Review Article - Interventional Cardiology (2023) Volume 15, Issue 5
Cardiovascular complications after lightning strike injury
- Corresponding Author:
- Indiresha Iyer
Department of Cardiovascular Medicine, Heart and Vascular Institute, Cleveland Clinic Akron General, Akron, Ohio, United States of America,
E-mail: IYERI@ccf.org
Received date: 08-Nov-2023, Manuscript No. FMIC-23-119672; Editor assigned: 10-Nov-2023, PreQC No. FMIC-23-119672 (PQ); Reviewed date: 24-Nov-2023, QC No. FMIC-23-119672; Revised date: 01-Dec-2023, Manuscript No. FMIC-23-119672 (R); Published date: 11-Dec-2023, DOI: 10.37532/1755-5310.2023.15(5).766
Abstract
Cloud to ground Lightning strikes is the second leading cause of weather-related deaths in the USA, recently accounting for approximately 28 deaths annually. Lightning strike injuries are more common in the summer months especially in the south- eastern and southern parts of the USA. Outdoor lightning strikes can result in death. Deaths due to lightning strikes are approximately 4 times more common in males and the average age of death about 37 years. Two-thirds of lightning associated deaths occur in the first hour of injury and are generally due to arrhythmias or respiratory failure. Patients hospitalized after Lightning Strike Injury (LSI) need to be monitored for cardiovascular events such as cardiac arrest, arrhythmias (ventricular, atrial and brady arrhythmias), myocardial damage, pericardial and aortic complications. There may be some gender differences in cardiac manifestations after lightning strike injury with one study reporting atrial arrhythmias predominantly in men and conduction blocks predominantly in women. The postulated mechanisms for cardiovascular manifestations include direct myocardial cell damage from the massive Direct Current (DC) current, electric arrhythmias due to depolarization mechanisms, severe vasospasm from catecholaminergic surge, blast injury and medullary dysfunction due to lightning injury of the brain. Cardiac arrest, Ventricular arrhythmias, Electrocardiography (ECG) pattern of ST-Segment Elevation Myocardial Infarction (STEMI) are associated with increased odds for mortality and myocardial contusion has been described on autopsy in those with cardiac manifestations. Reverse triage, Aggressive Cardiopulmonary Resuscitation and Standard (ACLS) protocols are recommended for the management of these patients. Technological advances in weather forecasting, public awareness and public policy are important in prevention of lightning strike injuries.
Keywords
Lightning strike injury • Arrhythmias; Myocardial damage • Cardiac arrest
Introduction
Lightning is a natural severe weather phenomenon. According to the National Oceanographic and Atmospheric Administration, Cloud-to-Ground (CG) and Intra- Cloud (IC) lightning flashes are detected and mapped in real-time by two different networks in the United States-the National Lightning Detection Network and Total Lightning Network [1]. Earth Net’s Total Lighting network detected 441 million lightning pulses in 2020 over the US. Of those, 31 million (7%) were Cloud to Ground Lightning strikes. Lightning counts are higher in the Southeast, Midwest and South [2].
Literature Review
Epidemiology of lightning strike injuries and deaths
The risk of being struck by lightning is estimated by the National Weather Service (NWS) to be 1 in 1.2 million based on a 10-year average between 2009-2018 [3]. (Appendix, Tables S1-S3, Figures S1 and S2). Although rare, lightning strike injuries can be deadly and remain the second leading cause of weather- related deaths in the US. Between 1989-2018, the US has averaged 43 deaths due to lightning annually [3]. There is a decreasing trend in the annual number of deaths due to lightning with an average of 27 Lightning Strike fatalities for the period 2009-2018 [3]. However, the number of lightning strikes is projected to increase by 12% for every degree of rise in global average air temperatures [4].
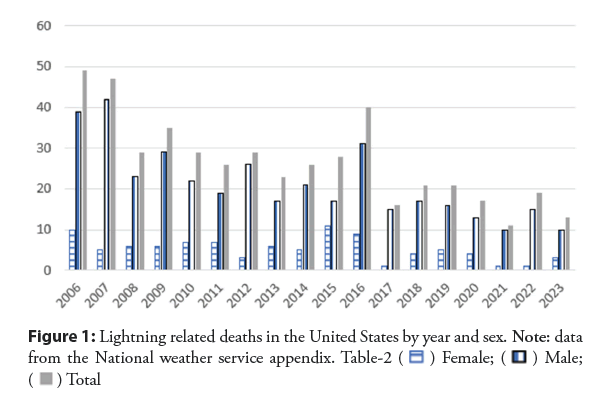
According to the CDC there were 444 lightning strike deaths in the United States between 2006 and 2021. The average age at the time of death was 37 years [5], and an age range of 10-60 years [6]. Men were 4 times more likely to be affected by a Lightning Strike Injury (LSI). The states of Florida, Texas, Colorado, North Carolina, Alabama, Arizona, Georgia, Missouri, New Jersey, and Pennsylvania had the most LSIs and deaths. The summer months, especially July and weekends saw the highest number of LSIs and deaths. Also, two thirds of lightning strike fatalities occurred between noon and 6 pm. Although, a third of LSI occurred indoors, Outdoor LSI is associated with mortality, especially outdoor leisure related activities such as fishing, boating, playing sports and relaxing at the beach (Figure 1) [6].
Mechanisms of lightning strike injury
Human contact with lightning can occur by different physical mechanisms. The postulated mechanisms are: 1) Direct Lightning strike; 2) Indirect Lightning strike due to contact with an object that was directly struck such as an umbrella, golf club or pole; 3) A side flash where part of the electric current jumps from a struck object such as a tree to the individual nearby; 4) Step voltages produced by current flowing from a struck object through the ground to an individual standing nearby with one step closer to and one step further from the source creating a potential difference; 5) Lightning leader process results from progressive ionization of air below a charged cloud resulting in successive pre-discharges that progressively reach closer to the earth. This results in an opposite electrostatic charge build up in the earth and in individuals directly in that area can cause upward streamers which connect with the pre-discharges to create successive lightning strikes; 6) Explosive barotrauma due to rapid expansion (in microseconds) of superheated air (>30000 K) around the cylindrical luminous channel resulting in an outward propagating shock wave that causes mechanical trauma to any object in its path [7-11].
The estimated distribution of LSI by mechanism in descending frequency is Ground Current (40%-50%) Side Flash (20%-30%) Contact (15%-25%) Upward Leaders (10%-15%) Direct strike (3%-5%) and Blunt trauma (unknown) (Figure 2) [9].
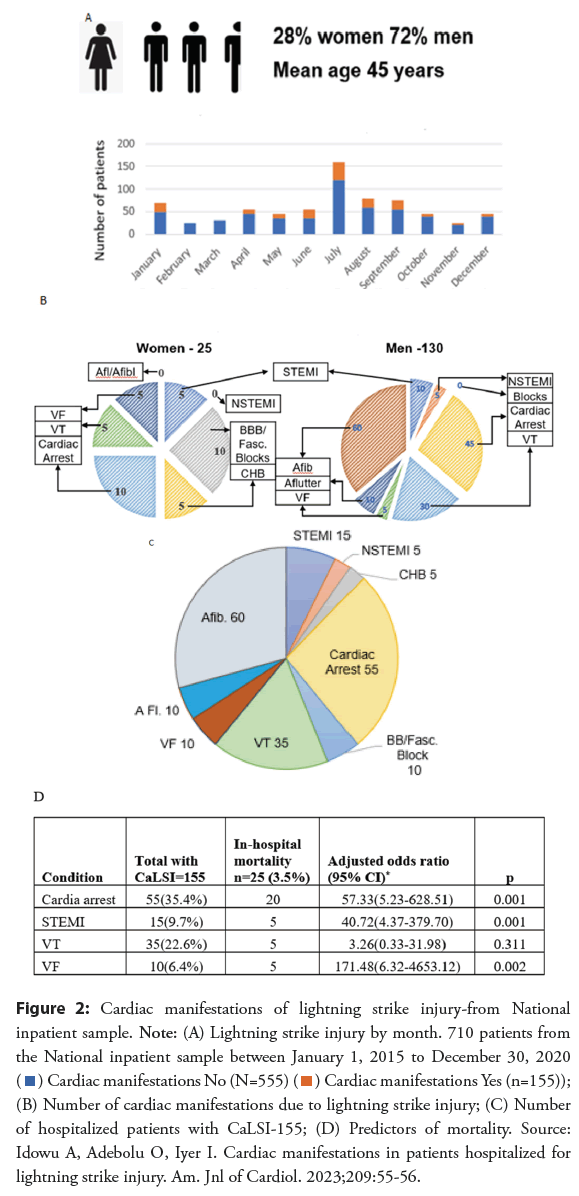
Figure 2: Cardiac manifestations of lightning strike injury-from National inpatient sample. Note: (A) Lightning strike injury by month. 710 patients from the National inpatient sample between January 1, 2015 to December 30, 2020  (B) Number of cardiac manifestations due to lightning strike injury; (C) Number
of hospitalized patients with CaLSI-155; (D) Predictors of mortality. Source:
Idowu A, Adebolu O, Iyer I. Cardiac manifestations in patients hospitalized for
lightning strike injury. Am. Jnl of Cardiol. 2023;209:55-56.
(B) Number of cardiac manifestations due to lightning strike injury; (C) Number
of hospitalized patients with CaLSI-155; (D) Predictors of mortality. Source:
Idowu A, Adebolu O, Iyer I. Cardiac manifestations in patients hospitalized for
lightning strike injury. Am. Jnl of Cardiol. 2023;209:55-56.
Pathology and pathogenesis of lightning strike cardiovascular manifestations
Clinical presentation in lightning strike victims vary greatly per individual depending upon the mechanism of physical contact with lightning, the points of entry and exit and by current following the path of least resistance. Nerves followed by blood and muscles have the least resistance while bones and dry skin have higher resistance [7,8]. This may explain the preponderance for neurological and cardiovascular damage among these patients [7]. In a wet individual, the wet skin and clothing may offer lower resistance than the body and a significant portion of the electric current may be diverted [10].
The high energy of a lightning discharge in a direct hit to the upper torso or head is associated with a high incidence of cardiac injury. Such high current (10,000 to 30,000 Amperes) can result in temporary asystole and respiratory arrest [11-13]. Respiratory arrest secondary to lightning-induced medullary center dysfunction has also been implicated in asystole [14]. In a sheep lightning model, initial asystole followed by perfusing arrhythmias and later permanent asystole has been reported [15]. Both VF and asystole have been reported as initial documented arrhythmias in humans with LSI [16]. In many cases of initial asystole, cardiac automaticity can return along with return of spontaneous circulation [17]. In some cases, respiratory arrest can persist and the ensuing hypoxia will lead to asystole or pulseless electrical activity [15]. Based on studies of electrical injury, small amplitude currents can induce VF such as seen with a side-flash in LSI [18]. The Ventricular Fibrillation (VF) can spontaneously convert to Ventricular Tachycardia (VT) and into Sinus rhythm [19]. If VF is untreated it deteriorates into asystole. This occurred after approximately 30 minutes in a swine model of electrically induced VF [20].
Autopsy studies have shown the presence of myocardial contusion, hemorrhage and necrosis both in normal sized hearts and those with hypertrophied or enlarged hearts [7,16]. Massive compression of the anterior chest and rapid deceleration, as seen with blunt cardiac trauma are common causes of cardiac contusions [21]. Blast effects of LSI is the likely mechanism of myocardial contusion. Such structural damage plausibly forms the substrate for non-sustained and sustained ventricular arrhythmias [22], which can occur early or present late [23]. Other mechanisms that concurrently cause myocardial damage include direct effect of catecholamines and coronary vasoconstriction due to neuro-sympathetic activation triggered by physical and mental stress [24,25]. The degree of vasoconstriction has been shown to correlate with the response to Acetylcholine infusion [25].
Prolonged coronary vasospasm causing myocardial ischemia after LSI has been attributed to catecholamine surge, similar to the mechanisms in Takotsubo cardiomyopathy and in cases of phaeochromocytoma [26-28]. These mechanisms can result in ventricular dysfunction and arrhythmias.
Both clinical and autopsy reports of patients with LSI have described pericardial tear with hemopericardium, pericarditis (acute, persistent and recurrent and pericardial effusion) [11,16]. Direct atrial myocardial damage, pericardial inflammation related to contusion, neurohormonal changes and secondary effects of ventricular dysfunction may be contributory to the development of atrial arrhythmias.
Aortic intimal tears have been described and can be attributed to the blast effects although not well established [16].
The mechanism of Cardiac conduction blocks after LSI may be due to massive electrical current causing direct myocardial damage involving the Sinus node, Atrioventricular (AV) node and Bundle of HIS regions, similar to that seen on autopsy after high voltage electric injury [29].
Clinical cardiac manifestations of lightning strike injury
Lightning-related cardiovascular manifestations range from immediate to delayed (days to even weeks) and can be lethal or benign, transient or permanent [11,23]. Among patients hospitalized after LSI, 22% had varying cardiac manifestations [30]. Patients may manifest with asystole, Ventricular fibrillation or Ventricular tachycardia [10-13,17-19]. Acute or delayed pulmonary edema may occur both due to ventricular dysfunction and non-cardiogenic pulmonary edema [12]. Clinical and echocardiographic wall motion abnormality with left ventricular dysfunction, Takatsubo cardiomyopathy and biventricular heart failure are not uncommon cardiovascular findings [31].
The cardiac conduction system can also be affected. Conduction disturbances such as blocks, repolarization abnormality (non- specific ST-T wave changes, T-wave infarction), QT prolongation, atrial and ventricular arrhythmias (especially atrial fibrillation, ventricular tachycardia, and ventricular fibrillation), cardiac arrest have been reported in the literature [32]. One study reported some gender differences with atrial arrhythmias seen predominantly in males and conduction blocks mostly in females [30].
Electrocardiographic findings of myocardial infarction are also common after LSI, and they are often due to non-sustained coronary vasospasm rather than plaque rupture as coronary angiography most often shows no significant epicardial obstructive coronary artery disease [11,12,14,31]. There can be an elevation in cardiac biomarkers/enzymes (troponin, brain natriuretic peptide, creatinine kinase) after LSI probably because of myocardial contusion or free radical cellular injury [11,12,14]. The prognostic significance of elevation in these markers is yet unknown.
Postural orthostatic tachycardia syndrome has been reported as a late sequela of lightning-related autonomic dysfunction [33].
In patients with Cardiac Implantable Electronic Devices (CIEDs), a precautionary device check is also advised, Apart from one case report of elevated lead thresholds and erasure of pacemaker device memory following a lightning strike, there is a paucity of data on the short- and long-term impact of lightening on CIEDs [34,35]. CIEDs may function normally and an Implantable Cardioverter Defibrillator (ICD) has been shown to save a patient from VF induced by LSI [18].
Discussion
Risk factors for cardiovascular mortality
Some inferences can be made regarding risk factors for mortality based on descriptions of victims and on Autopsy studies. The mortality among patients with LSI is reported to be between 10%-30% with worldwide mortality rates estimated to be 0.2-1.7 deaths per million people per year with geographic differences in mortality [7]. Two-thirds of lightning associated deaths occur in the first hour of injury and are generally due to arrhythmias or respiratory failure [4].
Direct Strikes are associated with larger currents than a side flash. Direct strikes to the chest arms or head are more likely to be associated with cardiovascular manifestations than strikes to the lower torso [11]. Some patients on autopsy had an enlarged heart or cardiac hypertrophy which may have put them at higher risk for mortality [11].
In a review of 66 cases, among those with serious LSI, Mortality was 77% in those who presented with cardiopulmonary arrest, 38% in those with cranial burns and 30% among those with leg burns [13]. In a retrospective study, Cardiac arrest, Ventricular arrhythmias and STEMI by ECG were associated with increased odds of mortality among hospitalized patients after LSI [30].
Treatment implications
In 1968, Helen Taussig noted that individuals who were alive immediately after a LSI, the majority go on to recover, while those who appear to have no heart action and no respiratory movements need cardiopulmonary resuscitation the most, reminding that “those who are stunned but alive are not the ones who most urgently need help” [36]. This concept of’ reverse triage’ is supported by the rationale that the majority of individuals with LSI are younger and hence more likely to be otherwise relatively healthy. Cardiac automaticity can return even after prolonged asystole and prognosis can be excellent even in cases of prolonged respiratory arrest with aggressive cardiopulmonary resuscitation [37,38].
Since LSI occur outdoors, conditions for rescuers are likely suboptimal or even dangerous. While attending to patients after LSI is important, dispatchers and rescuers need to be mindful of the weather conditions, the condition of the immediate vicinity, address any potential lurking electrical hazards for rescuers, transport the victim to safety before continuing with rescue efforts and the possibility of failure of external defibrillators if the victim is wet. All these may delay initiation of resuscitation efforts.
Even those who do not seem to have any significant injury after lightning strike need to be monitored in a medical facility as some patients may develop cardiac manifestations later [39]. Since myocardial injury after LSI is unlikely to be related to epicardial coronary artery disease even in the presence of STEMI changes on ECG, such patients also can be treated at the nearest medical facility than transfer only to a facility with primary PCI capability. The strategy of expectant management to reduce coronary vasospasm after LSI, hoping to mitigate adverse cardiac events while logical, needs to be tested.
After discharge, a routine follow-up examination, including repeat Electrocardiogram (EKG) about 1-4 weeks after LSI may be prudent even in stable patients to evaluate for late sequelae [40].
Prevention
The decrease in Lightning strike deaths since the 1950s may reflect the impact of better weather forecasting, technological advances and wide broadcast of weather information on popular media resulting in greater public awareness of anticipated severe weather, policies related to participation in organized outdoor activities during severe weather [41], as well as dissemination of lightning safety tips by several organizations such as the CDC and the National weather service [42,43].
Future directions
Public policy approaches to prevention such as active push notifications of extreme weather alerts instead of voluntary subscription to weather alerts, modifying public places near outdoor leisure activities to withstand lightning may further reduce LSIs. Greater understanding of the clinical course of patients with LSIs requires standardization of data collection and information sharing such as through an international registry as espoused previously [44]. Such a registry may allow pragmatic trials of treatment approaches such as possible role of prophylactic prevention of coronary vasospasm upstream at the site of rescue..
Conclusion
Lightning strikes resulting in injury and deaths from lightning have shown a decreasing trend. LSIs are more common in young adult males in the summer months engaged in outdoor leisure activities, especially on weekends and in water-based leisure activities. Mortality is between 10%-30% and mainly due to cardiorespiratory and neurological damage. The immediate, acute and delayed cardiovascular manifestations of lightning strike injury include cardiac arrest, cardiac arrhythmias, myocardial damage, ventricular dysfunction, pericarditis and aortic damage. Cardiac arrest, Ventricular arrhythmias and STEMI by ECG are cardiac manifestations associated with increased odds of mortality among those hospitalized after lightning strike injury. Treatment of victims requires “reverse triage”, immediate aggressive resuscitation efforts, rapid transportation to hospitals and close monitoring. Prevention through avoidance of outdoor activity during severe thunderstorms using public policy and information sharing is important.
References
- NOAA-Severe weather 101: Lightning detection.
- 2020 US lightning report. (2003).
- From national weather service-How dangerous is lightning? (2023).
- Romps DM, Seeley JT, Vollaro D, et al. Molinari J Projected increase in lightning strikes in the United States due to global warming. Science. 346(6211):851-854 (2014).
- US lightning report
- National weather service. 1870
- Blumenthal R. Injuries and deaths from lightning. J Clin Pathol. 74(5):279-284 (2021).
- Blumenthal R, Jandrell IR, West NJ, et al. Does a sixth mechanism exist to explain lightning injuries?: Investigating a possible new injury mechanism to determine the cause of injuries related to close lightning flashes. Am J Forensic Med Pathol. 33(3):222-226 (2012).
- Cooper MA, Holle RL. Mechanisms of lightning injury should affect lightning safety messages (2010).
- López J, Urgoiti V, Gonzalez M, et al. Brief communication: A multi-disciplinary approach to a side-flash lightning incident to human beings in the Basque Country. Nat Hazards Earth Syst Sci.13:721-726 (2013).
- Lichtenberg R, Dries D, Ward K, et al. Cardiovascular effects of lightning strikes. J Am Coll Cardiol. 21(2):531-536 (1993).
- Kleiner JP, Wilkin JH. Cardiac effects of lightning stroke. JAMA. 240(25):2757-2759 (1978).
- Cooper MA. Lightning injuries: Prognostic signs for death. Ann Emerg Med. 9(3):134-138 (1980).
- Saglam H, Yavuz Y, Yurumez Y, et al. A case of acute myocardial infarction due to indirect lightning strike. J Electrocardiol. 40:527-530 (2007).
- Kroll MW, Luceri RM, Efimov IR, et al. The electrophysiology of electrocution. Heart Rhythm O2. 4(7):457-462 (2023).
- Wetli CV. Keraunopathology: An Analysis of 45 Fatalities. Am J Forensic Med Pathol. 17(2): 89-98 (1996).
- Ravitch MM, Lane R, Safar P, et al. Lightning stroke: Report of a case with recovery after cardiac massage and prolonged artificial respiration. N Engl J Med. 264:36-38 (1961).
- Kondur AK, Afonso LC, Berenbom LD, et al. Implantable cardioverter defibrillators save lives from lightning-related electrocution too! Pacing Clin Electrophysiol. 31(2):256-257 (2008).
- Altalhi A, Al-Manea W, Alqweai N, et al. Cardiac rhythm recorded by implanted loop recorder during lightning strike. Ann Saudi Med. 37(5):401-402 (2017).
- Kroll MW, Gregory PW, Raymond EI, et al. The stability of electrically induced ventricular fibrillation. Annu Int Conf IEEE Eng Med Biol Soc. 2012:6377-6381 (2012).
- El-Andari R, O'Brien D, Bozso SJ, et al. Blunt cardiac trauma: A narrative review. Mediastinum. 5:28 (2021).
- Robert E, de La Coussaye JE, Aya AG, et al. Mechanisms of ventricular arrhythmias induced by myocardial contusion: A high-resolution mapping study in left ventricular rabbit heart. Anesthesiology. 92(4):1132-1143 (2000).
- Drigalla D, Essler SE, Stone CK, et al. Delayed onset of atrial fibrillation and ventricular tachycardia after an automobile lightning strike. J Emerg Med. 53(5):740-745 (2017).
- Bloom S, Davis DL. Calcium as mediator of isoproterenol-induced myocardial necrosis. Am J Pathol. 69(3):459-470 (1972).
- Yeung AC, Vekshtein VI, Krantz DS, et al. The effect of atherosclerosis on the vasomotor response of coronary arteries to mental stress. N Engl J Med. 325(22):1551-1556 (1991).
- Dundon BK, Puri R, Leong DP, et al. Takotsubo cardiomyopathy following lightning strike. BMJ Case Rep. (2009).
- Hayashi M, Yamada H, Agatsuma T, et al. A case of takotsubo-shaped hypokinesis of the left ventricle caused by a lightning strike. Int Heart J. 46(5):933-938 (2005).
- Santos JRU, Brofferio A, Viana B, et al. Catecholamine-induced cardiomyopathy in pheochromocytoma: How to manage a rare complication in a rare disease? Horm Metab Res. 51(7):458-469 (2019).
- James TN, Riddick L, Embry JH, et al. Cardiac abnormalities demonstrated postmortem in four cases of accidental electrocution and their potential significance relative to nonfatal electrical injuries of the heart. Am Heart J. 120(1):143-157 (1990).
- Idowu A, Adebolu O, Iyer I, et al. Cardiac manifestations in patients hospitalized for lightning strike injury. Am J Cardiol. 209:55-56 (2023).
- McIntyre WF, Simpson CS, Redfearn DP, et al. The lightning heart: A case report and brief review of the cardiovascular complications of lightning injury. Indian Pacing Electrophysiol J. 10(9):429-434 (2010).
- Christophides T, Khan S, Ahmad M, et al. Cardiac effects of lightning strikes. Arrhythm Electrophysiol Rev. 6(3):114-117 (2017).
- Grubb BP, Karabin B. New onset postural tachycardia syndrome following lightning injury. Pacing Clin Electrophysiol. 30(8):1036-1038 (2007).
- Obszański B, Tułecki Ł, Kutarski A, et al. Lightning-induced pacing system malfunction: A case report. Eur Heart J Case Rep. 3(2):ytz092 (2019).
- Ginwalla M, Battula S, Dunn J et al. Termination of electrocution-induced ventricular fibrillation by an implantable cardioverter defibrillator. Pacing Clin Electrophysiol. 33(4):510-512 (2010).
- Taussig HB. Death from lightning-and the possibility of living again. Ann Intern Med. 68(6):1345-1353 (1968).
- Part 8: advanced challenges in resuscitation. Section 3: Special challenges in ECC. 3G: electric shock and lightning strikes. Resuscitation. 46(1-3):297-299 (2000).
- Zafren K, Durrer B, Herry JP, et al. Lightning injuries: Prevention and on-site treatment in mountains and remote areas. Official guidelines of the International Commission for Mountain Emergency Medicine and the Medical Commission of the International Mountaineering and Climbing Federation (ICAR and UIAA MEDCOM). Resuscitation. 65(3):369-372 (2005).
- Davis C, Engeln A, Johnson EL, et al. Wilderness medical society practice guidelines for the prevention and treatment of lightning injuries: 2014 update. Wilderness Environ Med. 25(4 Suppl):S86-S95 (2014).
- Van RR, Eikendal T, Kooij FO, et al. A shocking injury: A clinical review. Injury. 53(10):3070-3077 (2022).
- Walsh KM, Cooper MA, Holle R, et al. National athletic trainers' association position statement: Lightning safety for athletics and recreation. J Athl Train. 48(2):258-270 (2013).
- Natural Disasters and Severe Weather. Lightning safety tips. (2022).
- Molinari J Projected increase in lightning strikes in the United States due to global warming
- Pfortmueller CA, Yikun Y, Haberkern M, et al. Injuries, sequelae, and treatment of lightning-induced injuries: 10 years of experience at a swiss trauma center. Emerg Med Int. 2012:167698 (2012).