Case Report - Neuropsychiatry (2019) Volume 9, Issue 3
Budd Chiari, Pain, Depression and Suicidal Thoughts
Konstantinos Kontoangelos1,2,†, Marina Economou1,2, Eleni Lazaratou1, Melanie Deutsch3, John Koskinas3, Charalambos Papageorgiou1,2
11st Department of Psychiatry, Eginition Hospital, School of Medicine, University of Athens, Athens, Greece
2University Mental Health Research Institute, Athens, Greece
32nd Academic Department of Internal Medicine, Medical School of National and Kapodistrian University of Athens, Hippokration General Hospital of Athens, Athens, Greece
- *Corresponding Authors:
- Konstantinos Kontoangelos
Athens University Medical School, 1st Department of Psychiatry
Psychiatry, Eginition Hospital, 74 Vas. Sofias Avenue, 11528, Athens, Greece
Tel: 0030-210-7289409
Fax: 0030-210-7242020
Abstract
ABSTRACT
Background
Budd–Chiari syndrome is caused by occlusion of the hepatic veins that drain the liver. It presents with abdominal pain, ascites, and liver enlargement.
Methods and findings
This is a case report of a female patient with depression, acute pain and suicidal thoughts treated with duloxetine and pregabalin before an invasive procedure to establish portosystemic shunt for the treatment of acute Budd Chiari syndrome.
Conclusion
Management of pain requires a comprehensive pain assessment and implement a multimodality treatment approach designed to address the pain and associated physical, psychosocial and behavioral problems of the patient.
Keywords
Budd chiari, Pain, Depression and suicidal thoughts
Introduction
Budd-Chiari syndrome (BCS) is a rare and potentially life-threatening disorder characterized by thrombotic obstruction of the hepatic outflow tract that transports blood from hepatic veins into the inferior vena cava [1]. This definition excludes sinusoidal obstruction syndrome and hepatic outflow obstruction secondary to rightsided cardiac disease [2]. Typical presentation consists of abdominal pain, and pain is one of the common reasons that patients visit the doctor, and during these appointments, physicians and all medical care professionals should evaluate patients for comorbidities such as depression, anxiety and suicidal thoughts [3]. This is a case report of a female patient with depression, acute pain and suicidal thoughts treated with duloxetine and pregabalin before an invasive procedure to establish portosystemic shunt for the treatment of acute Budd Chiari syndrome.
Case Presentation
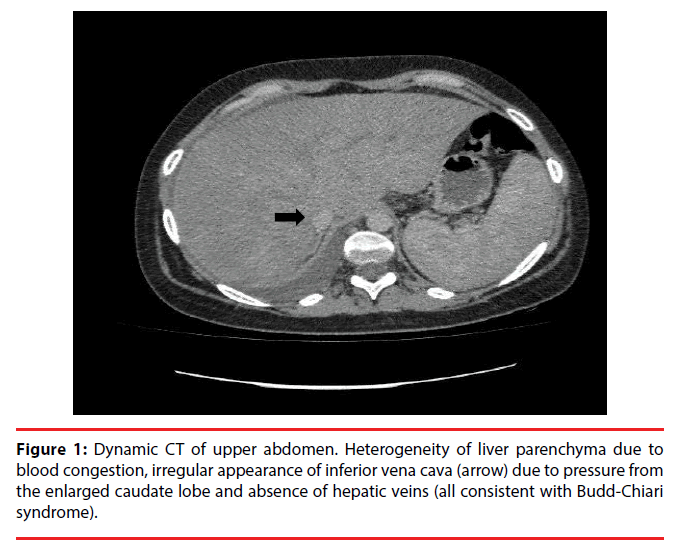
A 24‑year‑old female was admitted to the Hippokration General Hospital of Athens due to fever combined with progressive abdominal distension, abdominal pain and vomiting.. Upon admission, the patient was febrile with a slight pallor, and exhibited bilateral cervical, axillary and inguinal lymphadenopathy. Asystemic examination revealed a uniformly distended abdomen with tense ascites and no palpable mass. The liver was enlarged and the spleen was palpable 8 cm below the left costal margin (Figure 1). Mild edema was observed in the lower extremities. Blood analysis revealed a hemoglobin (Hb) level of 10.5 g/dl, white blood cell (WBC) count of 8.79 × 10 e3/uL(normal range, 5.2‑12.4 × 10.e3/uL), red blood cell(RBC) count of 3.72 × 10.e6/uL (normal range 4.2-6.1 × 10.e6/Ul) and platelet (PLT) count of 134 × 10 e3/uL (normal range 130-400 × 10.e3/uL )and D-Dimmer 1035.3 (normal range<500μg/L). Laboratory data showed elevated Erythrocyte Sedimentation Rate (ESR), 80 (normal range 5-15 mm); elevated C-Reactive Protein,79.90 (normal range 0.00-5.00); serum bilirubin [total bilirubin] (TB), 33.0 μmol/l (normal range, 3.4‑17.1 μmol/l); Fibrinogen(FIB) 504 (normal range 200-400 mg/dl); Activated Partial Thrompoplastin Time(APTT) 35.6 (Normal range 27-35 sec);direct bilirubin (DB), 0.90 (normal range, 0.00-0.50 mg/dl), total bilirubin 1,70(normal range, 0.20-1.20 mg/dl) and Gamma-glutamytransferase (γ-GT) levels of 70 (normal range, 9-36 U/l), with elevated alanine and aspartate aminotransferase levels(AST=52. ALT=78). Tests for human immunodeficiency virus (HIV) were negative. An abdominal computed tomography scan showed an enlarged liver, splenomegaly, splenic hilar varicose veins and right pleural effusion. Color Doppler studies revealed mechanical stenosis of the two hepatic veins alterations in the inferior caval vein in the posterior segment of the liver, due to an increase volume of the caudate lobe. These findings were consistent with Budd Chiari Syndrome (BCS). Surgery or a transjugular intrahepatic portosystemic shunt (TIPS) procedure was performed. She had depressed mood most of the day, nearly every day, diminished interest or pleasure in all, or almost all, activities most of the day, insomnia or nearly every day, fatigue or loss of energy nearly every day and feelings of worthlessness and recurrent thoughts of death and recurrent suicidal ideation with a specific plan (“I want to die. The pain is intolerable. I will take all my pills to suicide”). The intensity of the symptoms goes hand in hand with its physical condition and is consonant with the exacerbations and remissions of the disease. On the Short–Form McGill Pain Questionnaire [4], he scored I-a=22, II=Worst possible pain, III=3, while on the Beck Depression Inventory (BDI) [5], he had a score of 23. Pregabalin was gradually administered, with a starting dose of 75 mg once a day that over a period of two weeks increased to 75 mg three times a day. She was then prescribed duloxetine (30 mg/day) and the dosage of duloxetine was escalated to 60 mg/day after two weeks of titration and then 120 mg/ day after four weeks. The patient reported on his last assessment that he could be more active and less fearful of his pain symptoms that now were milder and her mood was improved. The patient gave informed consent, and was her anonymity preserved.
Discussion
BCS is a life-threatening hepatic vascular disorder. With the advancement of new therapeutic strategy, the prognosis of BCS has gradually improved [6]. In patients with BCS postoperative pain occurs and acute pain and stress engenders both a sensory and an emotional experience and is an adaptive response protecting the body from tissue damage like a burning fire or the attack of a predator [7]. Stress and pain engage the learning circuitry of the hippo-campus and amygdal [8]. In our patient duloxetine and pregabalin improved effectively the clinical condition concerning the pain and the psychomotor development. Pregabalin is a medicine that exerts its phamacodynamic effect by modulating voltage-gated calcium channels and has a linear pharmacokinetic profile. Pregabalin was shown to be effective in several models of neuropathic pain (incisional injury, inflammatory injury, and formalin-induced injury [9]. Pregabalin is particularly potent and effective as an analgesic, and is characterized by linear kinetics across a wide range of doses. Pregabalin is not metabolized by cytochrome P450 (CYP) enzymes or an inducer of drug-metabolizing enzymes. Pregabalin is particularly suitable because does not develop interaction with other drugs currently used for the treatment of chronic pain or associated psychiatric disorders (e.g. anxiety, depression) [10]. The antidepressive effect of pregabalin has been found to be associated with symptom relief in patients with generalized anxiety disorder and the anti-depressive effect of pregabalin one could postulate that the alleviation of the pain in our patient might be associated with the antidepressive effect of pregabalin, but this would be supported from the remarked improvement in his BDI scores [11]. Duloxetine, a dual reuptake inhibitor of serotonin and norepinephrine, is approved for the treatment of major depressive disorder, generalized anxiety disorder, diabetic peripheral neuropathic pain, fibromyalgia, and chronic musculoskeletal pain [12].
Conclusion
Chronic pain is a highly prevalent problem experienced by an extraodinarily heterogeneous patient population. The psychiatrist in the medical-surgical setting encounters a variety of issues involving difficulties with the managements of pain.These issues include recognition and alleviation of psychosocial stresses and depression. The management of chronic pain requires specific skills, including the ability to perform a comprehensive pain assesment and implement a multimodality treatment approach designed to adress the pain and associated physical, psychosocial and behavioral problems of the patient.
Conflict of Interest
The authors declare no conflict of interest.
References
- Martens P, Nevens F. Budd-Chiari syndrome. Uni. Euro. Gastroent. J 3(6), 489-500 (2015).
- DeLeve LD, Valla DC, Garcia-Tsao G, et al. Vascular disorders of the liver. Hepatology 49(5), 1729-1764 (2009).
- McGreevy K, Bottros MM, Raja SN. Preventing chronic pain following acute pain: risk factors, preventive strategies, and their efficacy. Eur. J. Pain. Suppl 11(5), 365-372 (2011).
- Melzack R .The short-form McGill Pain Questionaire. Pain 30(2), 191-197 (1987).
- Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch. Gen. Psychiatry 4(1), 561-571 (1961).
- Plessier A, Valla DC. Budd-Chiari syndrome. Semin. Liver. Dis 28(3), 259-269 (2008).
- McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol. Rev 87(3), 873-904 (2007).
- McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann. NY. Acad. Sci 1186, 190-222 (2010).
- Gajraj NM. Pregabalin: Its pharmacology and use in pain management. Anesth. Analg 105(6), 1805-1815 (2007).
- Chiechio S, Zammataro M, Caraci F, et al. Pregabalin in the treatment of chronic pain: an overview. Clin. Drug. Invest 29(3), 203-213 (2009).
- Stein DJ, Baldwin DS, Baldinetti F, et al. Efficacy of pregabalin in depressive symptoms associated with generalized anxiety disorder: a pooled analysis of 6 studies. Eur. Neuropsychophrmacol 18(6), 422-430 (2008).
- Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochr. Databa. Syst. Rev 3(1), CD007115 (2014).