Research Article - Journal of Interventional Nephrology (2018) Volume 1, Issue 1
Analysis of internal jugular catheter (IJC) inserted by a nephrologist for haemodialysis in a kidney care center in Nigeria.
- Corresponding Author:
- Okafor UH
Renal Unit, Department of Medicine, Enugu State University Teaching Hospital Parklane Enugu, Nigeria
E-mail: umehughes@yahoo.com
Abstract
Background: Internal jugular catheter is an important vascular access, and plays a critical role in haemodialysis. It can be used for both salvage (acute) and maintenance (chronic) haemodialysis. The objective of the study was to analyze the outcome of internal jugular catheter inserted by a nephrologist for haemodialysis in a kidney care center in Nigeria.
Methodology: This was a prospective non randomized study. All patients who had IJC inserted at the center (Hilton Clinics) from 1st October 2011 to 31st September 2016 who gave consent were recruited for the study. Their bio data, clinical parameters and details of their IJC insertion were documented. The data obtained was analysed with SPSS version 22.
Results: A total of 129 patients were recruited for the study, and they had 150 IJC insertions. There were 59.7% males and 40.3% females with a ratio of 1.5:1. The age range was 12 to 84 years and mean age was 51.4±15.2 years. Hypertension and chronic glomerulonephritis were the commonest cause of kidney failure. All the patients had haemodialysis using femoral catheters before IJC was inserted, 96.9% had right IJC, 80.7% had tunneled IJC, 74.4% had one insertion, 3.1% three insertions. Infection was the commonest complication and it is the commonest reason for removal or replacement of catheter.
Conclusion: Internal jugular catheter insertion for haemodialysis by a nephrologist is viable and has good outcome.
Keywords
Internal jugular, Catheter, Insertion, Haemodialysis, Nephrologist
Introduction
Haemodialysis is the most available renal replacement therapy for patients with acute or chronic kidney failure in most countries [1,2]. Central venous catheter is the commonest vascular access used for haemodialysis in most developing nations [1,3,4]. Hitherto femoral vein was the only vascular access used for haemodialysis in most centers in Nigeria. This was attributed to lack of skill to use other vascular access. This caused marked limitation in managing chronic kidney disease patients requiring maintenance haemodialysis.
However, recently nephrologist in Nigeria including one of the authors acquired the requisite skill to insert and maintain both tunneled and non-tunneled central venous catheters using internal jugular and subclavian veins.
The right internal jugular vein (IJV) is a preferred route for hemodialysis catheters, for its ease in identification, big size and unhindered straight passage to the right atrium [5,6]. This is also the recommendation of National Kidney Foundation - Kidney Disease Outcome Quality Initiative (NKF - KDOQI) [7]. Although the left IJV and both subclavian vein (SCV) have been used for secondary access by most clinicians, several studies suggest that both should be avoided because of a high incidence of complications [7-9]. The right external jugular vein (EJV) had also been used as vascular access for hemodialysis as well as non-dialysis central vein catheter. The straight course, superficial location and similar blood flow as IJV are main advantages for its use [10].
Insertion of IJC requires in addition to skill, supporting facilities including Doppler ultrasound to locate the vessels, fluoroscopy to visualize the guide wire and X-ray machines to visualize the catheter and access complications [11]. In most centers in Nigeria including the study location Doppler ultrasound and fluoroscopy were not available. Thus use of anatomical landmark of the internal jugular vein and experience of the nephrologist plays key role in insertion of jugular catheter in most resource poor nations including Nigeria. There is scanty report on IJC insertion on haemodialysis patients in Nigeria.
The objective of the study was to analyze the outcome of internal jugular catheter inserted by a clinical nephrologist for haemodialysis in a kidney care center in Nigeria.
Methodology
This was a prospective non randomized study. The location of the study was Hilton clinics Port Harcourt, Rivers state, Nigeria. This is a private multispecialty hospital located in the oil rich region of Nigeria. The facility attends to patients from the Niger delta states of Nigeria and beyond. The hospital offers diagnostic and therapeutic services in kidney and kidney related diseases including kidney biopsy, renal replacement therapy, pre/post-transplant care and has facilities for in and outpatient services. There are 5 haemodialysis machines (4 NIPRO and 1NIKISSO). About 95% of haemodialysis patients in the center uses central venous catheters (CVC) access viz femoral vein, internal jugular catheter and subclavian vein. Only about 18% of the patients on CVC had internal jugular catheter and less than 1% had subclavian catheter as vascular access.
▪ Study population
The study population was haemodialysis patients who had internal jugular catheter inserted from 1st October 2011 to 30th September 2016. All patients presenting during the study period that met the inclusion criteria and gave consent were recruited.
▪ Study procedure
The study was approved by the ethical committee of the hospital. The details of the study were explained to all participating patients. Informed consent was obtained from each patient before recruiting them for the study. Only patients that gave consent were recruited. The patient’s bio data and clinical parameters, details of jugular catheter insertion, duration of the catheter and complications during and after the procedure were documented.
▪ Technique for internal jugular catheterization
The details of the procedure were explained to the patients and written consent for the procedure obtained.
Patients were positioned supine.
The head was turned away from the side of procedure.
Sand bag was placed between the scapula to extend the neck.
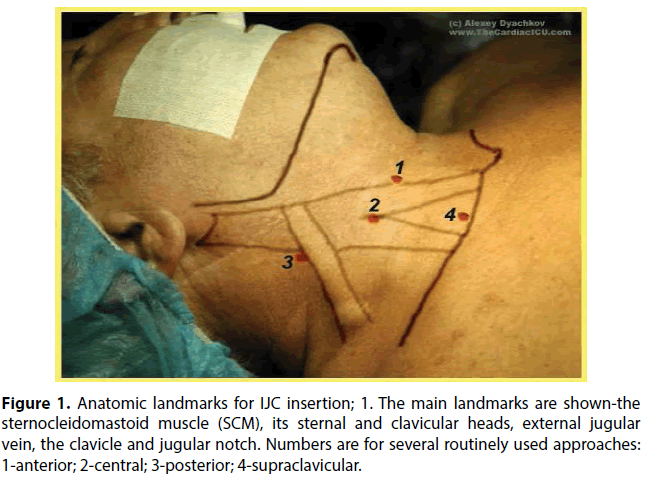
Relevant anatomy was determined using the landmark as in Figure 1 [12]. The area of puncture was identified; usually we used the top of the triangle between the sternal and clavicular head of the sternocleidomastoid muscle.
Figure 1: Anatomic landmarks for IJC insertion; 1. The main landmarks are shown-the sternocleidomastoid muscle (SCM), its sternal and clavicular heads, external jugular vein, the clavicle and jugular notch. Numbers are for several routinely used approaches: 1-anterior; 2-central; 3-posterior; 4-supraclavicular.
The skin was cleaned with chlorhexidine and ethanol from the mandible to the nipple, including the angle of the mandible, chin, and axilla. The cleaned area was covered with a drape exposing only the operating area.
The area of puncture was anaesthetized with 5 ml of plain 1% lignocaine
A finder needle connected to a 10 mL syringe was advanced through the skin at an approximately 60° angle and in the direction of the nipple until venous blood (dark) is aspirated. The syringe was detached from the needle and a guidewire was advanced into the vein through the needle. The guidewire was ensured to have a free movement and when satisfied with the length (about 10 cm) that has entered, the needle was removed.
The double lumen cuffed catheter was used to determine the exit point on the chest by measuring the length from the angle of Louis to the puncture site and curve to the chest wall and the exit site is determined 2-4 cm distal to the cuff.
A skin incision was made at the measured exit site and puncture site. A tunnel was made from the skin exit site on the chest to the puncture site using the tunneler.
The double lumen cuffed catheter was attached to the tunneler and pulled through the tunnel from the exit site out through the puncture site. The tunneler was detached from the catheter after the cuff has entered the tunnel to about 2-4 cm from skin exit site.
The puncture site was dilated using the dilators over the inserted guidewire. Then the catheter is advanced over the guidewire until the tip is estimated to be at a position corresponding to the angle of Louis. Occasionally the peel sheath was used (not regularly to minimize blood loss) and the catheter was passed through the sheath to the same length and the sheath was then removed.
The patency of the catheter was ascertained by aspirating blood freely through both lumen of the catheter. The lumens of the catheter were flushed with heparinized saline and subsequently locked with 2500 iu heparin and 40 mg gentamycin added to each lumen.
The incision on the neck was closed and the catheter was anchored at the exit site using nylon 2/0. Both were dressed after cleaning with chlorhexidine and iodine (Figure 2).
A post procedure chest X-ray was performed to confirm the position of the catheter tip and exclude complications (Figure 3).
Data analysis
The data obtained was entered into a spread sheet and analysed using IBM (New York) statistical package for social sciences version 22.
The results were presented in tables and charts as mean, standard deviation and frequencies. The P value of less than 0.05 was considered significant.
Result
A total of 129 (88.4%) of the 146 patients who had IJC catheterization during the study period gave consent for the study and were recruited. There were a total of 150 IJC insertions. There were 77 (59.7%) males and 52 (40.3%) females with a ratio of 1.5:1. The age range was 12 to 84 years with mean of 51.4±15.2 years. Majority of the patients (85.3%) were married and more than 60% of them were either in business or public service. The details of the demographic data are shown in Table 1.
| Male n (%) | Female n (%) | Total n (%) | p-value | |
|---|---|---|---|---|
| Age (years) <35 35-44 45-54 55-64 ≥65 |
- 9 (11.7) 13 (16.6) 22 (28.6) 18 (23.4) 15 (19.5) |
- 7 (13.5) 11 (21.2) 9 (17.3) 13 (25) 12 (23.1) |
- 16 (12.4) 24 (18.6) 31 (24) 31 (24) 27 (20.9) |
0.69 |
| Marital status Married Single Divorced Widowed |
- 69 (89.9) 7 (9.1) - 1 (1.3) |
- 41 (78.8) 7 (13.5) 1 (1.9) 3 (5.8) |
- 110 (85.3) 14 (10.9) 1 (0.8) 4 (3.1) |
0.22 |
| Occupation Public/civil servants Business Retired Unemployed Students others |
- 38 (49.4) 20 (26) 11 (14.3) 3 (3.9) 3 (3.9) 2 (2.6) |
- 12 (23.1) 11 (26.9) 10 (19.2) 14 (3.8) 5 (9.6) - |
- 50 (38.8) 31 (24) 21 (16.3) 17 (13.2) 8 (6.2) 2 (1.6) |
- |
| Total | 77 (59.7) | 52 (40.3) | 129 (100) | 0.03 |
Table 1. Demographic data of the patients.
Hypertension and chronic glomerulonephritis constitute the commonest cause of kidney failure. Five (4.0%) patients presented with graft failure resulting from rejection. The cause of kidney failure was not known in 16 (12.4%) patients including 2 patients with graft rejection. Table 2 shows the details of the causes of renal failure.
| Male (%) | Female (%) | Total (%) | |
|---|---|---|---|
| HTN | 25 (32.5) | 15 (28.8) | 40 (31) |
| CGN | 15 (19.5) | 17 (24.8) | 32 (24.8) |
| HIVAN | 11 (14.3) | 4 (7.7) | 15 (11.6) |
| DM | 12 (15.6) | 3 (5.8) | 15 (11.6) |
| OBN | 2 (2.6) | 3 (5.7) | 5 (3.9) |
| SCN | 1 (1.3) | 1 (1.9) | 2 (1.6) |
| KTPR | 1 (1.3) | 1 (1.9) | 2 (1.6) |
| KTPR/CGN | 1 (1.3) | 1 (1.9) | 2 (1.6) |
| KTPR/DM | 1 (1.9) | - | 1 (0.8) |
| VASCULITIS | 1 (1.3) | - | 1 (0.8) |
| UNKNOWN | 7 (9.1) | 7 (13.5) | 14 (10.8) |
| TOTAL | 77 (100) | 52 (100) | 129 (100) |
Table 2. Sex distribution of causes of renal failure; HTN-hypertension, CGN-chronic glomerulonephritis, HIV-human immunodeficiency virus associated nephropathy, SCN-sickle cell nephropathy, KTPR-kidney transplant rejection.
All the patients used femoral vein access when commencing haemodialysis with duration ranging from 1 to 52 weeks (mean of 10.1±8.7 weeks and median of 8 weeks) before internal jugular catheter was inserted. Four (3.1%) patients had left IJC while others (96.9%) had right IJC.
One hundred and seven (82.9%) patients had 121 (80.7%) tunneled IJC (tIJC) and 25 (19.4%) patients had 29 (19.3%) non tunneled IJC (ntIJC)
One hundred and twelve (86.8%) patients had only a single IJC insertion (74.4% tIJC, 17.8% ntIJC); 13 (10.1%) had IJC inserted 2 times (7 tIJC, 4 ntIJC), 4 (3.1%) patients had IJC inserted 3 times (4 tIJC) and 2 (1.6%) had their ntIJC replaced with tIJC. The indications for removal/replacement of IJC in these patients were as documented in Figure 4.
The duration of the procedure ranged from 20 to 210 minutes with a mean of 58.4±26.5 minutes (median of 55 minutes). One hundred and fifty catheters were inserted, 102 (68%) had a single puncture, 25 (16.7%) were punctured twice, 19 (12.7%) thrice, and 4 (2.7%) had more than 3 punctures. Two patients had the procedure abandoned after 3 punctures.
The duration patient used the tunneled and non-tunneled IJC were 1-88 and 1-8 weeks respectively, with a median of 10 and 4 weeks respectively.
Discussion
The demographic pattern of patients with chronic kidney disease in Nigeria showed that chronic kidney disease was commoner in the young adults, males and low socioeconomic status [13,14]. However in this study though males and those of low socioecomic status constitute the majority, more than 60% of them were aged 45 years and above. Probably the older population has a better family (children) support to afford the procedure.
Chronic glomerulonephritis and hypertensive nephrosclerosis constitute about 57% of causes of renal failure in this study and this is consistent with previous reports of causes of chronic kidney disease in Nigeria [3,4,15]. Patients with graft failure constitute 4% of the study population and all of them resulted from rejection of the graft. This is the first report of post-transplant patients constituting significant proportion of haemodialysis population in Nigeria. This highlights the increasing population of kidney transplant patients and need for improvement in post-transplant care.
Use of femoral vein as vascular access has been reported to be fraught with complications including thrombophlebitis of the iliac vein. This vein is used for anastomosis of the veins during kidney transplant. Thus use of femoral vein as haemodialysis access is discouraged and should be reserved mainly for emergency haemodialysis. However, in this study all the patients had prolonged use of femoral vein access before IJC was inserted. Ignorance, poverty and nonavailability of skill contributed to this prolonged use of femoral vein access.
The right internal jugular vein is commonly used because it has a straighter course and also less prone to complications associated with injury to thoracic duct, azygos vein and pneumothorax. Multiple punctures has also being associated with increasing risk of puncture related complication, thus it is recommended that the number of punctures should not exceed 3 times. Most of the patients in this study had right IJC; 68% of them were punctured once while 16.7%, 12.7% and 2.7% were punctured 2, 3 and 4 or more times respectively. This is comparable to the study that reported 59.7%, 14.9%, 14.9% and 10.4% for 1, 2, 3 and 4 and more punctures respectively [16]. Two of the procedures in this study were abandoned after 3 punctures; those that had more than 3 punctures were requested by the patients. The duration of the catheterization ranged from 10 to 210 minutes with a median of 55 minutes (21 minutes for ntIJC and 56 minutes for tIJC). The duration catheterization was longer in patients requiring multiple punctures, difficult procedure and anxious patients. Ultrasound guided techniques has been reported to reduces the number of punctures and the duration of catheterization [17,18].
Majority of the patients (82.9%) in this study had tIJC as it is more cost effective-stays longer and less prone to infection. The duration of IJC was between 1 and 88 weeks; this is consistent with other studies [16,19]. The IJC was replaced in 13% of the patients and reasons were mainly due to catheter dysfunction, infection and dislodgement, choice of the patient and long duration of the IJC. Furthermore IJC was removed in patient that improved, died and those that subsequently had atriovenous fistula access, and kidney transplant. The reasons for catheter removal/replacement in the study by Wang et al. [20] were catheter dysfunction, infection and atriovenous fistula.
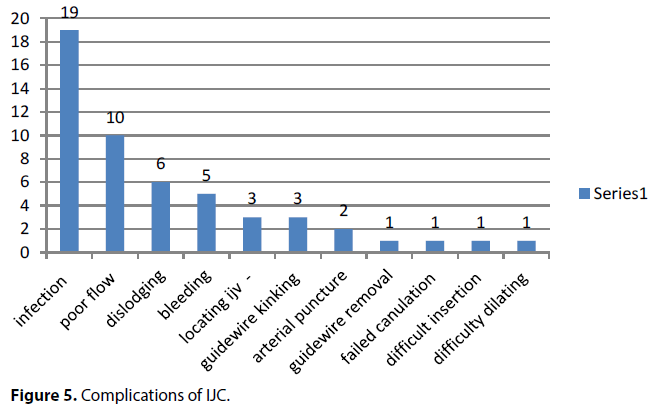
Challenges of insertion of central venous catheters for haemodialysis including internal jugular catheterization are its association with multiple complications (Figure 5). The complications may be catheter related and catheter unrelated, puncture related and puncture unrelated, early and late complications. Complications were reported in about 34.7% of the IJC insertions in this study. Chung et al. [19] reported complications in 33.6% in their study which is consistent with this study. However other authors had reported either lower or higher complications in their study; Kamanran et al. [21] 21.9%, El-Shahawy MA and Khilnani H [22] 43.2%, Gamtam et al. [16] 24.9%, 10% catheter related and 14.9% catheter unrelated.
Infection was the commonest complication in this study occurring in 14.7%. The infection could be at catheter exit site, tunnel, catheter tip or systemic including bacteremia/septicemia, and septic emboli causing endocarditis, arthritis, pneumonia etc. The infections noted in this study included exit site infection, septicemia and infective endocarditis. Various procedures has been recommended to reduce rate of infections in patients with IJC including aseptic protocol in inserting the catheters, antibiotic lock of the catheter after each haemodialysis, applying antibiotic cream at the exit site, antibiotic coating of the catheters, and active surveillance for infection [23,24].
Other complications reported in this study included poor blood flow(defined as blood flow less than 200 ml/min lasting more than 30 minutes) in 6.7%, spontaneous dislodging of the catheters in 4%, (83.3% of them with ntIJC), bleeding in 3.3%, difficult procedure in 4.7%, ( difficulty locating vein-2%; difficulty inserting guidewire-2%; difficult inserting catheter-0.67%; difficulty dilating the puncture-0.67%), arterial puncture in 1.3% and failed insertion in 0.67%. Apart from these complications in this study, other studies had also reported pneumothorax, chylothorax, stenosis of the innominate vein, fracture of the guide wire/catheter, accidental carotid artery/ jugular vein fistula, and thrombosis of the catheter etc [16,18,21,22].
Considering that due to unavailability of facilities for Doppler ultrasound and fluoroscopy, external landmark and chest X-ray were the guide used in this study; the outcome of IJC insertion in this study is good and comparable to those done in centers with the requisite facilities. This requires diligence and experience/skill to minimize the numerous complications associated with IJC insertion.
In conclusion, insertion of internal jugular catheter by a nephrologist for haemodialysis in resource poor nation is practicable and the outcome is good. This will improve haemodialysis and patients outcome in these developing nations.
Hence it is recommended that insertion of internal jugular catheters should be inculcated in curriculum of nephrology training. Nephrologist should be encouraged to insert internal jugular catheters in all eligible patients requiring haemodialysis. There will be need for policies in alleviating the cost of renal care including insertion of internal jugular catheters and other vascular access. The limitations of this study were small sample size.
References
- Pozo ME, Leow JJ, Groen RS, et al. An overview of renal replacement therapy and health care personnel deficiencies in sub-saharan africa. Transpl Int. 25(6): 652-657 (2012).
- McCann M, Einarsdottir H, Van Waeleghem JP, et al. Vascular access management III: Central venous catheters. J Ren Care. 36(1): 25-33 (2010).
- Eyo Effiong Ekpe, Udeme Ekirikpo. Challenges of vascular access in a new dialysis centre-Uyo experience. Pan Afr Med J. 7(1): 23 (2010).
- Okunola Y, Ayodele O, Akinwusi P, et al. Haemodialysis practice in resource limited setting in the tropics. Ghana Med J. 47(1): 4-9 (2013).
- Vascular Access Work G. Clinical practice guidelines for vascular access. Am J Kidney Dis. 48(1): S248-S273 (2006).
- Bannon MP, Heller SF, Rivera M. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy. 4: 27-39 (2011).
- National Kidney Foundation. III. NKF-K/DOQI Clinical Practice Guidelines for Vascular Access: update 2000. Am J Kidney Dis. 37: S137-S181 (2001).
- Agarwal AK. Central vein stenosis. Am J Kidney Dis. 61(6): 1001-1015 (2013).
- Trerotola SO, Kuhn-Fulton J, Johnson MS, et al. Tunneled infusion catheters: Increased incidence of symptomatic venous thrombosis after subclavian versus internal jugular venous access. Radiology. 217(1): 89-93 (2000).
- Cho SK, Shin SW, Do YS, et al. Use of the right external jugular vein as the preferred access site when the right internal jugular vein is not usable. J Vasc Interv Radiol. 17(5): 823-829 (2006).
- Docktor BL, Sadler DJ, Gray RR, et al. Radiologic placement of tunneled central catheters: Rates of success and of immediate complications in a large series. AJR. 173(2): 457-460 (1999).
- Dyachkov A. Internal jugular vein catheterization.
- Egbi OG, Okafor UH, Meibodei KE, et al. Prevalence and correlates of chronic kidney disease among civil servants in Bayelsa State, Nigeria. Nigerian J Clin Prac. 17(5): 602-607 (2014).
- Arogundade FA, Barsoum RS. CKD prevention in Sub-Saharan Africa: A call for governmental, nongovernmental, and community support. Am J Kidney Dis. 51(3): 515-523 (2008).
- Wokoma FS, Okafor HU. Haemodialysis experience with chronic kidney failure patients at the University of Portharcourt teaching hospital: an analysis of data of the first year of operation. TJN. 5(2): 97-104 (2010).
- Gautam SN, Bhatta SK, Shrestha BC, et al. Placement of double lumen central venous catheter for hemodialysis patients: an experience.
- Lin BS, Huang TP, Tang GJ, et al. Ultrasound-guided cannulation of the internal jugular vein for dialysis vascular access in uremic patients. Nephron. 78(4): 423-428 (1998).
- Aydin Z, Gursu M, Uzun S. Placement of hemodialysis catheters with a technical, functional, and anatomical viewpoint. Int J Nephrol. 5 (2012).
- Chung HY, Soo WK, Myong YN, et al. Percutaneous catheterization of the internal jugular vein for hemodialysis. Korean J Intern Med. 16(4): 242-246 (2001).
- Wang P, Wang Y, Qiao Y, et al. A Retrospective study of preferable alternative route to right internal jugular vein for placing tunneled dialysis catheters: right external jugular vein versus left internal jugular vein. PLoS ONE. 11(1): e0146411.
- Kamanran T, Zaheer K, Khan AA, et al. Applications and complications of subclavian vein catheterization for hemodialysis. J Coll Physicians Surg Pak. 13(1): 40-46 (2003).
- El-Shahawy MA, Khilnani H. Carotid-jugular arteriovenous fistula: a complication of temporary hemodialysis catheter. Am J Nephrol. 15(4): 332-336 (1995).
- Raad II, Hohn CD, Gilbreath BJ, et al. Prevention of central venous catheter-related maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol. 15(4): 231-238 (1994).
- Böhlke M, Uliano G, Barcellos FC. Hemodialysis catheter-related infection: Prophylaxis, diagnosis and treatment. J Vasc Access. 16(5): 347-355 (2015).