Case Report - Interventional Cardiology (2017) Volume 9, Issue 4
An unusual case of arrhythmic palpitations in a volleyball player
- Corresponding Author:
- Zefferino Palamà
Cardiology Unit, Policlinico Casilino, Rome, Italy
Tel: +390623188406
E-mail: zefferino.palama@icloud.com
Abstract
A case of a 31 years old woman volleyball player highly symptomatic for arrhythmic palpitations is reported. The woman was disqualified from competitive sport and referred to our centre for atrial fibrillation (AF) ablation. During symptoms surface ECG had documented irregular supraventricular tachyarrhythmia interpreted as AF. Electrophysiological study could reveal double-His conduction as the true arrhythmia mechanism and the patient was successfully treated with nodal slow pathway ablation. Patient was totally asymptomatic at a 12 months follow up and he was readmitted to competitive sport. The case further underlines the concept that young subjects with suspected lone AF should undergo to a careful clinical evaluation in order to reconstruct the exact electrophysiological mechanism to plan a safe and effective therapy.
Keywords
Arrhythmic palpitations, Volleyball player, Atrial fibrillation, Double His
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered in clinical practice. The prevalence of the arrhythmia increases with age [1]. However, increasing evidence indicates that paroxysmal AF can also onset in young or middle-aged subjects or otherwise healthy athletes: the so called ‘PAFIYAMA’ (‘paroxysmal AF in young and middle-aged athletes’) [2].
Pulmonary veins ablation is known to be an effective therapy to treat symptomatic AF patients, even if the risks related to the procedure are still not neglectable. However, in order to increase the benefit/risk ratio of any ablation it could be important to better define the underlying electrophysiological mechanism of the arrhythmia. This could help to plan a safe and more effective therapeutic approach.
Clinical Case
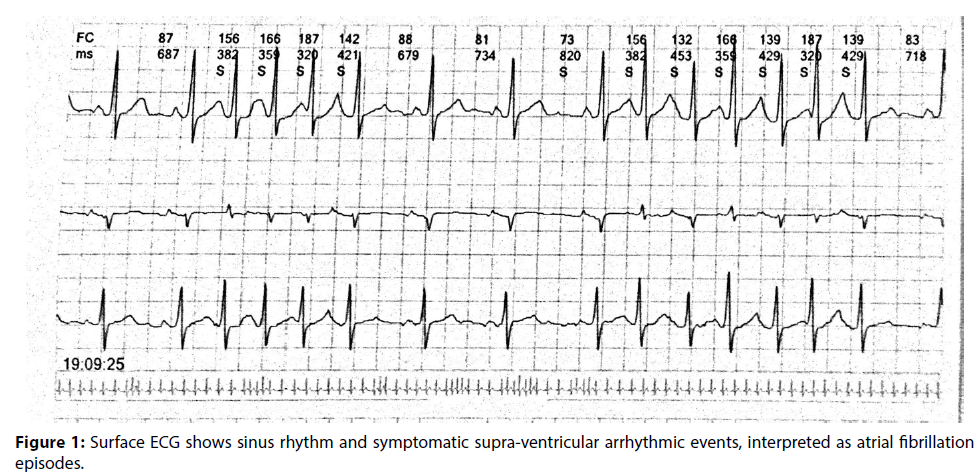
A 31 years old woman was referred to our Hospital for long lasting palpitations with ECG evidence of short-term episodes of atrial arrhythmia interpreted as AF. The arrhythmia was refractory to multiple antiarrhythmic drugs (Figure 1). The patient was a competitive volleyball player, but she had been disqualified from sport because of the episodes of palpitations during physical activities. No significant diseases were present on her past medical history. Physical examination was unremarkable. Echocardiographic evaluation didn’t show any significant pathological finding.
Patient was referred to our centre for electrophysiological (EP) study and eventual AF ablation.
Informed consent was obtained for EP study and ablation. The procedure was performed in a non-sedated, fasting state. Three catheters were introduced through femoral veins: a quadripolar catheter was placed in right ventricle, a decapolar catheter was placed inside coronary sinus and a mapping quadripolar steerable catheter was placed in His bundle region.
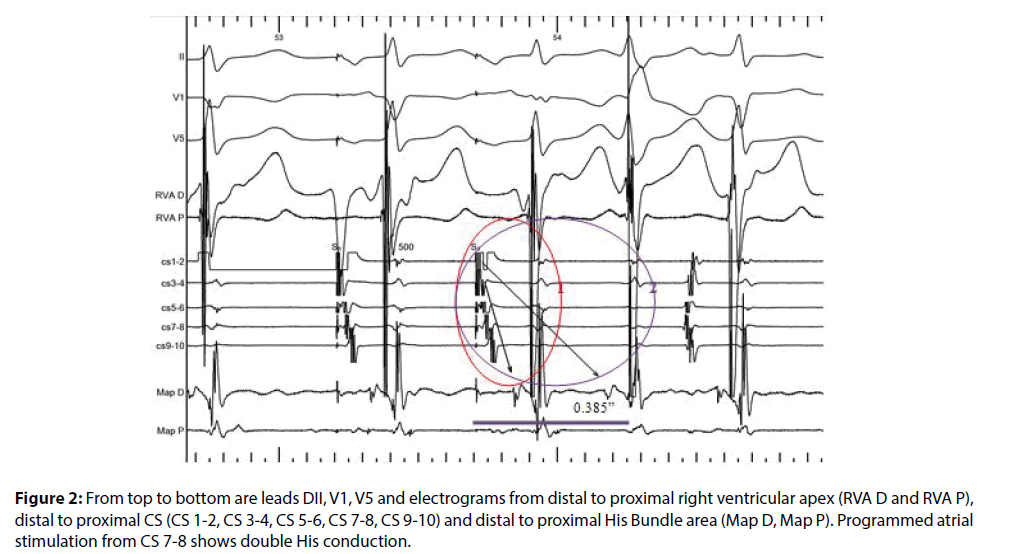
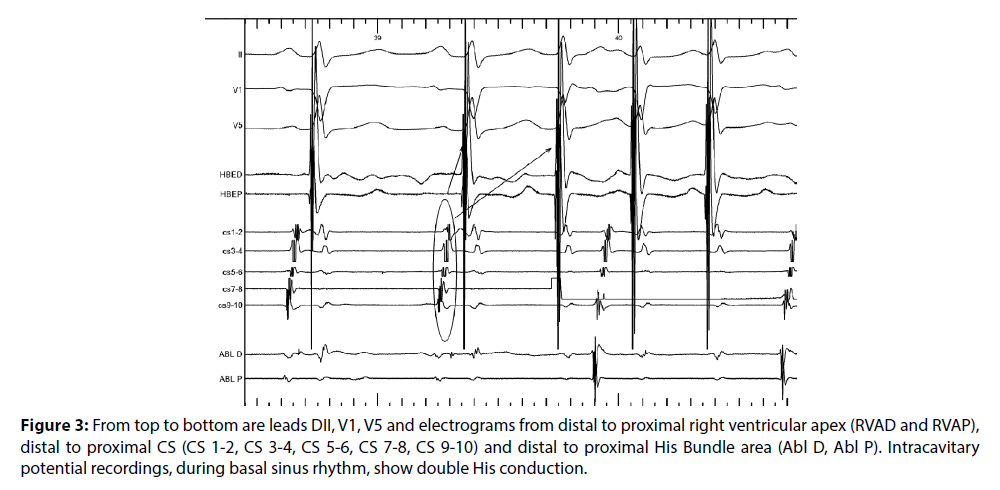
Baseline recordings showed normal AH and HV interval. Ventricular pacing showed dissociated ventricular-atrial (VA) conduction, excluding the presence of concealed accessory pathways. Programmed atrial stimulation showed double nodal pathway conduction and reproducible evidence of double-His conduction with a single extrastimulus (Figure 2): an atrial extrastimulus was followed by two ventricular beats with different AH interval. The same phenomenon was also recorded after a normal sinus beat as shown in Figure 3. From the second beat, after every P wave (visible in surface leads DI, V1 and V5) we can see an atrial potential (visible in the coronary sinus tracings CS), and two his-ventricular potentials (visible in the ventricular tracings RVA). The fast and irregular heart rate during this phenomenon was perceived by the patient as palpitations.
Figure 2: From top to bottom are leads DII, V1, V5 and electrograms from distal to proximal right ventricular apex (RVA D and RVA P), distal to proximal CS (CS 1-2, CS 3-4, CS 5-6, CS 7-8, CS 9-10) and distal to proximal His Bundle area (Map D, Map P). Programmed atrial stimulation from CS 7-8 shows double His conduction.
Figure 3: From top to bottom are leads DII, V1, V5 and electrograms from distal to proximal right ventricular apex (RVAD and RVAP), distal to proximal CS (CS 1-2, CS 3-4, CS 5-6, CS 7-8, CS 9-10) and distal to proximal His Bundle area (Abl D, Abl P). Intracavitary potential recordings, during basal sinus rhythm, show double His conduction.
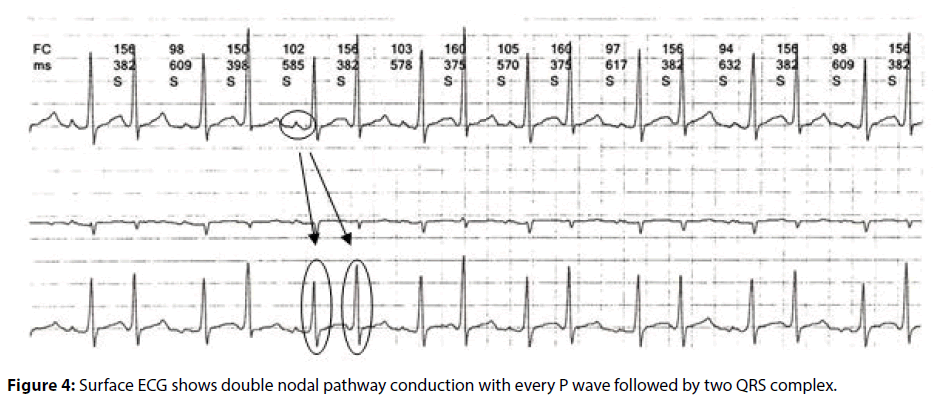
If we carefully analyze another surface ECG, recorded during palpitations, we can appreciate the presence of double QRS after every spontaneous sinus P wave (Figure 4). In order to eliminate the arrhythmic events, slow pathway ablation was performed. Ablation catheter was anatomically positionated in the posterior region of the Koch’s triangle where the slow pathway potential was recorded. Two pulse of RF (50 W, 60°C) were applied near CS ostium where small amplitude, multicomponent atrial electrogram and a large ventricular electrogram were recorded on the ablator distal bipole, corresponding to the endocardial site of the slow pathway. an Application of RF energy on this site was associated to the induction of many junctional beats, indicating effective ablation.
After ablation programmed atrial stimulation showed no double nodal pathway conduction nor arrhythmia inducibility during a 30 min observation period. Effective AV nodal refractory period was subsequently elicited at a coupling interval of 300 msec. No evidence of double-His conduction was observed after ablation.
A 12 months clinical follow-up showed no arrhythmic recurrences. One month after procedure patient was able to resume her sport activity.
Discussion
This case refers to a young volleyball player who had been pharmacologically treated for a long time for arrhythmic palpitations interpreted as short runs of AF. Because of invalidating symptoms, patient was disqualified from sport activity. In case of young subjects with suspected AF, we always have to consider the presence of possible supraventricular tachycardia (SVT) that may trigger or mimic AF [3,4]. A significant proportion of candidates to AF ablation could be inducible for a SVT at EP study and SVT ablation showed a strong preventive effect on AF recurrences. The presence of this arrhythmic trigger is more frequent in young patients without significant structural heart disease [5]. The identification of a precise mechanism of AF induction can avoid useless and long ablative procedures.
The identification of the correct arrhythmia mechanism in our patient, consisting in the rare phenomenon of the double-His conduction, allowed us to avoid unuseful wide ablative lesions. It is important to consider that the EP mechanism of arrhythmia induction could have been suspected at a careful surface ECG analysis. In fact, the surface ECG shows the possible presence of double nodal pathways, as further confirmed by the electrophysiological study [6,7]. This is a rare phenomenon and it is very important to recognize it in order to plan an effective and safe ablative therapy. In this case, a simple ablation of the slow pathway enabled us to treat a complex clinical trouble.
Perspective
Catheter ablation could be an effective solution in many athletes with arrhythmias [8,9]. Double-His conduction [3,4] is a rare phenomenon that can be responsible of invalidating symptoms even in young patients with structurally normal hearts and in athletes. Careful clinical workout and detailed surface ECG analysis help to identify or suspect uncommon arrhythmia mechanism and to plan a safe and effective curative ablative strategy.
References
- Writing M, Lloyd-Jones D, Adams RJ, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 121: e46-e215 (2010).
- Gomar F, Perez-Quilis C, Lippi G, et al. Atrial fibrillation in highly trained endurance athletes—Description of a syndrome. Int. J. Cardiol. 226: 11-20 (2017).
- Rostock T, Sanders P, RotterM, Haïssaguerre M. Sinus rhythm mimicking atrial fibrillation recurrence. Heart. Rhythm. 2(10): 1158 (2005).
- Mansour M, Marrouche N, Ruskin J, Natale A, Keane D. Incessant nonreentrant tachycardia due to simultaneous conduction over dual atrioventricular nodal pathways mimicking atrial fibrillation in patients referred for pulmonary vein isolation. J. Cardiovasc. Electrophysiol. 14(7): 752-755 (2003).
- Sciarra L, Rebecchi M, De Ruvo E, et al. How many atrial fibrillation ablation candidates have an underlying supraventricular tachycardia previously unknown? Efficacy of isolated triggering arrhythmia ablation. Europace. 12(12): 1707-1712 (2010).
- Arena G, Bongiorni MG, Soldati E, Gherarducci G, Mariani M. Incessant nonreentrant atrioventricular nodal tachycardia due to multiple nodal pathways treated by radiofrequency ablation of the slow pathways. J. Cardiovasc. Electrophysiol. 10(12): 1636-1642 (1999).
- Sakurada H, Sakamoto M, Hiyoshi Y, et al. Double ventricular response to a single atrial depolarization in a patient with dual AV nodal pathways. Pacing. Clin. Electrophysiol. 15: 28-33 (1992).
- Furlanello F, Lupo P, Pittalis M, et al. Radiofrequency catheter ablation of atrial fibrillation in athletes referred for disabling symptoms preventing usual training schedule and sport competition. J. Cardiovasc. Electrophysiol. 19(5): 457-462 (2008).
- Grazioli G, Fernández-Armenta J, Prat S, et al. Ablation of frequent premature ventricular complex in an athlete. Scand. J. Med. Sci. Sports. 25(6): 876-879 (2015).