Case Report - Interventional Cardiology (2011) Volume 3, Issue 2
Bilateral arterial thoracic outlet syndrome with intermittent subclavian artery occlusion
- Corresponding Author:
- Kapildeo Lotun
Section of Vascular Medicine, 1200 E Broad Street
West Hospital, 5th Floor, Medical College of Virginia
Virginia Commonwealth University, Richmond
VA 23298, USA
E-mail: klotun@mcvh-vcu.edu
Abstract
Keywords
arterial thoracic outlet syndrome, bilateral thoracic outlet syndrome, cervical rib
Thoracic outlet syndrome (TOS) is an all inclusive term for symptomatic neurovascular bundle disorder when it passes between the anterior scalene and middle scalene muscles. The clinical presentation typically reflects the component of the neurovascular bundle affected. Arterial TOS represents a very small subset of this patient population, with neurogenic and venous compressive symptoms being more prevalent. These patients are frequently misdiagnosed, in part due to the heterogeneity of the patients and their respective clinical presentations.
Etiologically, a significant percentage of patients with TOS presenting with vascular compressive symptoms of the upper extremity have congenital bony abnormalities. Cervical ribs occur in a small percentage of the general population and in a majority of cases, when seen is an incidental finding. Arterial TOS is a rare presentation that may result from the compression of the subclavian artery as it courses through the neck to the axilla. In this article we present a case of a young female with symptoms of vascular insufficiency resulting from fixed and dynamic subclavian artery narrowing and occlusion secondary to a congenital cervical rib.
Case report
The patient studied is a 27-year-old righthanded female, nonsmoker, who presented with right upper extremity discomfort experienced for a total of 4 months. She works as a paralegal and her job requires a significant amount of typing. She reported the sudden onset of a dull ache occurring in her right upper extremity upon awaking one morning. This progressed from the level of the wrist, proximally to involve the forearm and upper arm, lasting 3–5 min and relieved by shaking or placing her arm in a dependent position. Her symptoms were exacerbated and reproduced by repetitive motion of the arm. She subsequently noticed episodes of hand pallor followed by bluish discoloration during periods of activity, and primarily nocturnal episodes of paresthesias and numbness of fingers and thumb which were apparent at rest.
She had incurred a cat scratch injury over the dorsum of her right hand 2 weeks earlier with delayed healing. Her arm pain had progressed to the point where it was present throughout the entire day. She was using oral contraceptive pills as her only medication, with an unremarkable review of systems and family history.
Physical examination revealed a well-nourished female, blood pressure of 134/79 mmHg of her left arm and no discernable blood pressure on the right. Her upper extremity examination revealed an edematous right hand with pallor on elevation and dependent rubor. There was mild hypothenar and thenar wasting with delayed capillary refill. The right axillary artery was palpable (2/2), the brachial, radial and ulnar pulses were not palpable, but Dopplerable with distant monophasic signals. There was an auscultated subclavian bruit at the supraclavicular fossa, which accentuated with arm abduction. Right upper extremity abduction at 90° led to significant diminution of axillary pulse and with extreme abduction no axillary pulse was detected. She had diminished pinprick sensation in her right thumb with intact motor function. Allen’s test was negative on the right and left hands, respectively. The left arm vascular examination was normal. There was a nonhealing scratch mark on the dorsum of the right hand.
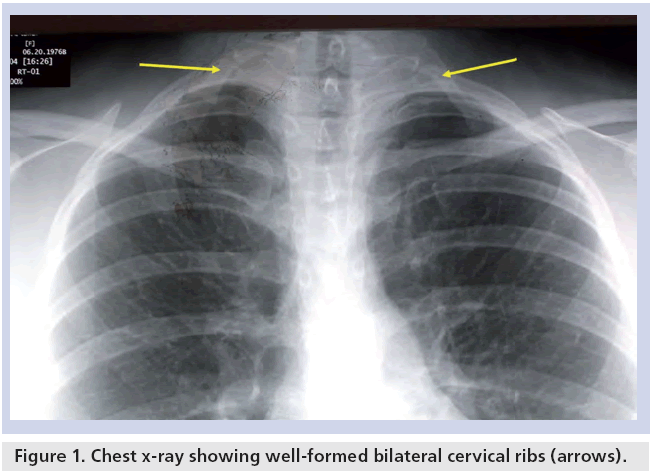
Connective tissue disease serologies and hypercoagulable disorder work-up were essentially negative. Her chest x-ray (Figure 1) revealed the presence of well-formed bilateral cervical ribs. Magnetic resonance angiography (MRA) of the great vessels and its major branches revealed mild dilatation of the distal right subclavian artery. Chest computed tomography with contrast confirmed the presence of bilateral cervical ribs and showed significant stenosis of the right subclavian artery between the clavicle and cervical rib. The latter rib articulated with the first thoracic rib. Both the subclavian artery and vein were significantly compressed with abduction maneuvers, although the brachial plexus appeared unremarkable. Duplex ultrasonography of the right upper extremity revealed normal flow velocity in the distal subclavian and the axillary arteries. The proximal brachial artery was occluded in the upper arm. There was arterial reconstitution of the radial and ulnar pulses in the forearm.
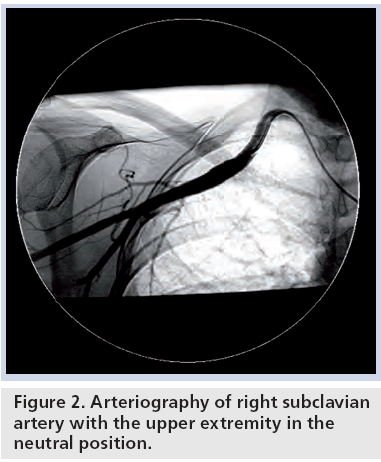
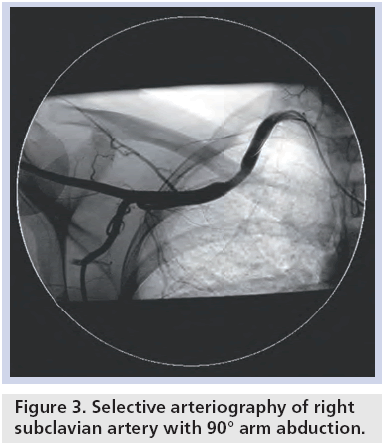
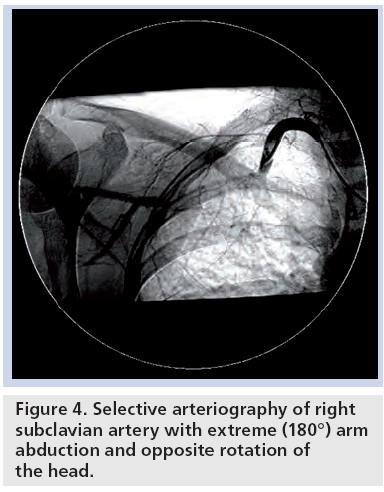
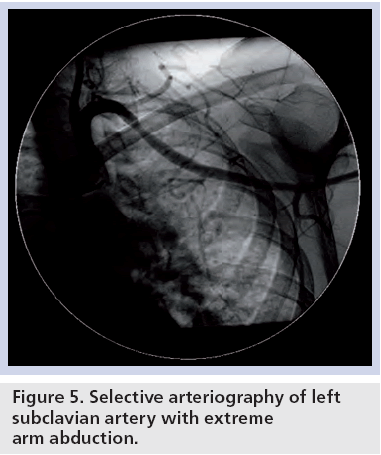
The patient subsequently underwent diagnostic contrast angiography from a right common femoral artery approach. Selective angiography of the right subclavian artery revealed a focal dilatation, distal to the second portion, involving the third portion of the subclavian artery and proximal axillary artery (Figure 2). The right subclavian and axillary arteries appeared patent. The brachial artery demonstrated total occlusion with reconstitution of the radial, ulnar and interosseous arteries. These three arteries remained patent to the wrist and both the deep and superficial palmar arches were well formed within the hand. Right upper extremity abduction at 90° demonstrated stenosis of the subclavian artery (Figure 3). Extreme abduction up to 180° and contralateral rotation of the head with hyperextension of the neck produced complete occlusion of the subclavian artery, leading to cessation of flow (Figure 4). Left subclavian artery angiography revealed patent subclavian, axillary and brachial arteries in the neutral position. With similar TOS provocative maneuvers, there was only a mild stenosis of the left subclavian artery (Figure 5).
Treatment began with antiplatelet therapy. Although thrombolytic therapy was considered, given the chronicity of symptoms the decision was made not to pursue this treatment option. Cardiothoracic surgery was consulted and the patient was eventually referred for definitive surgery. The cervical and first thoracic ribs were both surgically removed through a supraclavicular approach and a simultaneous arterial bypass with reverse saphenous vein was performed from the axillary to radial artery, given the symptomatic occlusion of the brachial artery. No definite repair of the subclavian artery was performed, because the surgeon did not feel that the poststenotic dilatation of the artery was significant to justify repair. There were no complications and postoperative course was uneventful. Follow-up examination revealed resolution of symptoms in the right arm with palpable radial and ulnar pulses. Duplex examination revealed patent axillo-radial bypass graft and normal graft velocities.
A total of 6 month later, she returned with symptoms suggestive of arterial insufficiency of the left arm. MR angiography confirmed the presence of a left cervical rib with aneurysmal dilatation of the left subclavian artery. She underwent successful left first rib and cervical rib resection via a transaxillary approach. Again no definite repair of the left subclavian artery was performed given the lack of stenosis and only mild aneurysmal dilatation. Her postoperative course was uneventful. She remained asymptomatic at the 6‑month and 2-year follow-up and physical examination revealed palpable right axillo–radial graft and normal palpable bilateral radial and ulnar arteries.
Discussion
Thoracic outlet syndrome is an all-inclusive term for symptomatic neurovascular bundle compartment disorders. The term TOS was first introduced by Peet in 1956 [1]. This phenomenon was originally described by Adson and colleagues in 1927, in a patient with a cervical rib and vascular injury, and at that time, thought to be solely an arterial compression problem [2]. However, cervical ribs have been observed throughout history were initially described by both Galen and Vesalius. It was in 1818 that the clinical connection between cervical ribs and symptoms was made by Astley Cooper [2]. In 1918, Halsted et al reported 21 patients with subclavian artery aneurysms is believed to be caused by a cervical ribs in a case series of 525 patients [3].
Although our patient sought fairly prompt medical attention, in most cases, a formidable delay in establishing the diagnosis of arterial TOS exists, likely due to its infrequent cause of TOS, and as a result is often misdiagnosed [4]. The heterogeneity of a patient’s presentation likely explains why the diagnosis may prove to be elusive. The neurovascular bundle as it courses down from the neck through the axilla may become compromised from surrounding structures; the resultant consequences may include dynamic or fixed stenosis of the subclavian vein or artery, as described in this article. Fixed stenosis may occur with hypertrophy of the scalene muscles or displacement and compression of the subclavian artery by the cervical rib or the fibrous band connecting the cervical rib to the first rib. The anatomic position of the cervical rib poses a functional limitation of the space termed the scalene triangle, which may lead to compression symptoms of TOS.
Patients with venous TOS are usually young and present with effort thombosis involving the dominant arm. Presenting symptoms include arm swelling and discomfort, and a constellation of symptoms referred to as Urshel’s sign including heaviness, redness of the arm, cyanosis and dilated, visible veins across the shoulder and upper arm [5].
Neurogenic TOS is usually more common in women occurring in the third and fourth decades of life. It is more common in patients with occupations requiring repetitive motion. Patients usually present with a history of neck trauma and symptoms consistent with nerve irritation, such as pain, paresthesias, and weakness in the arm and hand; this most often involves all five fingers, but is more pronounced in the fourth and fifth digits and the ulnar forearm. Some patients also complain of occipital headache due to the compression of the upper brachial plexus. Muscles of the neck and shoulder of the affected arm may be tender. A positive Tinel’s sign over the brachial plexus in the neck and reduced sensation to light touch in the fingers may be present. Although not diagnostic, provocative maneuvers may elicit the symptoms [4,6].
Bilateral cervical ribs were responsible for the vascular compromise observed in our patient. They occur in less than 1.0% of the general population. Two-thirds of cervical ribs occur in women. Importantly, 90% of these patients remain asymptomatic [4]. Patients with significant arterial compression, however, may demonstrate symptoms of vascular insufficiency resulting in limb ischemia. The compromised vessel may lead to a stenotic lesion, aneurysmal dilatation and result in thromboembolic events. In the early stages, patients may have symptoms suggestive of autonomic dysfunction such as unilateral cold hypersensitivity, Raynaud’s phenomenon, as well as episodes of rubor and recurrent edema. As demonstrated by our case, this disorder may often be erroneously attributed to musculoskeletal disorders or collagen vascular disease. The unilateral presentation of symptoms suggests that this is most likely an embolic or neurovascular compressive process. As the disorder progresses, patients may experience episodes of cold-induced ischemia, fingertip pain and frank punctate ischemic ulcers at the paronychial areas. Alternatively, in the face of progressive stenosis or complete arterial occlusion, patients will complain of aching in the hand and arm with exercise, and activity, or rest pain [7].
Our patient presented initially with exertionprovoked symptoms and poor wound healing secondary to compromised tissue perfusion. Her symptoms were limited to the dominant right arm, exclusively. It is plausible that her arm dominance and vocation requiring repetitive use of the right arm may be responsible for intermittent injury to the right subclavian artery. The intermittent arterial occlusion can lead to endothelial damage, stenosis and aneurysmal formation with potential thrombus generation. The genesis of poststenotic dilatation is thought to be vibration from turbulence caused by the stenosis [8]. The formation of local thrombus may be a cause of either antegrade or retrograde embolic events [9]. Approximately 12% of patients present with acute upper extremity ischemia and these patients tend to have a relatively worse clinical outcome and as such should be treated expeditiously and aggressively [9,10]. Our patient had a late embolic occlusion of the proximal brachial artery which explains her symptoms of ischemic rest pain. Neurogenic TOS is usually accompanied by varying degrees of arterial symptoms especially involving the lower trunk of the brachial plexus [11]. In this case, there was no compression on the brachial plexus even with provocative maneuvers, which explains the lack of neurologic symptoms.
Eliciting a comprehensive history in these patients should be focused on identifying possible inciting triggers, such as neck injuries or trauma from remote motor vehicle accidents, and those who use computers in nonergonomic positions for extended periods of time. Physical exam may reveal a palpable supraclavicular pulsatile mass and localized tenderness associated with the presence of a bruit. In addition, provocative TOS maneuvers to replicate symptoms may be useful. During the Adson’s maneuver, the patient is asked to turn their head toward the symptomatic shoulder while extending their arm, neck and shoulder away from the body, while the radial pulse is checked in the extended arm. Diminished pulse and reproduction of symptoms are considered a positive maneuver. Because false positives may occur, the unaffected side should also be checked. With the Wright test, a sitting patient is instructed to hyperabduct the arm with external rotation, while the pulse is checked in the affected arm. Again, a diminished pulse or reproduction of symptoms is considered positive for the presence of TOS. Similarly, the Roos test is performed with the patient in a sitting position, while both elbows are held at shoulder height while the shoulders are thrust back, and the patient is then asked to repeatedly open and close their fists for several minutes. Reproduction of symptoms and shoulder fatigue may indicate the presence of TOS. Approximately 56% of normal individuals will have a positive test on at least one provocative TOS maneuver [12]. Diagnostic imaging should include a chest x-ray with lordotic views, and cervical spine series, duplex ultrasonography, magnetic resonance angiography and/or computed tomography angiography may also be employed to identify structural and osseous abnormalities. Patients may ultimately require invasive contrast arteriography to delineate the vessel anatomy and assist in determining the therapeutic options appropriate to respective patients. Treatment with noninvasive conservative measures, such as stretching, massage, physical therapy or chiropractic manipulation, may be helpful in ameliorating symptoms [13].
Surgical treatment, when mandated, may require excision of the cervical rib to relieve symptoms, which may also include removal of anomalous muscles. A transaxillary, supraclavicular or posterior approach has been employed successfully in these surgical cases [14–16]. A combined supraclavicular and infraclavicular approach offers the advantage of complete exposure of the subclavian artery, cervical and first ribs, and delineates muscular and fibrous abnormalities [17]. Situations resulting in significant vascular injury may necessitate reconstructive surgery to repair the vessel defect. The indications for surgical arterial repair or bypass of the affected segment include mural thrombus and aneurysm formation. There is evidence that there is regression of the poststenotic dilatation after surgical removal of the first rib and the cervical rib [8,18].
The presence of a cervical rib and mild angiographic abnormality of the left subclavian artery in our patient presented us with a management dilemma. Being asymptomatic and involving her nondominant arm, the decision was made to treat her conservatively and follow her clinically with serial noninvasive tests, which would entail the addition of provocative maneuvers. However, she presented with left-sided TOS symptoms shortly after her first surgery. It is unclear, but certainly plausible, that she favored her left arm for daily activities following surgery. This led to intermittent left subclavian artery trauma and micro-injury resulting in vascular compromise. Involvement of the dominant arm in the symptomatology of arterial TOS has been documented in baseball players and certainly in cases of effort-induced axillary-subclavian vein thrombosis or Paget–von Schrotter syndrome [19–21]. Although not routinely advocated, there are few reports of bilateral cervical rib resection in case series of arterial TOS [22,23].
Conclusion
Thoracic outlet syndrome presenting with arterial occlusive symptoms has a varied clinical presentation. Careful history, comprehensive physical examination complemented by noninvasive imaging modalities, facilitates arriving at the correct diagnosis and instituting the appropriate treatment strategy for the respective patients. Surgical decompression remains the mainstay of treatment when symptoms dictate intervention.
Future perspective
Although TOS is a disease that has been recognized for more than a century, treatment options continue to evolve with the advent of endovascular therapies. Endoscopic or robotic surgery will probably be other treatment modalities that will become available in the near future.
Financial and competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ This article depicts a classic case of arterial thoracic outlet syndrome, secondary to congenital bilateral cervical ribs. The uniqueness of this case lies in that our patient had bilateral arterial occlusive symptoms, most likely a manifestation of her occupation which required typing. Complete subclavian arterial occlusion was observed with provocative maneuvers. The mainstay of treatment remains surgical decompression consisting of the cervical and first rib resection.
▪ Classic case of pure arterial thoracic outlet syndrome without any neurologic manifestations secondary to complete bilateral cervical ribs.
▪ Article describes bilateral symptomatology most likely related to her occupation and her arm usage.
▪ Intermittent complete subclavian artery occlusion with provocative maneuvers.
▪ Surgical decompression is the mainstay of treatment in arterial thoracic outlet syndrome.
References
- Peet RM, Henriksen JD, Anderson TP et al.: Thoracic-outlet syndrome: evaluation of a therapeutic exercise program. Proc. Staff Meet. Mayo Clin. 31(9), 281–287 (1956).
- Adson AW, Coffey JR: Cervical rib: a method of anterior approach for relief of symptoms by division of the scalenus anticus. Ann. Surg. 85(6), 839–857 (1927).
- Halsted WS: Dilation of the great arteries distal to partially occluding bands. Proc. Natl Acad. Sci. USA 4(7), 204–210 (1918).
- Sanders R, Hammond S: Management of cervical ribs and anomalous first ribs causing neurogenic thoracic outlet syndrome. J. Vasc. Surg. 36(1), 51–56 (2002).
- Urschel H, Patel A: Surgery remains the most effective treatment for Paget–Schroetter syndrome: 50 years’ experience. Ann. Thorac. Surg. 86(1), 254–260 (2008).
- Sanders R, Hammond S, Rao N: Thoracic outlet syndrome: a review. Neurologist 14(6), 365–373 (2008).
- Roos DB: Overview of thoracic outlet syndromes. In: Vascular Disorders of the Upper Extremity. Machleder HI (Ed.). Wiley-Blackwell, NJ, USA, 155–177 (1989).
- Robicsek F, Sanger PW, Taylor FH et al.: Pathogenesis and significance of post-stenotic dilatation in great vessels. Ann. Surg. 147(6), 835–844 (1958).
- Naz I, Sophie Z: Cerebral embolism: distal subclavian disease as a rare etiology. J. Pak. Med. Assoc. 56(4), 186–188 (2006).
- Lee T, Hines G: Cerebral embolic stroke and arm ischemia in a teenager with arterial thoracic outlet syndrome: a case report. Vasc. Endovascular Surg. 41(3), 254–257 (2007).
- Criado E, Berguer R, Greenfield L: The spectrum of arterial compression at the thoracic outlet. J. Vasc. Surg. 52(2), 406–411 (2010).
- Nord KM, Kapoor P, Fisher J et al.: False positive rate of thoracic outlet syndrome diagnostic maneuvers. Electromyogr. Clin. Neurophysiol. 48(2), 67–74 (2008).
- Huang J, Zager E: Thoracic outlet syndrome. Neurosurgery 55(4), 897–902 (2004).
- Roos DB: Transaxillary approach for first rib resection to relieve thoracic outlet syndrome. Ann. Surg. 163(3), 354–358 (1966).
- Maxey T, Reece TB, Ellman P et al.: Safety and efficacy of the supraclavicular approach to thoracic outlet decompression. Ann. Thorac. Surg. 76(2), 396–399 (2003).
- Johnson CR: Treatment of thoracic outlet syndrome by removal of first rib and related entrapments through posterolateral approach: a 22 year experience. J. Thorac. Cardiovasc. Surg. 68(4), 536–545 (1974).
- Cormier JM, Amrane M, Ward A et al.: Arterial complications of the thoracic outlet syndrome: fifty-five operative cases. J. Vasc. Surg. 9(6), 778–787 (1989).
- Roach MR: Poststenotic dilatation in arteries. In: Cardiovascular Fluid Dynamics (Volume 2). Bergel DH (Ed.). Academic Press, NY, USA, 111–139 (1972).
- McCarthy WJ, Yao JS, Schafer MF et al.: Upper extremity arterial injury in athletes. J. Vasc. Surg. 9(2), 317–327 (1989).
- Ligh C, Schulman B, Safran M: Case reports: unusual cause of shoulder pain in a collegiate baseball player. Clin. Orthop. 467(10), 2744–2748 (2009).
- Sevestre M, Kalka C, Irwin W et al.: Paget– Schroëtter syndrome: what to do? Catheter. Cardiovasc. Interv. 59(1), 71–76 (2003).
- Lutz BS, Matejic B, Ingianni G: Thoracic outlet syndrome: follow-up on 33 cases with regard to vascular compression. Int. J. Angiol. 7(3), 202–205 (1998).
- Casey RG, Richards S, O’Donohoe M: Vascular surgery of the upper limb: the first year of a new vascular service. Ir. Med. J. 95(4), 104–105 (2002).