Research Article - Interventional Cardiology (2016) Volume 8, Issue 6
Anticoagulation with rivaroxaban after ultrasound-assisted catheter-directed thrombolysis in patients with intermediate highrisk pulmonary embolism a case series
- Corresponding Author:
- Peter Marschang
Department of Internal Medicine III (Cardiology, Angiology), Medical University of Innsbruck
Anichstr 35, A-6020 Innsbruck, Austria
Tel: +4351250481414
Fax: +4351250423310
E-mail: Peter.Marschang@i-med.ac.at
Submitted: 08 November 2016; Accepted: 25 November 2016; Published online: 29 November 2016
Abstract
Background: The optimal treatment for intermediate-high risk pulmonary embolism (PE) is still unclear and challenging. A new method for this entity is ultrasound-assisted catheter directed thrombolysis (USAT). The use of non-vitamin K antagonist anticoagulants (NOAC) is currently not recommended after thrombolysis. In our case series we tried to evaluate the efficacy and safety of NOAC treatment shortly after USAT. Methods and findings: We report five patients with intermediate-high risk pulmonary embolism who were successfully treated with rivaroxaban as post-procedural anticoagulation after USAT. The treatment was tolerated well with rapid clinical improvement and almost complete normalisation of right heart function (reduction of mean right to left ventricular (RV/LV) ratio from 1.22 (range 1.07-1.24) at baseline to 0.87 (range 0.76-1.07) three days after thrombolysis (p = 0.016). We observed one GUSTO moderate bleeding episode and a transient rise in creatinine in one patient, but no other adverse events. After 2.4 days (range 2-4 days), patients were switched from unfractionated heparin to rivaroxaban. Follow up-visit after three months showed normalisation of right heart function (RV/LV ratio 0.69 (range 0.65-0.81), no recurrent thrombotic events and no additional bleeding episodes. Conclusion: In our experience, USAT followed by post-procedural anticoagulation with rivaroxaban appears to be an effective treatment of intermediate-high risk pulmonary embolism.
Keywords
Anticoagulation, Pulmonary embolism, Catheter, Thrombolysis
Introduction
Intermediate-high risk pulmonary embolism (PE), which is characterized by evidence of both right heart dysfunction on an imaging test and elevated cardiac laboratory biomarkers [1], carries a significant risk of short term mortality (up to15% within the first 3 months) [2].
Although systemic thrombolysis has been shown to be an effective treatment for this patient group, it has the disadvantage of a substantial bleeding risk including intracranial haemorrhage [3]. In contrast, ultrasound-assisted catheter-directed thrombolysis (USAT) uses only a fraction (10-20%) of the thrombolytic dose and may therefore be able to restore right heart function without a substantial increase in bleeding risk [4,5].
After acute treatment with USAT, these patients need further anticoagulant treatment to prevent recurrent venous thromboembolism (VTE) [6]. Non- vitamin K antagonist anticoagulants (NOAC) provide numerous advantages compared to vitamin K antagonists but are currently not recommended for patients receiving thrombolytic treatment.
Here, we report a case series of five patients who were successfully treated with USAT followed by post-procedural anticoagulation with rivaroxaban at our department.
Characteristics of Cases
Between October 2013 and June 2015, five (age 51- 82) patients with confirmed symptomatic intermediate high-risk PE were treated as described below. In each case, extensive pulmonary emboli with central involvement of the main pulmonary arteries (bilateral except for patient 4) were detected by multi-detector computed tomography. Epidemiologic and laboratory findings are summarized in Table 1. Clinical parameters and pulmonary embolism severity index (PESI) are shown in Table 2.
| No. | age | gender | relevant history | Trop-T (ng/l) | D-dimer (µg/l) | NT-pro-BNP (ng/l) |
|---|---|---|---|---|---|---|
| 1 | 77 | female | prior DVT and PE, CKD stage III | 27.5 | 12453 | 8352 |
| 2 | 82 | male | - | 156.9 | 9083 | 3781 |
| 3 | 73 | male | coronary artery bypass grafting | 26.3 | 19811 | 3445 |
| 4 | 81 | female | pneumonia left lower lobe | 31.5 | 25329 | 1456 |
| 5 | 51 | male | prior DVT(2x), bladder cancer, COPD II | 122 | 12960 | 3722 |
PE: Pulmonary Embolism
CKD: Chronic Kidney Disease
COPD: Chronic Obstructive Pulmonary Disease
Laboratory references values: Trop-T (0.0-14.0 ng/l), D-dimer (0-500 μg/l), NT-pro-BNP (0-172 ng/l)
Table 1: Epidemiologic and baseline laboratory parameters.
| Patient No | heart rate (bpm) | systolic arterial pressure (mmHg) | respiratory rate (breaths/min) | oxygen saturation at ambient air(%) | PESI score | PESI class |
|---|---|---|---|---|---|---|
| 1 | 97 | 163 | 16 | 84 | 97 | III |
| 2 | 104 | 107 | 12 | 92 | 92 | III |
| 3 | 100 | 144 | 25 | 70 | 163 | V |
| 4 | 107 | 90 | 18 | 82 | 131 | V |
| 5 | 128 | 100 | 20 | n.a.* | 141 | V |
Table 2: Clinical parameters and pulmonary embolism severity index (PESI) at baseline.
In each case, the decision to perform USAT was made based on the severity of PE-related symptoms and the absence of improvement under standard anticoagulation therapy after obtaining full informed consent.
Case I
A 77-year-old woman was admitted to our hospital with a recent onset of dyspnea and precordial pressure. She had a history of prior pulmonary embolism and deep vein thrombosis (DVT) 12 years ago as well as chronic kidney disease stage III and long-standing arterial hypertension. On admission, the laboratory evaluation revealed an increase in D-dimer, troponin T and NT-proBNP. The electrocardiogram (ECG) showed a slightly elongated PQ interval (210 msec), a concordant negative T wave in III and a slowly rising R wave in the precordial leads. Overall, the pulmonary embolism severity index (PESI) score was 97 (Class III). Multidetector computed tomography (MDCT) showed bilateral, extensive pulmonary emboli with central involvement of the right main pulmonary artery. Echocardiography showed significant right heart enlargement (right-to left ventricular ratio 1.07) and moderate tricuspid regurgitation. Ultrasound of the lower extremity veins showed proximal thrombosis of the right great saphenous vein as probable source. Since no improvement in the patients clinical condition was observed, ultrasound - assisted catheter-directed thrombolysis was performed.
Case II
An 82-year old man without a history of relevant comorbidities came with vertigo and chest pain, both since 3-4 weeks, to our emergency department. Additionally, he had syncope with a short time period of unconsciousness on the day of admission, resulting in an excoriation on the head. Shortly afterwards he presented himself orientated and awake at our department. His ECG showed an elongated PQ interval as well as concordant negative T-waves in V3 and V4. The evaluation showed a PESI-score of 92. His laboratory report revealed elevated D-dimer, troponin T and NT-pro- BNP (Table 2). Imaging methods detected bilateral pulmonary embolism with central affection of the main pulmonary arteries and significant dilation of the right ventricle, reduction in right ventricular ejection fraction and the presence of a McConnell sign. Sonography showed a completely occluded left popliteal vein. After initial stabilisation, the patient showed a marked deterioration with a blood pressure drop to 100/60 mmHg and dyspnoea with a high oxygen demand (10 L/min). After exclusion of an intracranial haemorrhage by MDCT, decision for ultrasound - assisted catheter-directed thrombolysis was made due to his worsened clinical condition.
Case III
A 73-year old patient was referred to our emergency department in a pre-syncopal condition in reduced general condition. One month ago, coronary artery bypass grafting had been performed. He suffered from severe dyspnea with an oxygen saturation of 70% without oxygen supplementation and 90% with oxygen supplementation (6 L/min) and tachycardia. The PESI score added up to 163 points (Class V) and the ECG showed a prolonged PQ-interval, a total right bundle branch block and a left anterior fascicular block. His laboratory markers showed an elevated D-Dimer, troponin- T and NT-proBNP. MDCT displayed extensive bilateral pulmonary embolism with involvement of the main pulmonary arteries. Echocardiography revealed right ventricular dysfunction, a dilation of the right pulmonary artery, paradox septum movement, the presence of a D-sign and moderate tricuspid regurgitation. Compression venous ultrasonography indicated the presence of an acute thrombosis in the right superficial femoral vein and also in the fibular vein on the same side. Due to the clinical presentation and significant right heart overload the decision for ultrasound - assisted catheter-directed thrombolysis with rtPA was made.
Case IV
An 81-year old woman was admitted at our emergency department with an acute onset of dyspnea, vertigo, nausea and emesis. About 10 months before she had been admitted with pneumonia of the left lower lobe at our hospital. In addition she had a history of hypertension. Initially, her general condition was reduced with a blood pressure rate of 90/53 mmHg and an oxygen saturation of 82% without supplementation. Overall, her PESI-score was 131. The ECG showed an elongated QT-interval, a SI/QIII-type and an incomplete right branch bundle block. In the MDCT central pulmonary embolism involving mainly the right pulmonary artery was detected. The laboratory parameters displayed an elevated D-dimer, troponin T and NT-proBNP. Subsequently, the patient could be stabilized haemodynamically with mean blood pressure values of 102/79 mmHg. The echocardiographic findings included signs of a right heart overload, a moderate to high tricuspid regurgitation and a small pericardial effusion. Ultrasound revealed a non-recent thrombosis in the left superficial femoral vein and in the popliteal vein. Without marked improvement regarding the clinical and laboratory parameters as well as a persistent right heart dysfunction, the patient underwent ultrasound -assisted catheter-directed thrombolysis.
Case V
A 51-year old man reported shortness of breath since a few days and chest pain the day before when he presented at the outpatient department. He had a history of 2 episodes of DVT one year ago and 5 years ago, bladder cancer and chronic pulmonary lung disease (COPD) grade II. The patient had been treated with rivaroxaban (1 × 20 mg/day) but due to a dental procedure the medication had been interrupted for one month before the event. At the time when he was referred to the coronary care unit (CCU), the patient was stable in terms of cardiorespiratory parameters. Nevertheless, his PESI score revealed 141 points. The ECG displayed tachycardia and the onset of a new right branch bundle block. Laboratory parameters showed marked elevation of D-dimer, troponin T and NT-pro-BNP. The echocardiographic examination displayed a significant right ventricle dysfunction, whereas compression venous ultrasonography showed no signs of a recurrent DVT. MDCT revealed bilateral central pulmonary embolism detectable on both sides and signs of right ventricle overload. Due to his clinical condition, ultrasound -assisted catheter-directed thrombolysis was initiated.
USAT Procedure and Short-Term Follow-Up
In all cases, we used EkoSonic endovascular system (EKOS Corporation, Bothell (WA), USA).
USAT was performed as described by Kucher et al. [4] with the following modifications: We used only one drug delivery catheter for each patient even in bilateral PE. In these cases, catheters with long treatment zones (18 cm) were placed at the bifurcation of the pulmonary emboli to allow efficient drug delivery into both main pulmonary arteries. For patient #4 with only rightsided central involvement, a shorter catheter (12 cm treatment zone) was used.
As thrombolytic agent, recombinant tissue plasminogen activator (rtPA) was used. In our case series we used 20mg of rtPA for bilateral PE in patients ≤ 75 years (patient # 3 and 5) and 15 mg rtPA for bilateral PE in patients >75 years (patient # 1 and 2), respectively. For patient #4 with only right-sided central PE, 10 mg rtPA was used. After a mean time of 16 hours (range 14-20 hours) the catheter was removed, the infusion of rtPA was stopped and the drug delivery catheter was removed.
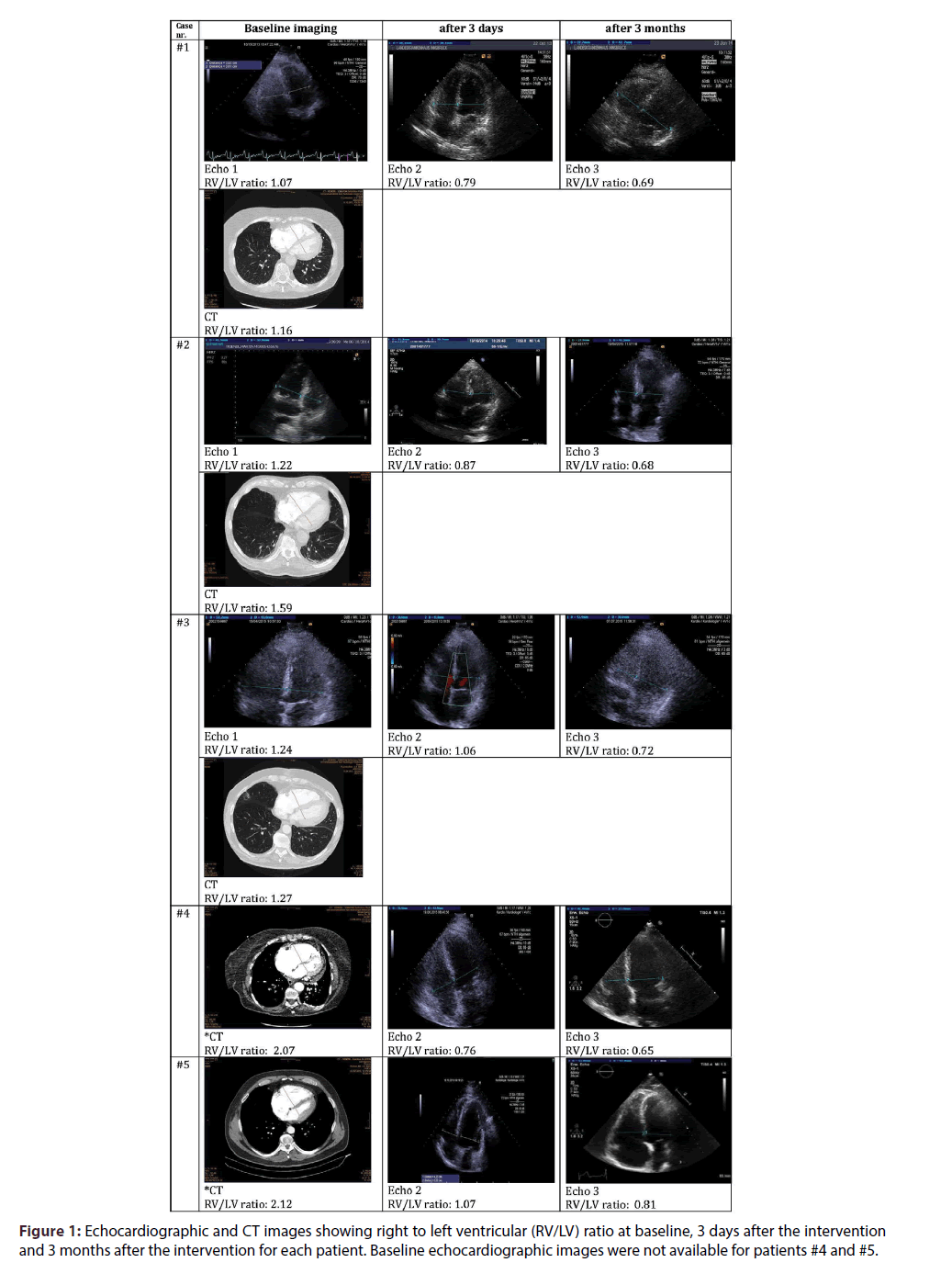
USAT was tolerated well by all patients with rapid and marked improvement of objective (heart rate, oxygen demand) and subjective (dyspnea) parameters. Only in patient #1, a GUSTO moderate bleeding episode (groin hematoma requiring the transfusion of two units of packed red cells) and a transient rise in creatinine (treated conservatively with infusions of physiological saline) were observed. Subsequently this patient and all other patients recovered well and after a mean time of 2.4 days (range 1-4 days), the patients were transferred back to the general ward. Follow-up echocardiographic examinations were performed in all patients after three days showing rapid improvement of right heart function with almost complete normalization of echocardiographically measured RV/ LV ratio (0.87 (range 0.76-1.07), corresponding to a statistically significant decrease of RV/LV ratio of 27% compared to baseline, p=0.033 (Figure 1).
Post-Procedural Anticoagulation and Long-Term Follow-Up
After a mean time of 2.4 days (range 2-4 days) unfractionated heparin was stopped and treatment with rivaroxaban (15 mg twice daily for the first 3 weeks) was initiated. All patients recovered well and were discharged subsequently after a mean hospital stay of 10.2 days (range 8–12 days). After 3 weeks the dose of rivaroxaban was changed to 20 mg once daily. Three months after USAT, patients were seen again at our outpatient clinic and follow-up-examination was performed. Echocardiography at three months showed further significant improvement with normalization of right heart function (RV/LV ratio 0.69 (range 0.65-0.81) in all patients (40% decrease compared to baseline, p=0.012). All patients reported marked improvement in terms of physical capacity. No recurrent thromboembolic events or additional bleeding episodes were reported. To prevent venous-thromboembolism (VTE) recurrence, continuation of anticoagulation treatment was recommended for all patients.
Discussion
The optimal management of intermediate-high risk PE is presently unclear [1,2,6]. USAT represents a promising new therapy for this entity [4,5,7,8].
Here we report the successful application of USAT in a case series of 5 patients with intermediate high-risk PE. After about two days, initial heparin therapy was terminated and oral anticoagulation with rivaroxaban was initiated. To the best of our knowledge, rivaroxaban treatment immediately following USAT has not been described before.
According to the PEITHO trial, systemic thrombolysis may be associated with a higher risk of bleeding complications in patients over 75 years compared to younger patients [3]. Especially older patients could therefore benefit from USAT compared to systemic thrombolysis, since this method requires only 10 - 20% of the usual dose of the thrombolytic compounds [9,10].
Right ventricular (RV) to left ventricular (LV) ratio is a valuable indicator for right ventricular dysfunction [11]. RV/LV-ratio measurement is comparable in CT and echocardiographic imaging, however CT tends to overestimate this parameter [12,13]. This could also explain the differences between CT and echocardiography- calculated RV/LV ratio in our data (Figure 1), but nevertheless both methods showed right ventricular dysfunction in our case series.
In the large VTE studies with NOAC, patients receiving thrombolytic drugs for the index event were excluded [14]. Therefore, the use of NOAC like rivaroxaban is currently not recommended for patients with PE receiving thrombolytic therapy. In contrast to vitamin K antagonists, NOAC therapy has the advantage of a constant, predictable anticoagulation without frequent dose adaptation and variation in anticoagulant efficacy [15,16]. Therefore, therapy with NOAC may be even more effective than standard anticoagulation.
However, we would strongly advice to initiate NOAC therapy only after stabilization of the patient, control of eventual bleeding complications and restoration of renal function in the case of transient renal failure.
Our case series has several limitations. First, the number of patients is too small to perform decent statistical analyses for the safety data of rivaraoxaban after USAT. Second, the case series could be affected by selection bias due to the non-randomized exploratory study design.
With the initiation of rivaroxaban therapy shortly after USAT, we observed a favourable outcome during hospitalization as well as during the followup of three months, although there was a GUSTO moderate bleeding episode in one patient. With these considerations, post-procedural anticoagulation with rivaroxaban after USAT appears to be an effective and safe treatment of intermediate-high risk PE. Further appropriate trials are needed to confirm these findings before a wider use of this strategy can be recommended.
Conflict of Interests
W.M. Franz reports personal fees and non-financial support from Bayer. P. Marschang reports personal fees and non-financial support from Bayer, personal fees and non-financial support from Boehringer Ingelheim, personal fees from Bristol-Myers-Squibb, personal fees and non-financial support from Daiichi-Sankyo, personal fees from Pfizer, and personal fees and non-financial support from Sanofi-Aventis. The other authors state, that they have no conflict of interest.
Executive summary
Background: The optimal treatment for intermediate-high risk pulmonary embolism (PE) is still unclear and challenging. A new method for this entity is ultrasound-assisted catheter directed thrombolysis (USAT). The use of non-vitamin K antagonist anticoagulants (NOAC) is currently not recommended after thrombolysis. In our case series we tried to evaluate the efficacy and safety of NOAC treatment shortly after USAT.
Methods and findings: We report five patients with intermediate-high risk pulmonary embolism who were successfully treated with rivaroxaban as post-procedural anticoagulation after USAT. The treatment was tolerated well with rapid clinical improvement and almost complete normalisation of right heart function (reduction of mean right to left ventricular (RV/LV) ratio from 1.22 (range 1.07-1.24) at baseline to 0.87 (range 0.76-1.07) three days after thrombolysis (p = 0.033). We observed one GUSTO moderate bleeding episode and a transient rise in creatinine in one patient, but no other adverse events. After 2.4 days (range 2-4 days), patients were switched from unfractionated heparin to rivaroxaban. Follow up-visit after three months showed normalisation of right heart function (RV/LV ratio 0.69 (range 0.65-0.81), no recurrent thrombotic events and no additional bleeding episodes.
Conclusion: In our experience, USAT followed by post-procedural anticoagulation with rivaroxaban appears to be an effective treatment of intermediate-high risk pulmonary embolism.
References
- Konstantinides S, Torbicki A, Agnelli G, et al. 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) * Endorsed by the European Respiratory Society (ERS). Eur. Heart. J. 35, 3033-3069 (2014).
- Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur. Heart. J. 29, 2276-2315 (2008).
- Meyer G, Vicaut E, Danays T, et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N. Engl. J. Med. 370, 1402–1411 (2014).
- Kucher N, Boekstegers P, Müller OJ, et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation.129:479–486 (2014).
- Piazza G, Hohlfelder B, Jaff MR, et al. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism. JACC. Cardiovasc. Interv. 8, 1382–1392 (2015).
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic Therapy for VTE Disease. Chest. 149, 315–352 (2016).
- Engelberger RP, Moschovitis A, Fahrni J, et al. Fixed low-dose ultrasound-assisted catheter-directed thrombolysis for intermediate and high-risk pulmonary embolism. Eur. Heart. J. 36, 597–604 (2015).
- McCabe JM, Huang P-H, Riedl L, Eisenhauer AC, Sobieszczyk P. Usefulness and Safety of Ultrasound-Assisted Catheter-Directed Thrombolysis for Submassive Pulmonary Emboli. Am. J. Cardiol. 115, 821–824 (2015).
- Braaten JV, Goss RA, Francis CW. Ultrasound reversibly disaggregates fibrin fibers. Thromb. Haemost. 78, 1063–1068 (1997).
- Parikh S, Motarjeme A, McNamara T, et al. Ultrasound-accelerated Thrombolysis for the Treatment of Deep Vein Thrombosis: Initial Clinical Experience. J. Vasc. Interv. Radiol. 19, 521–528 (2008).
- Konstantinides S. Pulmonary embolism: impact of right ventricular dysfunction. Curr. Opin. Cardiol. 20, 496–501 (2005).
- Mansencal N, Joseph T, Vieillard-Baron A, et al. Diagnosis of right ventricular dysfunction in acute pulmonary embolism using helical computed tomography. Am. J. Cardiol. 95, 1260–1263 (2005).
- Park JR, Chang SA, Jang SY, et al. Evaluation of right ventricular dysfunction and prediction of clinical outcomes in acute pulmonary embolism by chest computed tomography: comparisons with echocardiography. Int. J. Cardiovasc. Imaging. 28, 979–987 (2012).
- Büller HR, Prins MH, Lensin AWA, et al. Oral Rivaroxaban for the Treatment of Symptomatic Pulmonary Embolism. N. Engl. J. Med. 366, 1287–1297 (2012).
- Fontana P, Goldhaber SZ, Bounameaux H. Direct oral anticoagulants in the treatment and long-term prevention of venous thrombo-embolism. Eur. Heart. J. 35, 1836–1843 (2014).
- van Es N, Coppens M, Schulman S, Middeldorp S, Buller HR. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood. 124, 1968–1975 (2014).