Maxillofacial Surgery, Meenakshi Ammal Dental College & Hospital, MAHER University, Maduravoyal, Chennai, Tamil Nadu, India
E-mail: drkeerthanaomfs@gmail.com
Abstract
Background: Analgesics are preferred for put-up operative pain control. They're indispensable for the uneventful direction of healing after the affected person undergoes oral surgical procedures. All through this, maximum of the analgesics, especially the ones below NSAIDS and opioids are notorious for inflicting gastric infection and ulcers in addition to addiction and dependence. A majority of sufferers are hence additionally suffering from unwarranted gastric inflammation that decreases the best of existence and their standard well-being and luxury. This literature evaluation is framed to apprehend the impact of analgesics in patients predisposed to gastritis undergoing minor oral surgical approaches.
Aim: To review the effect of post-operative analgesics on the gastric mucosa and long-time period problems of consumption of such drugs.
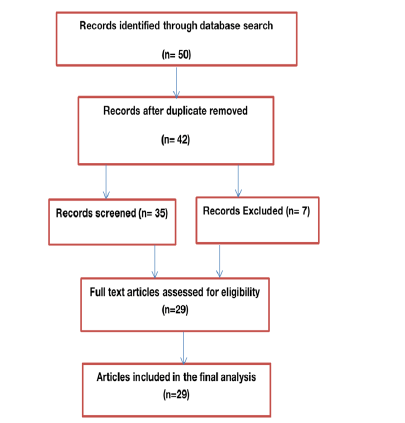
Methodology: PubMed, Cochrane Library, MEDLINE and Science Direct had been looked for the scientific journals by means of using key phrases “gastritis”, “gastric ulcer”, “NSAIDS”, “opioids” “nsaids precipitated ulcer”, “gastric perforations”, “gastric cancer”. Result: 50 articles had been identified through database search, out of 50 after duplicate removal 29 full-text articles were assessed and finalized for eligibility. In this text, we have reviewed the usage of analgesics in patients with gastric disorders primarily based on the available literature and contemporary evidence.
Conclusion: Maximum of the analgesics upon management cause gastro duodenal irritation and opioids have possibilities of dependency. This in turn causes physical and emotional discomfort to the patient. There may be a destiny scope of the advent of an alternative method of analgesia that reduces affected person soreness on taking analgesics which is thought to cause gastric infection, bleeding ulcers and prolonged use also leads to gastric perforation, most cancers and pharmacological dependence caused by opioids.
Keywords
gastritis, gastric ulcer, NSAIDS, opioids, gastric perforations, gastric most cancers
Introduction
Minor oral surgical procedures, such as patients undergoing intra-alveolar extraction, transalveolar extraction, impaction, alveoloplasty, implant placement, cyst enucleation, and TMJ strategies to call a few. These procedures involve the dissection of gingival mucosa and dissection of tender tissues and periosteum, guttering of bone tissues which are enormously invasive with a high incidence of post-operative pain which may be a result of postsurgical irritation/ inflammation secondary to the method, and it markedly affects patients’ restoration and pride, as a consequence warrant adequate intervention to alleviate the pain and consequently offer a discourse of return to everyday lifestyles and activities as early as viable. There had been a varied number of research into the efficacy of the drugs to reduce the ache and swelling [1].
Management of postoperative pain could be very important and drugs used to control pain not only have to be strong analgesics but must have better anti-inflammatory assets also. Analgesics shape a majority of drug treatments prescribed to patients undergoing oral and maxillofacial surgical treatments for the pain control. Most of the analgesics, specifically those beneath NSAIDS and opioids are notorious for causing gastric irritation and ulcers in addition to addiction and dependence. A majority of patients are consequently additionally affected by unwarranted gastric inflammation that decreases their quality of life and their general well-being and comfort. Very few researchers might be thinking about the gastric facet results of these medications and the viable remedies and alternatives [2].
In the area of Oral and Maxillofacial surgical operation, the endorsed capsules prescribed for use in postoperative analgesia consist of opioid analgesics, nonselective Nonsteroidal Anti-Inflammatory pills (NSAIDs), selective Cyclooxygenase (COX)-2 inhibitors, and acetaminophen. There may be tremendous subjects approximately gastrointestinal dysfunction and suppression of platelet features with the administration of nonselective NSAIDs because of the inhibition of prostaglandin and thromboxane synthesis via COX-1. Moreover, the utility of opioids is restrained due to destructive consequences including nausea, vomiting, drowsiness and drug dependence. In some international locations, for example, the United States, there may be top-notch difficulty with opioid misuse. Consequently, effective oral analgesics with a better protection profile are necessary. It's miles of paramount significance to prescribe an analgesic that isn't inflicting any side results and is also able to assuage the pain postoperatively [3, 4].
Methods
Literature became decided on through a search of PubMed, Cochrane Library, MEDLINE and Science Direct for the publications associated with pain and gastritis. The key phrases used for seeking were “NSAIDS”, “gastritis”, “gastro enteropathy, “gastric side consequences”, “opioids”, “gastritis because of opioids, “pain pathway”. Articles posted in the English Language became searched and selected from 12 months 1992-2022. In keeping with the available information, the articles blanketed are Review articles, Experimental articles and Hypothetical articles. Articles have been decided on the idea of evidence-based observation, the strength of analgesics utilized in a study, the type of medication used for examination and 1 year to 2 year follow-up. Articles that used identical analgesics from preceding studies and studies carried out on animal topics have been excluded. Each obtained article changed into reviewed and analyzed by 2 independent readers and if the articles have been taken into consideration relevant with the aid of both the readers they have been protected. In the event of a confrontation, the articles were re-examined and mentioned most of the authors and a choice changed into made whether or no longer to consist of the thing.
Database search revealed 50 articles associated with analgesia and gastritis, out of which 42 were recorded after reproduction was eliminated. Following the screening of the entire-text articles, 35 doubtlessly relevant full-textual content articles have been decided on and reviewed, and 7 articles were excluded. Full-length articles were obtained and their references were looked for additional articles (FIGURE 1).
Review of Literature
Pain is defined by the International Association for the Study of Pain (IASP) as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage”. Nociception, a complex set of electrochemical events that take place among the website online of tissue harm and the feel of pain, is one element of pain. Fundamental knowledge is key to treating pain efficiently. To successfully deal with pain, it's far vital to understand nociception. Four processes make up nociception: Modulation, transduction, transmission, and perception [5].
There are two substantial pain reflex pathways. The sympathetic aspect is proven by way of the top loop. Sympathetic reflexes are activated by the nociceptor input, and they then sensitize or activate the nociceptor terminals. The muscular contraction loop is depicted in the bottom loop. In some patients, nociceptors cause muscular nociceptors, which then feed returned into the same reflex to keep muscle contraction and discomfort [5, 6].
Gastritis is a set of conditions that inflame the stomach lining. Gastritis can be caused by drinking too much alcohol, prolonged use of Non-steroid Anti-Inflammatory Drugs (NSAID) such as aspirin or ibuprofen, or bacterial infection, such as Helicobacter pylori (H. pylori) considered the most typical cause of gastritis in the globe. However, gastritis was also discovered in 60%–70% of H. pylori-negative patients with functional dyspepsia or non-erosive gastroesophageal reflux. The distinction between acute and chronic gastritis is based on its time course, histological characteristics, anatomical distribution, and underlying pathogenic causes [7]. If acute gastritis is not treated, it will become chronic. Autoimmune gastritis is defined as chronic atrophic gastritis that is restricted to the corpus and fundus of the stomach and that is producing substantial diffuse atrophy of parietal and chief cells. It is associated with serum antiparietal and anti-intrinsic factor antibodies. Other than H. pylori, additional organisms like Mycobacterium avium intracellular, Herpes simplex, and Cytomegalovirus can also cause gastroenteritis. GERD is brought on by acid reflux. Collagenous gastritis, sarcoidosis, eosinophilic gastritis, and lymphocytic gastritis are all uncommon causes of gastritis [7,8].
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are most commonly used for their therapeutic effects which include inflammation inhibition, analgesia and fever suppression [9]. Although NSAIDs can lead to gastrointestinal complications, they are frequently prescribed worldwide. Their primary mechanism of action consists of Cyclooxygenase (COX) enzyme inhibition, thus reducing the synthesis of prostaglandins, which play a crucial role in gastro-protective mucus secretion. Therefore, NSAID use can lead to several adverse gastrointestinal effects, such as gastric or duodenal ulcers, hemorrhage or perforation [9, 10]. These complications are more common in non-selective NSAIDs, which act both on COX1 and COX2, whereas COX2-selective inhibitors tend to lower the risk of gastrointestinal complications [8]. Although NSAIDs represent the most common class of drugs which can cause gastrointestinal tract complications, other substances can also damage the gastric mucosa in children, such as corticosteroids, valproic acid or chemotherapeutic drugs. A rare case of hemorrhagic gastritis induced by oral iron supplements in a teenage female has also been described in the literature [11].
NSAIDs injure the gut by causing topical injury to the mucosa and systemic effects associated with mucosal prostaglandin depletion derived from COX-1. The systemic effects of NSAIDs appear to have a predominant role. Because of that, the use of enteric-coated aspirin preparations and parenteral or rectal administration of NSAIDs to prevent topical mucosal injury has failed to prevent the development of ulcers [12]. The acidic properties of most NSAIDs (including ASA) initiate mucosal damage. These weak acids remain in their non-ionized lipophilic form in the highly acidic gastric environment. These conditions favour migration into surface epithelial cells, where NSAIDs are dissociated into the ionized form that traps hydrogen ions, inducing mucosal injury [13].
COX 2 isoform is prompted in most tissues in response to inflammatory stimuli. Prostaglandins derived from COX-2 may be generated on the ulcer margin and seem to play a crucial role in ulcer recuperation by triggering cell proliferation, angiogenesis and healing of mucosal integrity. This isoform is the number one goal for antiinflammatory drugs [14]. Therefore selective COX-2 NSAIDs even as having little to no impact on COX-1, ought to bring about powerful ache comfort with decreased damaging GI effects. This 'COX 2 hypothesis' has been challenged with the aid of using records from animal studies. Wallace et al pronounced that inhibition of each COX-1 and COX-2 is needed for NSAID-precipitated gastric harm within side the rat [14, 15].
The upper gastrointestinal results of NSAIDs can adversely affect the upper and lower gastrointestinal tract. The scientific importance and frequency of unfavorable occasions with NSAIDs inside the lower GI tract had been reported time and again, however, it is much less characterized than the ones from the upper GI tract [16]. The latest study from Lanas et al has proven that the frequency of hospitalizations because of upper GI complications lowering for the last 10 years, while the ones from the lower GI tract are increasing. In this article, we can recognize the upper GI occasions. From a scientific point of view, upper GI unfavorable occasions of NSAIDs may be classified into distinctive types [17].
■ Review of each drug with adverse effects
Paracetamol is regarded as an effective and relatively safe drug and has had a long history of causing low gastro-duodenal injury in both human and animal subjects. Paracetamol has a central analgesic effect that is mediated through the activation of descending serotonergic pathways. Debate exists about its primary site of action, which may be the inhibition of Prostaglandin (PG) synthesis or through an active metabolite influencing cannabinoid receptors. Studies on the mechanism of paracetamol action need to be further investigated; they should focus not only on the therapeutic effects of this medication but also on more frequently reported poisonings, particularly severe hepatotoxicity brought on by drug overdoses given the wide availability of paracetamol-containing preparations [18-20].
Ibuprofen is a non-selective COX inhibitor that is commonly used in adult, geriatric and pediatric patients, not only for its analgesic and antipyretic properties but also for safety reasons, in comparison with other drugs from its class. In addition, ibuprofen scavenges HO•, •NO, and ONOO− radicals and can potentiate or inhibit nitric oxide formation through its effects on Nitric Oxide Synthase (NOS) isoforms. Ibuprofen may activate the antinociceptive axis by binding to the cannabinoid receptors and through inhibition of fatty acid amide. One disadvantage of these medications is that they often cause stomach and bowel problems when taken for several weeks or months leading to stomach ulcers (gastric ulcers) or duodenal ulcers [21, 22].
These ulcers are collectively known as peptic ulcers. NSAIDs reduce the production of the hormone prostaglandin. One of the things prostaglandins do increase the production of gastric (stomach) mucus and substances that neutralize stomach acid. If there is too little prostaglandin, the stomach lining becomes more susceptible to damage from stomach acid. It can then become inflamed, and eventually, ulcers may develop. The guidelines concerning its posology and intervals of administration should be strictly respected to avoid adverse gastrointestinal effects [11,21,22].
Ketorolac tromethamine is a nonsteroidal anti-inflammatory drug with potent analgesic properties. Ketorolac is used to manage and treat acute, moderate to severe pain. It acts by inhibiting both COX-1 and COX-2 enzymes which are normally responsible for converting arachidonic acid to prostaglandins [10]. The COX-1 enzyme is constitutively active and can be found in platelets, gastric mucosa, and vascular endothelium. When ketorolac is used in higher doses, for periods longer than five days, or people older than 75, the risk of adverse effects rises noticeably. Ketorolac exhibits connections with severe GI, renal, and cardiovascular hazards, just like other NSAIDs. It may result in stomach or intestinal perforations as well as peptic ulcers in the GI system. All NSAIDs, including COX2 inhibitors, were demonstrated to raise the relative risk for peptic ulcers in a sizable pooled data set, with ketorolac having the highest RR at 11.5%. Ketorolac raises the risk of GI bleeding because of its antiplatelet characteristics. When compared to opioids, it also increases the risk of postoperative hemorrhage [23, 24].
Ketorolac is not recommended for people who react poorly to NSAIDs or who have allergies to them. Given the increased risk of bleeding, it is not advised to be administered either intraoperatively or before surgery. As it impairs fetal circulation and lessens uterine contraction, it is not advised during labor and delivery. Due to its potential to decrease renal function and increase fluid retention in individuals with renal disease or renal failure, ketorolac is contraindicated in these cases. Ketorolac is contraindicated in those with active peptic ulcer disease, recent gastrointestinal bleeding, or GI perforations. Caution should be used when administering this drug and patients should be monitored for adverse effects [23, 24].
Aceclofenac is a phenylacetic acid derivative NSAID with the chemical designation [2-(2,6-chlorophenyl) amino]- phenylacetoxyacetic acid. It is widely used in the management of pain and inflammation. Aceclofenac is also reported to reduce dental pain and inflammation. It is associated with gastrointestinal adverse events, including nausea, diarrhea, flatulence, constipation, vomiting, bleeding, and ulcers, which are the most common tolerability issues with this drug [25- 27].
Naproxen sodium (Anaprox) is an effective analgesic and anti-inflammatory drug, several studies have shown that it effectively manages both chronic and acute pain. It inhibits prostaglandin formation, leading to its therapeutic effectiveness, particularly in alleviating dysmenorrhea. Both naproxen and naproxen sodium have similar biological characteristics when dissolved in biological fluids, but administering naproxen as the sodium form allows for faster absorption from the digestive tract. The drug is almost entirely absorbed and has a typical 13-hour metabolic half-life. Naproxen is metabolized straightforwardly, with the parent molecule and its oxidative 6-desmethyl metabolite and their respective conjugates eliminated mainly in the urine. Its high therapeutic index and shallow dose-response curve make it less likely for other medications to significantly affect its pharmacokinetics [28, 29].
Diclofenac is a potent NSAID with wellresearched analgesic, anti-inflammatory, and antipyretic effects. It is commonly prescribed for treating acute and chronic pain and inflammatory conditions. Like all NSAIDs, diclofenac inhibits the production of prostaglandins by blocking both Cyclooxygenase-1 (COX-1) and Cyclooxygenase-2 (COX-2). The most commonly used form is the enteric-coated tablet containing 50 mg of diclofenac sodium. However, oral diclofenac has been associated with gastrointestinal disturbances, including gastritis, nausea, abdominal pain, constipation, vomiting, and GI ulcers. Sublingual piroxicam in the management of postoperative pain after surgical removal of the impacted mandibular third molar [30, 31].
Piroxicam is a potent, long-acting NSAID from the oxicam family, used for rheumatoid arthritis and osteoarthritis. It has keen antipyreticanalgesic action, inhibiting Cyclo-oxygenase (COX) reversibly. The drug's half-life is 38 hours, and it is primarily eliminated through hepatic metabolism to inactive metabolites, with less than 10% excreted unchanged in urine.
For post-operative pain after impacted teeth removal, piroxicam is available in both oral and sublingual forms. Adverse reactions in about 11% of patients include headache, dizziness, drowsiness, fatigue, and sweating. Peptic ulceration and gastrointestinal bleeding occurred in 1-1.4% of patients taking 20 mg/ day, increasing to 6.9% at 40 mg/day. Piroxicam may reduce renal blood flow, leading to transient and likely insignificant rises in urea or blood urea nitrogen, but serum creatinine concentrations remain unaffected. Reports of renal damage attributed to piroxicam have been documented [32,33].
Opioids have been the primary medication class used in oral and maxillofacial surgery for treating moderate to severe postoperative pain. Opiates have a long history, with references dating back to ancient civilizations. The opium poppy, Papaver somniferum, produces over 20 distinct alkaloids, including codeine and morphine [34].
The body contains opioid receptors that respond to both endogenously produced and exogenously administered opioid compounds, offering effective central analgesia. Opioid receptors are subdivided into delta, kappa, and mu subtypes and are located in various areas, including the spinal cord and brain, contributing to their efficacy in managing acute postsurgical pain [34,35].
However, the use of opioids can lead to various side effects in the gastrointestinal tract, such as dysmotility, gastric emptying delay, opioidinduced ileus, and opioid-induced constipation (OIC). Patients receiving opioids postoperatively should be closely monitored, and signs of respiratory depression or distress should be treated promptly with appropriate interventions, including opioid reduction, respiratory support, and opioid antagonist administration [36].
■ The routes of administration for acute postoperative pain medication
Multimodal analgesia involves the use of various analgesic medications and techniques that target different mechanisms of action in the peripheral or central nervous system. Different routes of administration can be used for dental pain management, each with its advantages and disadvantages. Oral administration of analgesic agents is a simple and non-invasive method that is highly accepted by patients and has demonstrated good efficacy in most cases [37,38].
Oral administration of NSAIDs requires the drugs to pass through the harsh environment of the gastrointestinal tract. Sublingual administration, on the other hand, bypasses the gastrointestinal tract. In inpatient settings, intramuscular (IM) or Intravenous (IV) routes are commonly used. However, for outpatient management, oral administration is the most preferred route [10, 39].
The IV route provides the fastest delivery of analgesics, but it comes with higher costs for intravenous opioids, paracetamol, or NSAIDs, without any additional benefit in terms of pain control. Therefore, the IV route should only be considered when the oral route is not feasible [40].
IM and Subcutaneous (SC) routes are frequently employed for acute pain treatment. However, after surgery, alternative routes of administration are preferred due to potential issues with poor perfusion, such as hypovolemia or hypothermia, which can affect the absorption of analgesics. This can result in inadequate pain relief or delayed side effects due to the redistribution of the medication depot once perfusion improves [10, 40].
Transdermal (TD) route
Transdermal drugs are applied to the skin and are absorbed into the bloodstream, primarily affecting the central nervous system. Fentanyl and buprenorphine are available in Transdermal (TD) preparations due to their ability to penetrate the skin. However, the onset and offset times of TD preparations are slow, making it difficult to titrate the dosage for short-term use. In many countries, TD fentanyl patches are specifically contraindicated for managing acute or postoperative pain. On the other hand, the fentanyl iontophoretic transdermal system is more widely accepted by nurses and patients compared to intravenous patient-controlled analgesia with morphine [41,42].
Transmucosal route
Highly fat-soluble drugs can be given through transmucosal routes, such as sublingual, buccal, intranasal, or rectal administration. These routes bypass first-pass hepatic metabolism and allow the drug to quickly enter the systemic circulation [10,43].
Rectal route
Rectal administration is a secondary option when other routes are unavailable. However, it has limitations related to absorption variability and rectal irritation. Contraindications include immune suppression, pre-existing rectal lesions, and recent colorectal surgery [40].
Both opioids and paracetamol can be effective when given rectally, but the time to peak analgesic effect and bioavailability can vary significantly among patients. Rectal opioids are mainly used for managing cancer pain. Rectal NSAIDs provide effective analgesia in many postoperative scenarios. However, they may cause rectal irritation and diarrhea, with similar incidences of nausea and vomiting compared to other routes. Therefore, using rectal NSAIDs does not offer any advantage over oral administration [44].
Intranasal Route (IN)
Nasal mucosa allows for high drug absorption, influenced by lipid solubility and drug ionization. The clinical impact of human nasal first-pass metabolism is not entirely clear. For intranasal (IN) drugs, it is suggested to limit the volume to 150 μL to prevent run-off into the pharynx [45].
Various opioids can be efficiently administered via the IN route. IN fentanyl is used for breakthrough cancer pain treatment. However, there was no significant difference in postoperative pain relief when comparing IN fentanyl to IV morphine, oral morphine, or IV fentanyl. Additionally, 3.15 g of IN ketorolac has been proven effective with an opioid-sparing effect after major surgery [46].
Sublingual and buccal routes
Sublingual (SL) or buccal mucosae provide a large surface for drug absorption, but swallowing may affect their effectiveness. Various fentanyl preparations, such as buccal tablets and soluble films, are approved for breakthrough cancer pain. However, SL preparations are not recommended for opioid-naïve patients or acute and postoperative pain due to the risk of respiratory depression [10,40].
Epidural route
Epidural analgesia is widely used for acute pain management in surgical settings, especially during childbirth. It is more effective than IV opioid analgesia and is recommended for postoperative pain relief in high-risk patients [10].
Intrathecal (IT)
Intrathecal local anaesthetics provide short-term postoperative analgesia. When combined with IT morphine (50-100 mcg) during orthopedic, urological, and gynecological procedures, it allows for longer-lasting analgesia compared to IT local anaesthetics alone. IT opioids are more effective in controlling pain than IV administration, but they may lead to more frequent side effects such as respiratory depression, urinary retention, nausea, vomiting, and pruritus [47].
■ Peripheral blocks
Regional and local analgesic techniques are now more commonly employed for perioperative pain management and are considered essential components of modern multimodal postoperative analgesia. The use of ultrasoundguided procedures has further enhanced the popularity of these techniques due to their improved success rate, faster performance, and quicker onset of action [10,48].
Sublingual administration of NSAIDs provides faster pain relief compared to oral administration. The drug is absorbed by the veins on the floor of the mouth, leading directly to the superior vena cava, resulting in quicker distribution of the drug [40,48].
Discussion
Despite significant efforts to improve postsurgical outcomes, the severity and burden of postsurgical pain continue to have a negative impact. Gastroenteropathy is frequently treated with acid-lowering medications, but the specific medications used can vary depending on the symptoms' type and intensity [49]. Proton Pump Inhibitors (PPIs) such as omeprazole and pantoprazole are commonly used to reduce stomach acid production. H2 blockers like ranitidine and famotidine also decrease acid formation. Antacids such as magnesium hydroxide or aluminum hydroxide neutralize stomach acid [50].
In cases where Helicobacter infection causes gastritis, PPIs are used in combination with two or three medications. If Nonsteroidal AntiInflammatory Drugs (NSAIDs) need to be taken frequently, they can be administered with an acidreducing drug. Administering local anesthesia to patients with gastritis does not present any contraindications. However, caution must be exercised when handling patients undergoing major surgical procedures due to prolonged immobilization of the gastric mucosa [51].
Detecting ulcerations caused by gastro enteropathy often requires expensive endoscopic examinations that may not always be available or affordable. Prolonged gastritis and breaches in the gastric mucosal lining can lead to more serious conditions. Therefore, it is crucial to address this concern early on and consider alternative medications whenever possible [52].
Therefore, the need for medications that are least gastrotoxic while effectively alleviating pain in postoperative pain management cannot be overstated. There are over 300 analogues of endogenous or exogenous opioid peptides designed to act on opioid receptors [53]. Extensive research has focused on developing new molecules that primarily have peripheral effects and do not pass the blood-brain barrier. Morphine and morphine-like medications predominantly work through the opioid μ receptor, which is responsible for most opioid effects in the brain and periphery. Opioid analogues, however, can have adverse effects on bowel function, including severe constipation, hard stools, incomplete evacuation, straining, bloating, and gastroesophageal reflux [54].
Nevertheless, some of these medications can be used to manage excessive exertion, such as fistula or story output. Loperamide and diphenoxylate are two popular opiates frequently used for this purpose [55].
Tolerance and dependency are common side effects associated with opioid treatment, both primary and acquired. Tolerance and dependency can have a genetic origin and may be present from the first dose. Acquired tolerance and dependency can be categorized as pharmacokinetic, pharmacodynamic, or learned. Repeated administration leads to pharmacokinetic tolerance, while decreased drug effectiveness over time results in pharmacodynamic tolerance [56]. Learned tolerance occurs when the effectiveness of the opioid medication decreases due to its frequent use. Although the mechanisms of tolerance are not fully understood, some studies have suggested increased neuropeptide activity, such as Calcitonin Gene-Related Peptide (CGRP) and substance P [57].
Hawkey et al. in 1991 found that aspirin and other Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) may have both anti-hemostatic and ulcerogenic effects on individuals with hematemesis and melena. To evaluate the erosive and anti-hemostatic effects of aspirin on the human stomach mucosa, they developed techniques for separate assessments. Under blinded randomized conditions, volunteers received either 300 mg of aspirin daily in the morning or 600 mg four times a day for five days. They investigated changes in endoscopic damage symptoms, spontaneous bleeding due to stomach erosion, biopsy-induced bleeding, and eicosanoid levels [58].
Aspirin significantly decreased serum thromboxane levels and greatly inhibited prostaglandin E2 generation in the stomach mucosa. Erosions developed and resolved quickly compared to baseline. Gastric erosions occurred more frequently when taking 300 mg of aspirin daily in the morning but, this was significantly less than when taking 600 mg of aspirin four times a day [58]. The occurrence of erosions was only associated with increased spontaneous bleeding when aspirin was used. Aspirin was associated with a high incidence of bleeding per stomach erosion and significantly increased bleeding caused by mucosal biopsy. The enteric coating did not affect aspirin's poor hemostasis, although it reduced endoscopic damage symptoms [59].
One of the limitations of analgesics is that their administration often causes gastro-duodenal irritation, and opioids can lead to dependency. This, in turn, causes physical and emotional discomfort for the patient, and the economic implications are an additional burden on both the patient and their family. Flupirtine maleate is a unique analgesic that neither belongs to the opioid family nor is classified as a Nonsteroidal Anti-Inflammatory Drug (NSAID). Its analgesic action occurs through the blockade of glutamate N-methyl-D-aspartate receptors. Unlike routinely used analgesic drugs, Flupirtine Maleate is devoid of their adverse effects while being equally effective in reducing pain sensation. Its distinctive mechanism of action provides a dual therapeutic effect with both analgesic and muscle relaxant properties, making it useful in the treatment of pain associated with muscle tension [60].
Conclusion
To conclude in terms of future scope, there is a need to introduce alternative methods of analgesia that reduce patient discomfort associated with analgesics known to cause gastric irritation, bleeding ulcers, and other potential complications such as gastric perforation, cancer, and pharmacological dependence caused by opioids.
Ethical Approval
Not applicable
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgement
Nil
Funding
Nil
References
- Hanzawa A, Handa T, Kohkita Y, Ichinohe T, Fukuda KI, A comparative study of oral analgesics for postoperative pain after minor oral surgery. Anesth. Prog. 65(1), 24-29 (2018). [Google Scholar] [Cross Ref]
- Drini M., Peptic ulcer disease and non-steroidal anti-inflammatory drugs. Aust. Prescr. 40(3), 91 (2017). [Google Scholar] [Cross Ref]
- Poveda RR, Bagan JV, Jimenez S. Y, Gallud RL., Use of nonsteroidal antiinflammatory drugs in dental practice: A review. Medicina Oral, Patología Oral y Cirugía Bucal. 2007 Jan;12(1):10-18. [Google Scholar] [Cross Ref]
- Kim SJ, Seo JT. Selection of analgesics for the management of acute and postoperative dental pain: a mini-review. J. Periodontal & Implant Sci. 50(2), 68 (2020). [Google Scholar] [Cross Ref]
- Manion J, Waller MA, Clark T, Massingham JN, Neely GG. Developing modern pain therapies. Front. Neurosci. 13, 1370 (2019). [Google Scholar] [Cross Ref]
- Steeds CE. The anatomy and physiology of pain. Surgery (Oxford). 27(12), 507-511 (2009). [Google Scholar] [Cross Ref]
- Sipponen P, Maaroos HI. Chronic gastritis., Scand. J. Gastroenterol. 50(6), 657-667 (2015). [Google Scholar] [Cross Ref]
- Varbanova M, Frauenschlager K, Malfertheiner P. Chronic gastritis – an update. Best Pract. Res. Clin. Gastroenterol. 28(6), 1031-1042 (2014). [Google Scholar] [Cross Ref]
- Bindu S, Mazumder S, Bandyopadhyay U., Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective. Biochem. Pharmacol. 180, 114147 (2020). [Google Scholar] [Cross Ref]
- Ghlichloo I, Gerriets V. Nonsteroidal anti-inflammatory drugs (NSAIDs). [Google Scholar]
- Marginean MO, Meliț LE, Mocanu S, Sasaran V. Ibuprofen, a potential cause of acute hemorrhagic gastritis in children - a case report. J. Crit. Care Med. 4(4), 143-146 (2018). [Google Scholar] [Cross Ref]
- Bjarnason I, Scarpignato C, Holmgren E, et al. Mechanisms of damage to the gastrointestinal tract from nonsteroidal anti-inflammatory drugs. Gastroenterology. 154(3), 500-514 (2018). [Google Scholar] [Cross Ref]
- Nagano Y, Matsui H, Tamura M, et al. NSAIDs and acidic environment induce gastric mucosal cellular mitochondrial dysfunction. Digestion. 85(2), 131-135 (2012). [Google Scholar] [Cross Ref]
- Peskar BM. Role of cyclooxygenase isoforms in gastric mucosal defense. J. Physiol-Paris. 95(1-6), 3-9 (2001). [Google Scholar] [Cross Ref]
- Rouzer CA, Marnett LJ. Cyclooxygenases: structural and functional insights. J. Lipid Res. 50, S29-34 (2009). [Google Scholar] [Cross Ref]
- Sostres C, Gargallo CJ, Lanas A. Nonsteroidal anti-inflammatory drugs and upper and lower gastrointestinal mucosal damage. Arthritis Res. Ther. 15(3), 1-8 (2013). [Google Scholar] [Cross Ref]
- Lanas A, Garcia RLA, Polo TM, Ponce M, Alonso AI, Perez AMA. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Off. j. Am. Coll. Gastroenterol. | ACG. 104(7), 1633-1641 (2009). [Google Scholar] [Cross Ref]
- Rainsford KD, Whitehouse MW. Paracetamol [acetaminophen]-induced gastrotoxicity: revealed by induced hyperacidity in combination with acute or chronic inflammation. Inflammopharmacology. 14, 150-154 (2006). [Google Scholar] [Cross Ref]
- Bannwarth B. Gastrointestinal safety of paracetamol: is there any cause for concern? Expert Opin. Drug Saf. 3(4), 269-272 (2004). [Google Scholar] [Cross Ref]
- Anderson BJ. Paracetamol (Acetaminophen): mechanisms of action. Pediatric Anesthesia. 18(10), 915-921 (2008). [Google Scholar] [Cross Ref]
- Coskuner I, Yilmaz TE. Awareness among patients taking oral non-steroidal anti-inflammatory drugs as analgesics: a cross-sectional study. J. Health Sci. Med. 4(1), 63-70 (1989). [Google Scholar] [Cross Ref]
- Guindon J, LoVerme J, De Lean A, Piomelli D, Beaulieu P., Synergistic antinociceptive effects of anandamide, an endocannabinoid, and nonsteroidal anti-inflammatory drugs in peripheral tissue: a role for endogenous fatty-acid ethanolamides? Eur. J. Pharmacol. 550(1-3), 68-77 (2006). [Google Scholar] [Cross Ref]
- Pendeville PE, Van Boven MJ, Contreras V, et al. Ketorolac tromethamine for postoperative analgesia in oral surgery. Acta Anaesthesiol. Belg. 46(1), 25-30 (1995). [Google Scholar] [Cross Ref]
- Forbes JA, Kehm CJ, Grodin MC, Beaver WT. Evaluation of ketorolac, ibuprofen, acetaminophen, and an acetaminophen-codeine combination in postoperative oral surgery pain. Pharmacotherapy. 10(6P2), 94S-105S (1990). [Google Scholar] [Cross Ref]
- Bakshi R, Jacobs L. D, Lehnert S, Picha B, Reuther J., A double-blind, placebo-controlled trial comparing the analgesic efficacy of two formulations of diclofenac in postoperative dental pain. Curr. Ther. Res. 52(3), 435-442 (1992). [Google Scholar] [Cross Ref]
- Lima PP, Fontanella V. Analgesic efficacy of aceclofenac after surgical extraction of impacted lower third molars. Int. J. Oral Maxillofac. Surg. 35(6), 518-521 (2006). [Google Scholar] [Cross Ref]
- Seymour RA, Frame J, Negus TW, Hawkesford JE, Marsden J, Matthew IR., The comparative efficacy of aceclofenac and ibuprofen in postoperative pain after third molar surgery. Br. J. Oral Maxillofac. Surg. 36(5), 375-379 (1998). [Google Scholar] [Cross Ref]
- Derry CJ, Derry S, Moore RA, McQuay HJ., Single dose oral naproxen and naproxen sodium for acute postoperative pain in adults. Cochrane Database of Systematic Reviews. 2009(1). [Google Scholar] [Cross Ref]
- Weisman SM, Brunton S. Efficacy and safety of naproxen for acute pain. J. Fam. Pract. 69(7 Suppl), S33-S38 (2020). [Google Scholar] [Cross Ref]
- Gazal G, Al-Samadani KH. Comparison of paracetamol, ibuprofen, and diclofenac potassium for pain relief following dental extractions and deep cavity preparations. Saudi Med. J. 38(3), 284 (2017). [Google Scholar] [Cross Ref]
- Zuniga JR, Phillips CL, Shugars D, et al. Analgesic safety and efficacy of diclofenac sodium softgels on postoperative third molar extraction pain. J. Oral Maxillofac. Surg. 62(7), 806-815 (2004). [Google Scholar] [Cross Ref]
- Mohammad S, Singh V, Wadhwani P, Tayade HP, Rathod O. K., Sublingual piroxicam in the management of postoperative pain after surgical removal of impacted mandibular third molar. Indian J. Dent. Res. 23(6), 839 (2012). [Google Scholar] [Cross Ref]
- Yee J., xPharm: The comprehensive pharmacology reference. Elsevier, (2008). [Google Scholar]
- Norn S, Kruse PR, Kruse E., History of opium poppy and morphine. Dansk Medicinhistorisk Arbog. 33, 171-184 (2005). [Google Scholar] [Cross Ref]
- Dhaliwal A, Gupta M., Physiology, opioid receptor. [Google Scholar] [Cross Ref]
- Camilleri M, Lembo A, Katzka D. A., Opioids in gastroenterology: treating adverse effects and creating therapeutic benefits. Clin. Gastroenterol. Hepatol. 15(9), 1338-1349 (2017). [Google Scholar] [Cross Ref]
- Schwenk E. S, Mariano E.R., Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J. Anesthesiol. 71(5), 345-352 (2018). [Google Scholar] [Cross Ref]
- Paladini A, Varrassi G. Multimodal pharmacological analgesia in pain management. Pain Manag. Pract. Novel Ther. Bioactives. (2020). [Google Scholar] [Cross Ref]
- Zhang H, Zhang J, Streisand JB. Oral mucosal drug delivery: clinical pharmacokinetics and therapeutic applications. Clin. Pharmacokinet. 41, 661-680 (2002). [Google Scholar] [Cross Ref]
- Puntillo F, Giglio M, Varrassi G. The routes of administration for acute postoperative pain medication. Pain Ther. 10(2), 909-925 (2021). [Google Scholar] [Cross Ref]
- Leppert W, Malec-Milewska M, Zajaczkowska R, Wordliczek J., Transdermal and topical drug administration in the treatment of pain. Molecules. 23(3), 681 (2018). [Google Scholar] [Cross Ref]
- Prausnitz MR, Langer R. Transdermal drug delivery. Nat. Biotechnol. 26(11), 1261-1268 (2008). [Google Scholar] [Cross Ref]
- Lam JK, Cheung CC, Chow MY, et al. Transmucosal drug administration as an alternative route in palliative and end-of-life care during the COVID-19 pandemic. Adv. Drug Deliv. Rev. 160, 234-243 (2020). [Google Scholar] [Cross Ref]
- De Boer AG, Moolenaar F, De Leede LG, Breimer DD., Rectal drug administration: clinical pharmacokinetic considerations. Clin. Pharmacokinet. 7, 285-311 (1982). [Google Scholar] [Cross Ref]
- Kahraman E, Gungor S, Ozsoy Y. Nasal delivery of high molecular weight drugs: recent trends and clinical evidence. In: Nasal Drug Delivery: Formulations, Developments, Challenges, and Solutions. Springer, Cham. (2023). p. 253-277. [Google Scholar] [Cross Ref]
- Lofts A, Abu-Hijleh F, Rigg N, Mishra RK, Hoare T. Using the intranasal route to administer drugs to treat neurological and psychiatric illnesses: rationale, successes, and future needs. CNS Drugs. 36(7), 739-770 (2022). [Google Scholar] [Cross Ref]
- Swain A, Nag DS, Sahu S, Samaddar DP. Adjuvants to local anesthetics: current understanding and future trends. World J. Clin. Cases. 5(8), 307 (2017). [Google Scholar] [Cross Ref]
- Chitnis SS, Tang R, Mariano ER. The role of regional analgesia in personalized postoperative pain management. Korean J. Anesthesiol. 73(5), 363-371 (2020). [Google Scholar] [Cross Ref]
- Krishnasamy S, Abell TL. Diabetic gastroparesis: principles and current trends in management. Diabetes Ther. 9, 1-42 (2018). [Google Scholar] [Cross Ref]
- Farrell B, Pottie K, Thompson W, Boghossian T, Pizzola L, Rashid FJ, et al. Deprescribing proton pump inhibitors: evidence-based clinical practice guideline. Can. Fam. Physician. 63(5), 354-364 (2017). [Google Scholar] [Cross Ref]
- McCarthy DM. Helicobacter pylori and non-steroidal anti-inflammatory drugs: does infection affect the outcome of NSAID therapy? Yale J. Biol. Med. 71(2), 101 (1998). [Google Scholar] [Cross Ref]
- Dixon MF. Pathology of gastritis and peptic ulceration. In: Mobley HLT, Mendz G. L, Hazell S. L., editors. Helicobacter pylori: Physiology and Genetics. Washington (DC): ASM Press; 2001. [Google Scholar] [Cross Ref]
- Pasternak GW, Pan YX. Mu opioids and their receptors: evolution of a concept. Pharmacol. Rev. 65(4), 1257-1317 (2013). [Google Scholar] [Cross Ref]
- Khansari M, Sohrabi M, Zamani F. The usage of opioids and their adverse effects in gastrointestinal practice: a review. Middle East J. Dig. Dis. 5(1), 5 (2013). [Google Scholar] [Cross Ref]
- Jain M, Wylie WP. Diphenoxylate and Atropine. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2023 Jan-. [Google Scholar] [Cross Ref]
- Morgan MM, Christie MJ. Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human. Br. J. Pharmacol. 164(4), 1322-1334 (2011). [Google Scholar] [Cross Ref]
- Schou WS, Ashina S, Amin FM, Goadsby PJ, Ashina M. Calcitonin gene-related peptide and pain: a systematic review. J. Headache Pain. 18(1), 1-7 (2017). [Google Scholar] [Cross Ref]
- Hawkey CJ, Langman MJ. Non-steroidal anti-inflammatory drugs: overall risks and management. Complementary roles for COX-2 inhibitors and proton pump inhibitors. Gut. 52(4), 600-608 (2003). [Google Scholar] [Cross Ref]
- Kedir HM, Sisay EA, Abiye AA. Enteric-coated aspirin and the risk of gastrointestinal side effects: a systematic review. Int. J. Gen. Med. 14, 4757-4763 (2021). [Google Scholar] [Cross Ref]
- Harish S, Bhuvana K, Bengalorkar GM, Kumar TN. Flupirtine: clinical pharmacology. J. Anaesthesiol. Clin. Pharmacol. 28(2), 172 (2012). [Google Scholar] [Cross Ref]