Short Communication - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 3
Are subdeltoid bursitis and polymyalgia rheumatica preferances of COVID-19 vaccine?
- *Corresponding Author:
- Alexander Rozin P
B. Shine Rheumatology Institute, Rambam Health Care Campus and Technion, Haifa, Israel
E-mail: a_rozin@rambam.health.gov.il
Abstract
COVID-19 vaccine became clear card life-saving medication. Due to over world vaccination a rate of prevalence and incidence of coronal infection is going to back down. However, we meet different side effects of the vaccine. Two cases of subdeltoid bursitis after COVID-19 vaccination discussed.
Keywords
COVID-19 vaccine • subdeltoid bursitis • polymyalgia rheumatica • corticosteroid therapy
Introduction
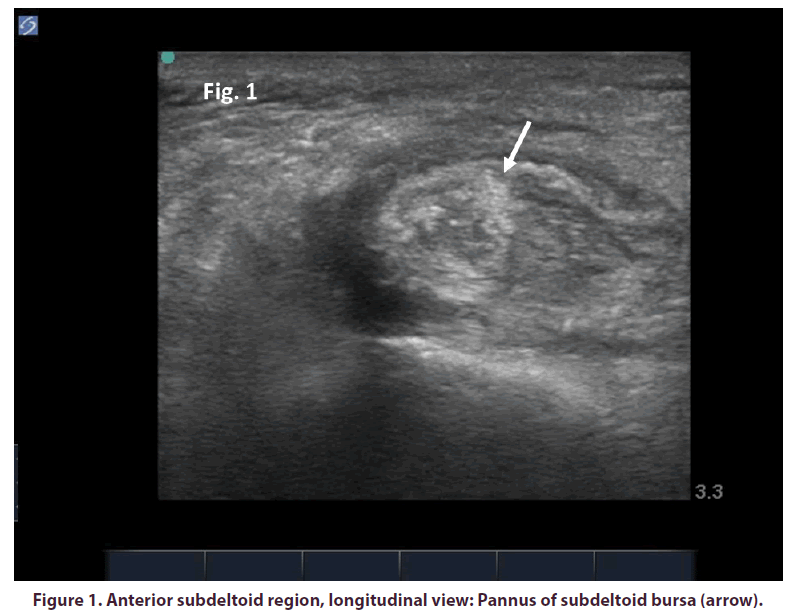
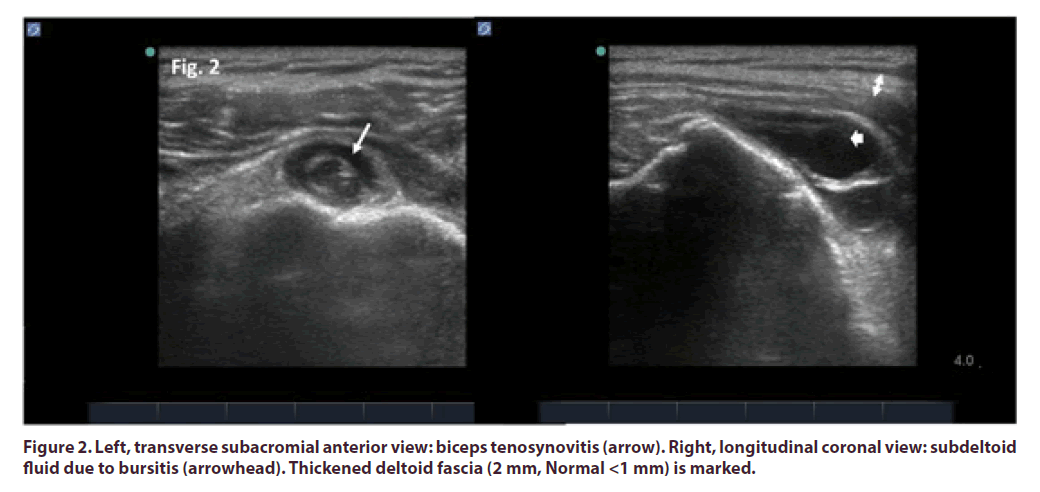
COVID-19 vaccine became clear card lifesaving medication [1]. Due to over world vaccination a rate of prevalence and incidence of coronal infection is going to back down. However, we meet different side effects of the vaccine [2,3]. It is not surprise. The vaccine has properties to induce immune reactions and protective antibody producion is only a part of them. Here there is first illustration. Medical sister 59 years old got second vaccine and 4 days later felt severe shoulder pain, swelling and limitation of motion. After first vaccination, there was only minor shoulder pain of the same side. Focus of injection (lateral shoulder) was not tender or red but a forward part of humeral head became swollen and painful. US showed pannus of subdeltoid bursa (Figure 1). Intrabursal injection with bethamethasone 6 mg followed by gradual pain, swelling and stiffness resolution during one week. Second history was graduate development of severe bilateral shoulder pain and stiffness in patients 83 years old for 3 weeks after second COVID-19 vaccination. Both injections performed on the same side. Severe subacromial tenderness, swelling and limitation observed. US showed bilateral tenosynovitis, subdeltoid bursitis and deltoid fasciitis (Figure 2) associated with polymyalgia rheumatica. C-reactive protein was elevated 35 times of normal. Methylprednisolone intravenous infusion of daily dose 25 mg followed by prednisone 20 mg/day alleviated complaints by 70% during next 3 days.
COVID-19 vaccine has high immunogenicity. As result of poor antigen presentation or failed antibody response S-protein may expansively spread causing tissue damage and hypersensitiviy reactions. Once upon ago an alternative mechanism of molecular mimicry was proposed [4]. Due to similarity of foreign antigen and host tissues, a process of neutralization of the antigen may be defected. This brings about its uncontrolled expansion and long standing autoimmune disease
References
- Polack SFP, Thomas SJ, Kitchin N et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine.N. Engl. J. Med. 383, 2603–2615 (2020).
- Zhang Y, Zeng G, Pan H et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults. Lancet. Infect. Dis. 21(2), 181–192 (2021).
- Rozin AP, Yalonetsky S. Images of COVID-19 Vaccination. Int. J. Case. Rep. Clin. Image. 3(1), 144(2021).
- Rozin AP. From molecular mimicry to cross-reactivity or pathogen expansion? A hypothesis. Clin. Rheumatol. 26, 285–288 (2007).