Case Report - Interventional Cardiology (2015) Volume 7, Issue 1
Aortocoronary dissection: long-term follow up of a case managed with ostial stent
- Corresponding Author:
- Joseph Franco
Suffolk Heart Group, 260 Middle Country Road
Smithtown, NY 11787, USA
E-mail: josephjfranco@hotmail.com
Abstract
Aortocoronary dissection is one of the most dramatic complications of coronary angiography or intervention. This term has been used to describe dissecti n the aorta that is the result of coronary artery dissection which propagates retr grade to involve the ascending aorta. We present a case of significant aortocoronary dissecti n and its management with 5-year clinical and radiographic follow up. Preventi n and management of this dreaded complication will be summarized.
Keywords
Angiography, complications, covered stents, dissection, ostial stenting, retrograde
Aortocoronary dissection is a term that refers to the untoward complication of coronary angiography or percutaneous intervention in which a coronary dissection propagates retrograde into the ascending aorta. The reported incidence is 0.02% [1]. Several risk factors for the development of aortocoronary dissection have been identified; however, a definitive approach to management is lacking.
Published reports on this opic exist [2–5]. Owing to the rare and deadly na re of his complication, a prospective st dy is nlikely to take place. However, mo nting experi-ence from different centers with cases span-ning the entire spectrum of dissection sever-ity may provide management insight to the interventional cardiologist that is faced with this critical complication.
We present a case of significant aortocoro-nary dissection, managed with a covered stent to the coronary ostium, with 5-year follow up and in vivo examination of the aorta proving complete healing.
Case
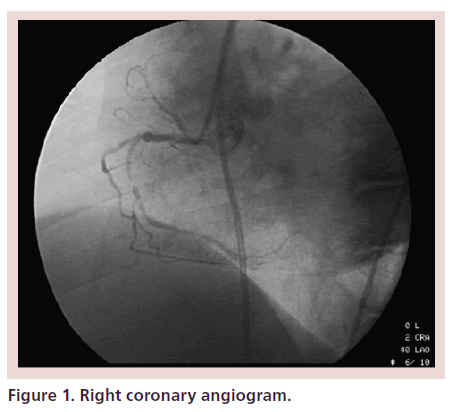
A 67-year-old woman with a history of hypertension and diabetes underwent elective coronary angiography for persistent class III angina and a positive stress test with a large inferior wall perfusion abnormality. Coronary dominance was right. There was eccentric 60% stenosis of the proximal right coronary artery (RCA) and a discrete 95% stenosis of the mid-RCA. The distal vessel had moderate atherosclerotic disease. Representative images of the coronary angiogram are pictured in Figure 1.
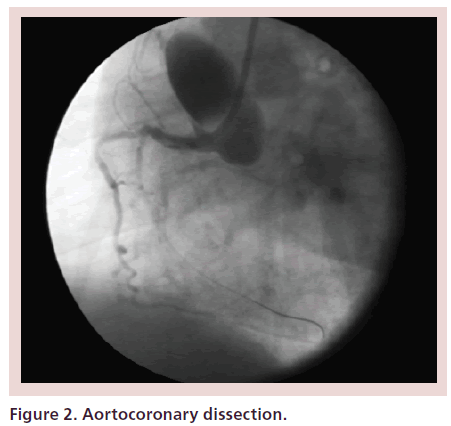
The initial intention was to treat the 95% mid-RCA lesion with the goal of relief of angina. Through a 6F JR4 guide catheter, the mid RCA was dilated with a Quantum balloon (2.5 × 8 mm, Boston Scientific, Natick, MA, USA). A drug-eluting stent (2.5 × 8 mm Express, Boston Scientific, Natick, MA, USA) was unable to cross the lesion. In an attempt to provide the support necessary to cross the lesion with the stent, the guide catheter became deeply seated in the RCA. This resulted in dissection of the proximal RCA which propagated retrograde into the aortic root and ascending aorta creating an extensive Type-A dissection (Debakey type II) extending just proximal to the origin of the innominate artery. A dissection of the mid RCA at the site of balloon angioplasty was also noted with distal extension and staining (Figure 2).
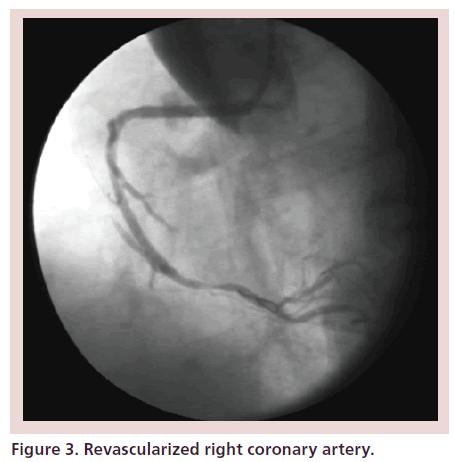
Consultation with a cardiothoracic surgeon was immediately obtained. The patient had stable vital signs and no chest pain. There was no evidence of pericardial effusion on emergent echocardiogram. The decision was made to attempt to seal the proximal RCA dissection with the aim of halting the progression of the aortic dis-section. A covered stent (19 mm JOSTENT, Abbott Vascular, IL,USA) was mounted on a Monorail balloon (3 × 20 mm NC Quantum Apex, Boston Scientific, MA, USA) and deployed in the proximal RCA. There was persistence of the dissection proximally and therefore a second 19 mm JOSTENT was deployed using a similar technique, overlapping the first JOSTENT and extending through the ostium of the RCA into the aortic root. No further contrast extravasation was noted, and the patient remained hemodynamically stable and free of chest pain. Next, a drug-eluting stent (2.5 × 23 mm BX Velocity, Cor-dis, Miami Lakes, FL, USA) was used to seal the mid to distal RCA dissec ion. Revascularized RCA is pictured in Figure 3.
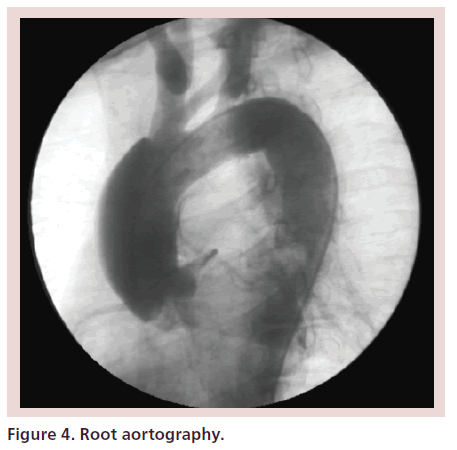
Root aortography revealed a Type-A dissection extending to, but not involving, the origin of the innominate artery, with no evidence of aortic regurgitation (Figure 4).
The patient was transferred to the cardiac intensive care unit in stable condition. A computed tomography of the chest was performed the following day and showed no evidence of dissection. She was discharged from the hospital on post-procedure day six. Follow up contrast CT scans 3 months and 1 year later also did not demonstrate aortic dissection.
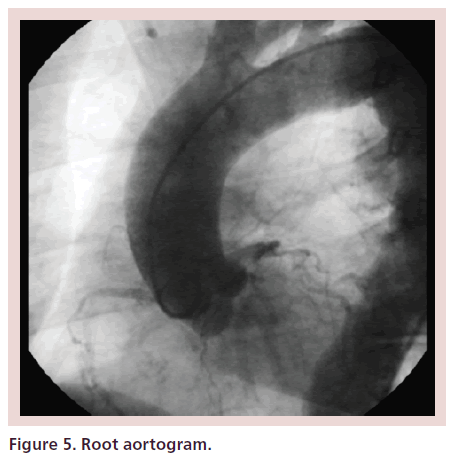
Five years later, the patient was admitted to the hospital with chest pain and positive cardiac biomarkers. She underwent diagnostic coronary angiography and root aortography which revealed multivessel CAD. Aortic dissection was not present (Figure 5).
An elective coronary artery bypass grafting sur-gery was performed. Intra peratively, the aorta was described as appearing normal and the grafts were successfully implanted on it. She was discharged on post-op day 13.
Discussion
Dissection of a coronary artery during cardiac catheterization is a well-recognized procedural complication. In most cases, the dissection travels distally from the entry point and leads to occlusion of the involved coronary. Rarely, the dissection may travel retrograde to the coronary cusp and sometimes into the ascending aorta [6]. The in-hospital mortality rate of Type-A aortic dissection that is managed without surgery is approximately 60% [7]. Therefore, every effort should be made to avoid this complication and to treat it before a negative outcome occurs.
The interventionalist should be aware of the risk factors for this complication. In a review of published case reports, the most common scenario is dissection that occurs in attempts to engage the RCA [8]. The right coronary cusp is smaller than the left coronary cusp and the angle at which the artery stems from the aorta is almost 90º, whereas the left main typically branches at an acute angle [9]. In addition, variant anatomy of the coronary ostia is a well-known risk factor for dissection [10]. Retrograde approach to chronic total occlusions has been associated, rarely, with aortocoronary dissections [11].
The use of rigid wires and catheters, noncompliant balloons or other devices, as well as catheterization during acute myocardial infarction are known predisposing factors [10]. In a more recent review of the literature, the most common cause of dissection was guide-catheter-induced trauma (63%) followed by guidewire-induced trauma (11.6%), forceful balloon inflation (14.7%), forceful contrast injection (7.4%) and forceful manipulation of a stent (1.1%) [12]. In addition to avoiding the previous predisposing factors, meticulous attention to the pressure waveform and avoiding contrast injection if it is dampened, is crucial. Moreover, guide catheters with side holes should be avoided as they may provide a false sense of security but can lead to dissection upon contrast injection [12].
Once aortocoronary dissection has been identified, contrast injection should stop, as it may worsen the dissection, and the following three management options need to be considered first:
• Clinical observation: Admission to the cardiac intensive care unit with repeated aortic imaging (TEE, computed tomography, etc). Frequent clinical and hemodynamic assessment is the mainstay of this option;
• Stenting of the coronary dissection: An attempt to occlude further blood flow through the coronary artery dissection into the ascending aorta with a stent at the coronary ostia may prevent aortic hematoma growth [8]. Direct stenting of the coronary dissection should also be performed [2], although ostial stenting should take precedence, as any delay can worsen prognosis or lead to progressive aortic dissection [8]. In our case, stenting the entry site first did not halt the retrograde dissection and only after the second stent, which extended across the ostium, was deployed that good control over the retrograde flow was obtained. The type of stent used should be operator and case specific. Some of the previous reports used covered stents, but other used noncovered ones [12];
• Immediate open surgical intervention [13].
Dunning et al. have previously proposed a severity grading system that can help to triage patients to one of the above management options [14]. If less than 40 mm of the ascending aorta is involved in the dissection, then nonsurgical approaches might be considered, whereas immediate surgery is advocated for dissections greater than 40 mm.
More recent reports, however, have documented excellent outcomes in stable patients with ostial stenting. When the dissection could be sealed under direct visualization, the results were usually satisfactory and the patients were spared surgery, even in cases of larger dissections [8].
It stands to reason that there may be bias when only successful cases are reported [15]. However, there is little doubt that repeated success justifies this approach in the appropriate scenario. It is important to note that this methodology does not preclude surgical intervention in case of clinical deterioration (e.g., expansion of the dissection, pericardial hemorrhage, hemodynamic instability, failure of percutaneous intervention, etc.) [8].
In our patient’s case, a decision to stent the RCA ostium was made, given her clinical stability and the presence of a backup surgical team. The outcome was excellent and this was confirmed 5 years later with in vivo examination of the aorta during elective bypass surgery. To our knowledge, this is the first report of 5-year follow up of aortocoronary dissection with the benefit of direct visualization of the ascending aorta, and confirming the complete healing to the point where grafts were successfully implanted.
In conclusion, we believe that in cases of known or suspected aortocoronary dissection, an immediate consultation with a cardiothoracic surgeon is mandatory. However, in the absence of hemodynamic instability an attempt at ostial stenting with the intent to prevent further propagation of the dissection is warranted and may prevent future morbidity and mortality.
Conclusion & future perspective
Significant experience now exists to justify an initial percutaneous approach to aortocoranry dissections in the appropriate setting. As we get more aggressive in approaching anatomically challenging coronary lesions, we need to remain wary of the rare, but deadly, complications of coronary angiograms and interventions. Luckily, the hardware will continue to improve, and along with adopting active prevention techniques, this will lead to aortocoronary dissection remaining a rare and a manageable complication.
Financial and competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
• Aortocoronary dissection is a lethal complication of coronary angiography and intervention.
• As with any complication, the best strategy is to avoid its occurrence.
• Carefully choosing the hardware and avoiding contrast injection when the pressure waveform is blunted are two essential steps in prevention.
• Once identified, contrast injection should stop until a management strategy is adopted.
• Coronary ostial stenting, followed by dissection site stenting, can stop the dissection and, as in our case, lead to complete healing of the aorta.
• Close monitoring and follow up regardless of the initial management are indicated.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- Vega MR. ortic dissection: exceedingly rare complication of coronary angioplasty. Cathet. Cardiovasc. Diagn. 42(4), 416 (1997).
- Yip HK, Wu CJ, Yeh KH et al. Unusual complication of retrograde dissection to the coronary sinus of valsalva during percutaneous revascularization: a single-center experience and literature review. Chest 119(2), 493–501 (2001).
- Seifein HB, Missari JC, Warner MF. Coronary stenting for aortocoronary dissection following balloon angioplasty. Cathet. Cardiovasc. Diagn. 38(2), 222–225 (1996).
- Perez-Castellano N, Garcia-Fernandez MA, Garcia EJ, Delcan JA. Dissection of the aortic sinus of Valsalva complicating coronary catheterization: cause, mechanism, evolution and management. Cathet. Cardiovasc. Diagn. 43(3), 273–279 (1998).
- Bapat VN, Venn GE. A rare case of aortocoronary dissection following percutaneous transluminal coronary angioplasty: successful treatment using offpump coronary artery bypasses grafting. Eur. J. Cardiothorac. Surg. 24(2), 312–314 (2003).
- Wyman RM, Safin RD, Portway V, Skillman JJ, McKay RG, Baim DS. Current complications of diagnostic and therapeutic cardiac catheterization. J. Am. Coll. Cardiol. 12(6), 1400–1406 (1988).
- Hagan PG. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 283(7), 897–903 (2000).
- Carstensen S, Ward MR. Iatrogenic aortocoronary dissection: the case for immediate aortoostial stenting. Heart Lung Circ. 17(4), 325–329 (2008).
- Lopez-Minguez JR, Climent V, Yen-Ho S, Gonzalez-Fernandez R, Nogales-Asensio JM, Sanchez-Quintana D. Structural features of sinus of valsalva and the proximal portion of the dissection. Rev. Esp. Cardiol. 59(7), 696–702 (2006).
- Boyle AJ, Chan M, Dib J et al. Catheter-induced coronary artery dissection: risk factors, prevention and management. J. Invasive Cardiol. 18(10), 500–503 (2006).
- El Sabbagh A, Patel VG, Jeroudi OM et al. Angiographic success and procedural complications in patients undergoing retrograde percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 3,482 patients from 26 studies. Int. J. Cardiol. 174(2), 243–248 (2014).
- Shorrock D, Michael TT, Patel V et al. Frequency and outcomes of aortocoronary dissection during percutaneous coronary intervention of chronic total occlusions: a case series and systematic review of the literature. Cathet. Cardiovasc. Interv. 84(4), 670–675 (2014).
- Darwazah AK, Aloul J, Abu Sham’a RA, Eida M, Ismail H. Iatrogenic right coronary artery dissection with retrograde extension to the right coronary sinus. J. Card. Surg. 23(2), 177–179 (2008).
- Dunning DW, Kahn JK, Hawkins ET, O’Neil WW. Iatrogenic coronary dissections extending into and involving the aortic root. Cathet. Cardiovasc. Intervent. 51(4), 387–393 (2000).
- Hunt I, Faircloth ME, Sinha P, Marber MS, Venn GE, Young CP. Aortocoronary dissection complicating angioplasty of chronically occluded right coronary arteries: is conservative approach the right approach? J. Thorac. Cardiovasc. Surg. 131(1), 230–231 (2006).
• Excellent argument for ostial stenting.
•• Excellent recent review of the published cases with emphasis on chronic total occlusions.