Mini Review - Interventional Cardiology (2023) Volume 15, Issue 4
Bail-out stenting: An overcoming problem in drug coating balloon percutaneous coronary intervention era
- Corresponding Author:
- Gabriele Ghetti
Department of Cardiology, IRCCS University Hospital of Bologna Policlinico S. Orsola-Malpighi, Bologna, Italy,
E-mail: gabriele.ghetti84@gmail.com
Received date: 03-Jul-2023, Manuscript No. FMIC-23-104468; Editor assigned: 05-Jul-2023, PreQC No. FMIC-23-104468 (PQ); Reviewed date: 19-Jul-2023, QC No. FMIC-23-104468; Revised date: 26-Jul-2023, Manuscript No. FMIC-23-104468 (R); Published date: 03-Aug-2023, DOI: 10.37532/1755-5310.2023. 15 (4).737
Keywords
Drug coated balloon • Bail-out stent • De novo coronary stenosis • Small vessels percutaneous coronary intervention • Optical coherence tomography • Fractional low reserve
Introduction
In the last two decades Drug Coated Balloons (DCB) Percutaneous Coronary Angioplasty (PCI) have been exponentially applied to more patients and various settings with satisfying results. The idea of “leaving nothing behind” after a percutaneous coronary angioplasty is fascinating due to restoring native vasomotricity and to reduce late and very late stent thrombosis and stent restenosis in absence of permanent metallic device without the elevated thrombotic risk seen with bioresorbable scaffolds [1-3].
Recent improvements in device features, procedural techniques and operators’ skills have limited acute complications such as recoil and high-grade dissections requiring a Bail-Out Stent (BOS) strategy, which remains the main issue related to DCB angioplasty.
Literature Review
What is a drug coated balloon?
DCBs are semi-compliant balloons coated with an ant proliferative drug and a matrix in order to reduce the drug loss into the blood flow and facilitate the drug delivery into vessel wall without permanent or semi-permanent scaffold implantation [4]. The DCB efficacy relies on the interplay between balloon designs, matrix formulations, drug, and its dose and release kinetics. The available DCBs differ in terms of the above characteristics so that a “class effect” may not be assumed [5].
The most used drugs are Paclitaxel and Sirolimus. Paclitaxel is an antimitotic agent that acts promoting the assembly of microtubules from tubulin dimers and stabilizes microtubules by preventing depolymerization, so it inhibits neointima formation. Furthermore, it is a lipophilic substance that needs a short contact-time to pass in a significate concentration into the vessel wall and lasting for several weeks [6]. However, some studies have suggested that Paclitaxel may have a small therapeutic window since high deses have been associated with higher mortality in patients undergoing lower limb revascularization with Paclitaxel DCB than those treated with Plain Old Balloon (POBA) [7]. Although these data have not been confirmed in subsequent studies and in coronary setting [8]. This theoretically drawback along with the fact that Paclitaxel drug eluting stent has resulted in worse clinical outcome as compared to current-limus drug eluting stents have prompted to develop new DCBs with the most studied one being the Sirolimus DCB.
When drug coated balloon can be used?
Primarily, DCB PCI demonstrated the same efficacy of Drug Eluting Stent (DES) in In-Stent Restenosis (ISR) [9]. In the last years, de novo small vessels DCB PCI resulted non inferior to DES at one-year and superior to DES at long follow-up in terms of Major Adverse Cardiac Events (MACE) [10-14]. These results could be related to the late lumen gain due to anti proliferative drug effect without the permanent inflammatory stimulus of a metallic platform [15]. Differently, DCB use in bifurcation treatment and in large vessels is still debated [16-18]. Promising evidences have been reported also in ST-Elevation Myocardial Infarction (STEMI) setting [19,20] and in high bleeding risk patient [21].
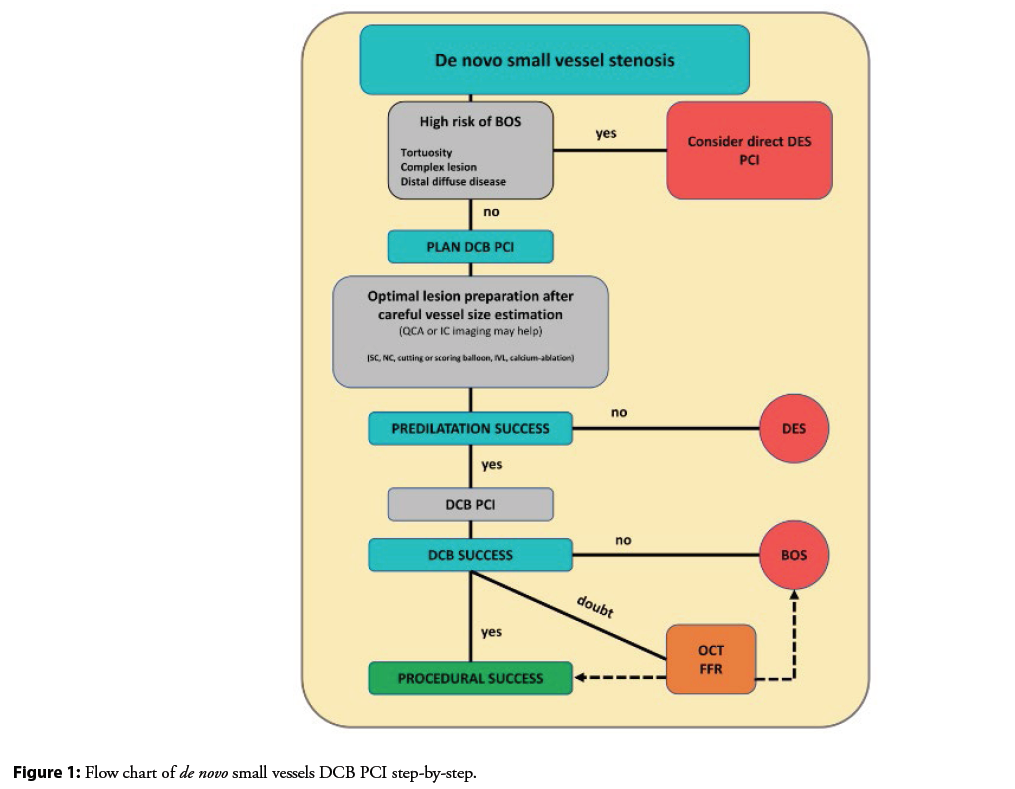
Drug coated balloon percutaneous coronary intervention step-by-step
The DCB is a device intended to delivery drug therapy into the vessel wall, not to properly do PCI. For this reason, a careful lesion preparation is recommended. There is not a predilatation tool of choice, but it should be calibrated on the kind of coronary stenosis and to the angiographic response. A balloon-to-artery ratio of 1:1 is recommended and in more complex stenosis it is reasonable to start with smaller balloons and subsequently reassess vessel size [22,23]. Any kind of predilatation tool can be used (semi-compliant, noncompliant, cutting or scoring balloon, intracoronary lithotripsy, calcium-ablator systems). The lesion preparation is to be considered successful if, at least 5 minutes after intracoronary nitro derivate administration, all the following points are met: 1) ≤ 30% residual angiographic stenosis; 2) Thrombolysis In Myocardial Infarction (TIMI) flow grade 3; the absence of a flow-limiting dissection. Then, a 0.8 or 1:1 DCB-to-artery ratio should be applied. The device should be two millimeters longer both side of the predilated lesion and inflated at nominal pressure. A single DCB must be used only for one coronary lesion. Referring to pre-stent era data, type A and B dissections are considered safe, and healing is always expected. Differently there is still debate on type C dissections [24], but at the moment the international recommendations suggest stent implantation in case of type C or worse coronary dissection. So, in case of high-grade dissections or important recoil BOS should be implanted (Figure 1).
Bail-out stent
Bail-out stent is the term used for stent placement to treat a coronary artery with iatrogenic complication (e.g. high grade dissection) or ineffective balloon angioplasty [25]. During a planned DCB PCI, the need of stent implantation can occur both after lesion preparation, and after DCB inflation. In the first case the operator should change is mind due to the presence of highgrade dissection or in case of important vessel recoil. BOS after DCB inflation is generally secondary to a worsening pre-existing coronary dissection. The risk of BOS should be bear in mind especially in case of a planned DCB PCI for de novo lesions in small vessel disease. Indeed, stent of small diameter needs long dual antiplatelet therapy and are affected by a higher risk of restenosis and thrombosis [26]. In the first small vessels randomized studies the rate of BOS was very high (more than 30%) owing to the first technology of DCB and low rate of lesion predilation [27]; but in recent trials the number of stents implanted during DCB angioplasty has been drastically reduced, although it is still not neglectable (Table 1). The need of BOS has been constantly associated with a trend in worse outcome both in the BMS and DES era [28]. In the most recent trials DCB were not inferior to DES in small vessels PCI, but despite the use of second generation DES in case of bail-out, the BOS group showed two times higher, even not statistically significant, rate of MACE (Table 2). The rates of MACE at 12 months in the BOS group were 15.8 in the BASKET SMALL 2 and 12.5% in PICCOLETO 2 trial, as compared to 7.0% and 4.9% of the only-DCB group, respectively.
| Year | Design | Pts (n) | Setting | DCB arm | DES arm | Stent before DCB protocol deviation (n, %) | BOS (n, %) | |
|---|---|---|---|---|---|---|---|---|
| PICCOLETO27 | 2010 | RCT | 57 | SVD | Dior | Taxus Libertè | nr | 10 (36) |
| BELLO28 | 2012 | RCT | 182 | SVD | IN.PACT Falcon | Taxus Libertè | nr | 19 (20) |
| Nishiyama et al.18 | 2016 | RCT | 60 | SVD | SeQuent Please | Xience | 3 (10) | 0 (0) |
| Gobic et al.20 | 2017 | RCT | 75 | STEMI | SeQuent | Biomime | nr | 3 (7) |
| BASKET SMALL 210 | 2018 | RCT | 758 | SVD | SeQuent Please | Taxus | 125 (14) | 19 (5) |
| or | ||||||||
| Xience | ||||||||
| RESTORE SVD12 | 2019 | RCT | 230 | SVD | Restore | Resolute | nr | 6 (5) |
| DEBUT21 | 2019 | RCT | 208 | HBR | SeQuent Please | Integrity | 23 (10) | 5 (5) |
| REVELATION19 | 2019 | RCT | 120 | STEMI | Pantera Lux | Orsiro | nr | 11 (18) |
| or | ||||||||
| Xience | ||||||||
| PEPCAD NSTEMI17 | 2020 | RCT | 210 | NSTEMI | SeQuent Please | BMS | nr | 18 (17) |
| or | ||||||||
| DES | ||||||||
| PICCOLETO 211 | 2020 | RCT | 232 | < 2.75 | Elutax SV/Emperor | Xience | nr | 8 (7) |
Table 1: Main clinical randomized trials comparing DCB and DES in de novo percutaneous coronary
Note: The table shows the main comparative studies between DCB and DES in de novo lesion PCI. The rate of bail-out stenting is extremely variable.
DCB: Drug Coated Balloons; DES: Drug Eluting Stents; PCI: Percutaneous Coronary Intervention; Pts: Number of Patients; SVD: Small Vessel Disease; BOS: Bail-Out Stent; RCT: Randomized Controlled Trial; STEMI: ST-Elevation Myocardial Infarction; NSTEMI: no ST-Elevation Myocardial Infarction; HBR: High Bleeding Risk.
| Year | Design | Pts (n) | BOS (n, %) | MACE DCB (%) | MACE DES (%) | MACE BOS (%) | Restenosis DCB (n, %) | Restenosis DES (n, %) | Restenosis BOS (n, %) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Piccoleto27 | 2010 | RCT | 57 | 10 (36) | nr | nr | nr | 9 (32) | 3 (10) | 3 (30) |
| BELLO28 | 2012 | RCT | 182 | 19 (20) | 10 | 16 | nr | 8 (10) | 10 (12) | 3 (16) |
| Nishiyama et al.18 | 2016 | RCT | 60 | 3 (10) | 0 | 0 | 0 | 0 (0) | 2 (6.1) | 0 (0) |
| BASKET SMALL 210 | 2018 | RCT | 758 | 19 (5.1) | 7 | 5.7 | 15.8 | nr | nr | nr |
| PICCOLETO 211 | 2020 | RCT | 232 | 8 (6.7) | 5.6 | 7.5 | 12.5 | 6.3 | 6.5 | nr |
Note: The table shows the main comparative studies between DCB and DES reporting major adverse clinical events or restenosis of BOS group at follow-up. Three of them reported the rate of restenosis and two of them the rate of MACE in DCB, DES or BOS group. BOS: bail-out stent; DCB: drug coated balloons; DES: drug eluting stents; Pts: number of patients; MACE: major adverse cardiac events; RCT: randomized controlled trial.
Table 2: Main clinical randomized trials reporting BOS adverse events at follow-up
The link between the use of BOS and the higher risk of MACE is not still clearly understood. Failure in lesion preparation could be associated with the use of longer stents that in small vessels are correlated to higher risk of failure during follow-up even with second-generation DES. Moreover, stenting a longer coronary segment is not free from the risk of bifurcation involvement making the procedure more complex.
Discussion
How to reduce bail-out stent rate
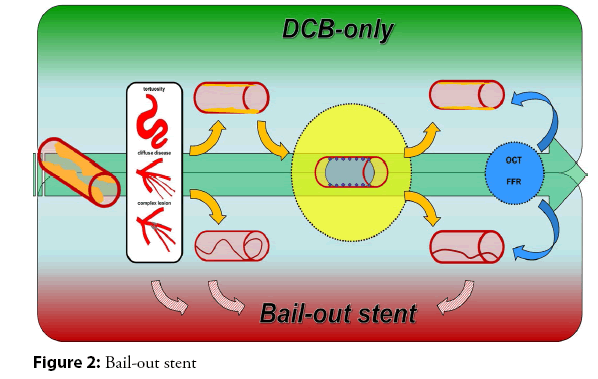
In planning and performing a DCB PCI, therefore, the need to achieve good angiographic results should be balanced with the risk of BOS. In a recent study, enrolling 168 consecutive patients treated with DCB, Ghetti, et al have demonstred that both lesion and procedural characteristics may be associated with the risk of BOS. In particular, vessel tortuosity, distal diffuse disease without a good landing zone for the device and very complex lesion-grade C according to American Heart Association/American College of Cardiology (AHA/ACC) classification-are strongly correlate to BOS [29]. Secondly, in small vessels PCI and in severe or diffuse disease, an accurate evaluation of vessel diameter is extremely important in order to avoid device oversizing (Figure 2). This is one of the operator-dependent BOS risk factors. Precisely, per each 0.1 incremental in DCB-to-artery ratio more than 1.0, there is four times higher risk of BOS. Experts’ consensuses suggest a gentle inflation with an under-dimensioned balloon or imaging assessment of vessel sizing and plaque morphology in case of visual estimation doubts. Ongoing randomized studies are applying imaging assessment, particularly Optical Coherence Tomography (OCT), to reduce the bail-out stent rate [30]. The advantages of imaging are: better sizing, identification of safe landing zones and plaque morphology assessment. Moreover, drug coated balloon inflation time should be as longer as can be tolerated. First, because longer balloon-artery contact leads to higher drug dose delivery into vessel wall. Secondly, long inflation can practice scaffoldlike effect and reduce iatrogenic dissection, like in peripheral percutaneous treatment [31].
Post-DCB assessment
International Expert Consensuses suggest angiographic visual assessment in at least two orthogonal projections to evaluate DCB PCI results. In case of absence of type C or worse dissection and no more than 30% of residual stenosis, the procedure can be considered successful. The objective of de novo DCB PCI is not a “stent-like” acute result because the complete effect of this therapy can be seen at long follow-up with delayed acute gain. On the contrary, the main goal of the procedure is not to cage coronary artery with a metallic permanent platform but return coronary vaso motricity. When angiographic result is dubitative, further invasive assessment have been proposed. OCT is the best tool to analyze anatomical coronary changes during PCI and OCT post-DCB PCI evaluations have been advocated to predict acute vessel closure. As in stent PCI, the presence of medial dissection is considered a sign of abrupt coronary closure, so BOS is required [32]. Some small studies report that post DCB-PCI intimal limited dissection as assessed by OCT is safe and linked to late lumen enlargement. On the opposite, medial dissections correlate with angiographic dissection progression after 15 minutes [33]. Recently, it has been suggested that physiological assessment-both hyperemic and not hyperemic indices-after DCB may have prognostic implications [34-36], however the optimal cut-off of functional test post-PCI it is not still clear. Finally a recent small observational study has suggested that dynamic changes of functional tests during 15 min after DCB may be associated with the risk of abrupt vessel closure due to severe dissections. However larger studies are warranted to confirm the efficacy and safety of this latter approach.
Conclusion
De novo vessels drug coated balloon percutaneous coronary angioplasty is a real attractive procedure and has shown better results compared to drug eluting stent PCI. However, bail-out stent is a relevant issue that should be bear in mind when a DCB PCI is planned. Indeed, BOS patients are affected by higher rate of 1-year MACE compared to DCB or DES only small vessels patients. Anatomical features, like vessel tortuosity, distal diffuse disease, and complex coronary stenosis are correlate to the risk of addictive stent implantation, as well as DCB oversizing. OCT and physiological assessment can be helpful to thoroughly assess the DCB PCI results.References
- Cosgrave J, Corbett SJ, Melzi G, et al. Late restenosis following sirolimus-eluting stent implantation. Am J Cardiol. 100(1):41-44 (2007).
- Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 293(17):2126-2130 (2005).
- Wykrzykowska JJ, Kraak RP, Hofma SH, et al. Bioresorbable scaffolds versus metallic stents in routine PCI. N Engl J Med.376:2319-2328 (2017).
- Scheller B. Opportunities and limitations of drug-coated balloons in interventional therapies. Herz. 36(3):232-239 (2011).
- Jeger RV, Eccleshall S, Ahmad W, et al. Drug-coated balloons for coronary artery disease. Third report of the international dcb consensus group. JACC Cardiovasc Interv. 13(12):1391-1402 (2020).
- Axel DI, Kunert W, Goggelmann C, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 96(2):636-645 (1997).
- Katsanos K, Spiliopoulos S, Kitrou P, et al. Risk of death following application of paclitaxel-coated balloons and stents in the femoropopliteal artery of the leg: A systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 7(24):e011245 (2018).
- Liistro F, Di Mario C. Paclitaxel-coated balloons in peripheral artery disease: How much is enough? Eur Heart J. 41(27):2553-2555 (2020).
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 40(2):87-165 (2019).
- Jeger RV, Farah A, Ohlow MA, et al. Drug-coated balloons for small coronary artery disease (BASKET-SMALL 2): An open-label randomized non-inferiority trial. Lancet. 392: 849-856 (2018).
- Cortese B, Di Palma G, Guimaraes MG, et al. Drug-Coated balloon versus drug-eluting stent for small coronary vessel disease: PICCOLETO II randomized clinical trial. JACC Cardiovasc Interv. 13(24):2840-2849 (2020).
- Tang Y, Qiao S, Su X, et al. Drug-coated balloon versus drug-eluting stent for small-vessel disease. JACC Cardiovasc Interv. 11(23):2381-2392 (2018).
- Sánchez JS, Chiarito M, Cortese B, et al. Drug-Coated balloons vs drug-eluting stents for the treatment of small coronary artery disease: A meta-analysis of randomized trials. Catheter Cardiovasc Interv. 1-10 (2020).
- Cortese B, Testa G, Rivero F, et al. Long-Term outcome of drug-coated balloon vsdrug-eluting stent for small coronary vessels: PICCOLETO-II 3-Year Follow-Up. JACC Cardiovasc Interv. 16(9):1054-1061 (2023).
- Baan Jr J, Claessen BE, Dijk KB, et al. A randomized comparison of paclitax eleluting balloon versus everolimus-eluting stent for the treatment of any in-stent restenosis: The DARE trial. J Am Coll Cardiol Intv. 11(3):275-283 (2018).
- Kleber FX, Rittger H, Ludwig J, et al. Drug eluting balloons as stand alone procedure for coronary bifurcational lesions: Results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 105(7):613-621 (2016).
- Scheller B, Ohlow MA, Ewen S, et al. Bare metal or drug-eluting stent versus drug-coated balloon in non-ST-elevation myocardial infarction: The randomised PEPCAD NSTEMI trial. Euro Intervention 15:1527-1533 (2020).
- Nishiyama N, Komatsu T, Kuroyanagi T, et al. Clinical value of drug-coated balloon angioplasty for de novo lesions in patients with coronary artery disease. Int J Cardiol. 222:113-118 (2016).
- Vos NS, Fagel ND, Amoroso G, et al. Paclitaxel-coated balloon angioplasty versus drug-eluting stent in acute myocardial infarction: The Revelation randomized trial. J Am Coll Cardiol Interv. 12(17):1691-1699 (2019).
- Gobić D, Tomulić V, Lulić D, et al. Drug-Coated balloon versus drug-eluting stent in primary percutaneous coronary intervention: A feasibility study. Am J Med Sci 354(6):553-560 (2017).
- Rissanen TT, Uskela S, Eranen J, et al. Drug-coated balloon for treatment of de-novo coronary artery lesions in patients with high bleeding risk (DEBUT): A single-blind, randomised, non-inferiority trial. Lancet. 394(10194): 230-239 (2019).
- Kleber FX, Mathey DG, Rittger H, et al. How to use the drug-eluting balloon: Recommendations by the German consensus group. Euro Intervention. (2011).
- Kleber FX, Rittger H, Bonaventura K, et al. Drug-coated balloons for treatment of coronary artery disease: Updated recommendations from a consensus group. Clin Res Cardiol. 102:785-797 (2013).
- Cortese B, Orrego PS, Agostoni P, et al. Effect of drug-coated balloons in native coronary artery disease left with a dissection. JACC Cardiovasc Interv. 8(15):2003-2009 (2015).
- Serruys PW, Keane D. The bailout stent. Is a friend in need always a friend indeed? Circulation. 88(5 Pt 1):2455-2457 (1993).
- Yeh RW, Secemsky EA, Kereiakes DJ, et al. Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention. JAMA. 315(16):1735-1749 (2016).
[CrossRef][Google Scholar][PubMed]s
- Cortese B, Micheli A, Picchi A, et al. Paclitaxel-coated balloon versus drug-eluting stent during PCI of small coronary vessels, a prospective randomized clinical trial. The PICCOLETO study. Heart. 96(16):1291-1296 (2010).
- Latib A, Colombo A, Castriota F, et al. A randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels: The BELLO (Balloon Elution and Late Loss Optimization) study. J Am Coll Cardiol. 60(24):2473-2480 (2012).
- Ghetti G, Bendandi F, Donati F, et al. Predictors of bail-out stenting in patients with small vessel disease treated with drug-coated balloon percutaneous coronary intervention. Catheter Cardiovasc Interv. (2023).
- Greco A, Sciahbasi A, Abizaid A, et al. Sirolimus-coated balloonversus everolimus-eluting stent in de novo coronary artery disease: Rationale and design of the Transform II randomized clinical trial. Catheter Cardiovasc Interv. 100(4):544-552 (2022).
- Horie K, Tanaka A, Taguri M, et al. Impact of prolonged inflation times during plain balloon angioplasty on angiographic dissection in femoropopliteal lesions. J Endovasc Ther. 25(6):683-691 (2018).
- Räber L, Mintz GS, Koskinas KC, et al. Clinical use of intracoronary imaging. Part 1: Guidance and optimization of coronary interventions. An expert consensus document of the European association of percutaneous cardiovascular interventions. Eur Heart J. 39(35):3281-3300 (2018).
- Yamamoto T, Ishii T, Ishida A, et al. Impact of post physiological assessment after treatment for de novo coronary lesions using drug-coated balloons. Int J Cardiol. 363:11-19 (2022).
- Shin ES, Ann SH, Singh GB, et al. Fractional flow reserve-guided paclitaxel-coated balloon treatment for de novo coronary lesions. Catheter Cardiovasc Interv. 88:193-200 (2016).
- Chung JH, Shin ES, Her AY, et al. Instantaneous wave-free ratio-guided paclitaxel-coated balloon treatment for de novo coronary lesions. Catheter Cardiovasc Interv 36: 179-185 (2020).
- Poerner TC, Duderstadt C, Goebel B, et al. Fractional flow reserve-guided coronary angioplasty using paclitaxel-coated balloons without stent implantation: feasibility, safety and 6-month results by angiography and optical coherence Tomography. Clin Res Cardiol. 106(1):18-27 (2017).