Brief Report - Imaging in Medicine (2016) Volume 8, Issue 3
Arteriovenous fistula between descending aorta: and left inferior pulmonary vein
- *Corresponding Author:
- Mustafa Kösecik
Division of Pediatric Cardiology
Sakarya University School of Medicine,Sakarya-Turkey
Tel.: +90 414 318 3000
E-mail: mustafakosecik@yahoo.com
Abstract
Congenital systemic arteriovenous fistula arising from aorta and draining through the pulmonary vein to left atrium without lung sequestration is a rare vascular malformation [1,2]. On physical examination there is usually a continuous or systolic murmur. Clinical presentation depends upon the size and place of the vascular malformation [3]. If there is a suspicion of arteriovenous fistula on physical examination and echocardiography, multislice computed tomography angiography (CTA) can be helpful in confirming diagnosis and anatomic model, and choosing appropriate treatment modality [3,4].
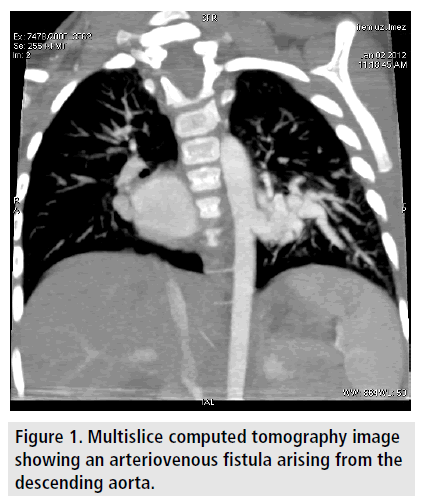
We describe a rare case with arteriovenous fistula between thoracic aorta and left inferior pulmonary vein occluded with Amplatzer vascular plugs. A 20 month old girl with failure to thrive and cardiac murmur was referred by a pediatrician with suspected congenital heart diseases for an echocardiography. Her weight and height were 9 kg (<3% percentile) and 78 cm (10-25% percentile). Physical examination confirmed the presence of Grade III/VI systolic murmur heard on apical region and radiated to the mid scapular region posteriorly. There were a hyper dynamic pulse at the rate of 110/ min, forceful left ventricular apex impulse and mild hepatomegaly. There was no cyanosis or clubbing. Chest radiography showed mild cardiomegaly (cardio thoracic ratio 0.54) with increased pulmonary vascular markings especially in the lower left pulmonary region. The patient has mild congestive heart failure clinically. Echocardiography revealed left atrial and ventricular enlargement, moderately mitral valve regurgitation and increased blood flow into left atrium from enlarged left inferior pulmonary vein. An abnormal vessel that demonstrated a communication with the left inferior pulmonary vein was noted nearly to the left atrium. Diagnosis of the patient may be arteriovenous malformation/fistula but was not clear. Hence multislice CTA was done which revealed an abnormal communication, arteriovenous fistula, originating from thoracic aorta and draining into left inferior pulmonary vein (FIGURE 1 & VIDEO 1). The fistula drained through the left inferior pulmonary vein to the left atrium leading to left-to-left shunt. Lung had normal bronchial connection and pulmonary vasculature.
Figure 1. Multislice computed tomography image showing an arteriovenous fistula arising from the descending aorta.
Video 1. An abnormal communication originating from thoracic aorta and draining into left inferior pulmonary vein on multislice CT angiography.
Video 2.An arteriovenous fistula originating from thoracic aorta and draining to left inferior pulmonary ve
Video 3. A complete fistula occlusion on angiography after the second procedure.
Thoracic aortogram revealed an arteriovenous fistula originating from thoracic aorta and draining to left inferior pulmonary vein, and finally into left atrium (VIDEO 2). That was closed with embolization of Amplatzer vascular plugs. Post procedure thoracic aortogram showed a complete occlusion (VIDEO 3).
Congenital arteriovenous fistula arising from thoracic aorta and draining into left inferior pulmonary vein without lung sequestration is an extremely rare malformation [1,5,6]. To the best of our knowledge, we reported the first case with a significant left-to-left shunt due to fistulous communication between the thoracic aorta and left inferior pulmonary vein, that percutaneous occlusion performed.
If there is a clinical and echocardiographic suspected arteriovenous fistula, multislice CTA is an appropriate imaging method to confirm diagnosis and choose therapy modality [4,6]. Also cardiac catheterization and angiography is necessary for both diagnosis and intervention procedures [3].
References
- Shebani SO, Khan MD, Tofeig MA. A congenital fistula between the descending aorta and the right pulmonary vein in a neonate presenting with heart failure. Cardiol. Young. 17, 563-564 (2007).
- Kosutic J, Minic P, Sovtic A et al. Upper lung lobe systemic artery-pulmonary vein fistula with signs and symptoms of congestive heart failure: Successful treatment with coil embolization. J.Vasc.Interv.Radiol. 18, 299-302 (2007).
- Keane JF, Fyler DC. Vascular Fistulae. In: Keane JF, Lock JE and Fyler DC. Nadas’ Pediatric Cardiology. 2nd edn,Philadelphia, 799-804 (2006).
- Moral S, Ortuño P, Aboal J. Multislice CT in congenital heart disease: Partialanomalous pulmonary venous connection. Pediatr.Cardiol. 29, 1120-1121 (2008).
- Currarino G, Katheryn W. Congenital fistula between an aberrant systemic artery and a pulmonary vein without sequestration: A report of three cases. J.Pediatr.87, 554-557 (1975).
- Jariwala P, Ramesh G, Sarat Chandra K. Congenital anomalous/aberrant systemic artery to pulmonary venous fistula: Closure with vascular plugs & coil embolization. Indian. Heart. J. 66, 95-103 (2014).