Review Article - Interventional Cardiology (2021)
Cardiovascular diseases and obesity: The concise systematic review in the context of SARS-CoV-2
- Corresponding Author:
- Idiberto José Zotarelli Filho
Department of Clinical Research,
FACERES–Faculty of Medicine of Sao Jose do Rio Preto,
Sao Paulo,
Brazil,
E-mail: dr.idibertozotarelli@faceres.com.br
Received date: July 05, 2021 Accepted date: July 19, 2021 Published date: July 26, 2021
Abstract
Introduction: COVID-19 disease is associated with vascular inflammatory processes, myocarditis, and cardiac arrhythmias, worsening CVD, diabetes, and hypertension. In this scenario, SARS-CoV-2 is worsening the comorbidities of obesity.
Objective: To conduct a summary systematic review on the main relationships of COVID-19 with cardiovascular diseases and obesity, highlighting the main physiometabolic and pathological mechanisms.
Strategy: The search strategy was carried out in the PubMed, Embase, Ovid and Cochrane Library, Web of Science, and Scopus databases. After a complete analysis of these selected studies, in the scenario of cardiovascular diseases (CVD), obesity initially favors the development of inflammation in adipose tissue, by increasing the production of pro-inflammatory adipokines. Metainflammation leads to myocardial dysfunction by direct injury to inflammatory mediators, as well as by dysfunction to other organs. Thus, the endothelial dysfunction caused by SARS-CoV-2 justifies blood vessel-related comorbidities such as cardiovascular disease, hypertension, diabetes, and obesity are more likely to develop severe COVID-19.
Conclusion: COVID-19 disease is associated with a high inflammatory load that can induce vascular inflammation, myocarditis, and cardiac arrhythmias. Cardiovascular disease and pharmacological inhibition of COVID-19 increase ECA2 levels, which can increase the virulence of the coronavirus in the lung and heart. Also, obesity is an important predictor of worsening SARS-CoV-2 pathology.
Keywords
SARS-CoV-2 • COVID-19 • Cardiovascular diseases • Obesity • Inflammatory processes
Introduction
The new coronavirus (SARS-CoV-2), whose disease is COVID-19, in March 2020, spread around the world causing respiratory diseases and deaths mainly in risk groups, mainly in obese, diabetic, and cardiovascular disease patients (CVD) [1]. Thus, the World Health Organization (WHO) declared a Public Health Emergency of International Importance, and the pandemic was declared [2].
In this context, COVID-19 disease is associated with vascular inflammatory processes, myocarditis, and cardiac arrhythmias, worsening CVD, diabetes, and hypertension. These disorders share the underlying pathophysiology related to the renin-angiotensin system [2]. In this context, some mechanisms can contribute to increasing the virulence of the coronavirus in the lung and heart, for example, cardiovascular disease and the pharmacological inhibition of Renin angiotesin system can increase the levels of Angiotensin-Converting Enzyme 2 (ACE2) or coronavirus infection may decrease ACE2, leading to excessive accumulation of angiotensin II, which induces acute respiratory distress syndrome and fulminant myocarditis [2]. In this sense, among patients with COVID-19, there is a high prevalence of cardiovascular disease and more than 7% of patients have a myocardial injury due to infection, about 22% of critically ill patients [2,3].
In this sense, SARS-CoV-2 can significantly affect cardiac function and cause myocardial damage, as ACE2 is used by the coronavirus to initiate infection [3]. Thus, it is necessary to assess cardiovascular damage in patients infected with SARS-CoV-2 and determine the correlation of pro-terminal type B serum natriuretic peptide (NT-proBNP) and cardiac troponin I (cTnI) with the severity of COVID-19 [2].
Also, obesity stands out as a multifactorial disease that can cause several public health problems [3,4]. Currently, about 30% of the world’s population is overweight or obese. By 2020, it is estimated that more than 60% of the world’s population will be overweight or obese. In this context, there are 2.0 billion overweight and obese people in the world [4]. In Brazil, this chronic disease has increased by 67.8% in the last thirteen years, from 11.8% in 2006 to 19.8% in 2018 [5].
In this context, SARS-CoV-2 is causing worsening obesity comorbidities [6]. Immunity plays a decisive role in SARS-CoV-2 infection. The lack of regulation and the excessive immune response to the viral stimulus exacerbate pro-inflammatory cytokines (cytokine storm), reaching a state of hyper inflammation, with consequent damage to various tissues of the obese [6,7]. It is known that obesity initially favors the development of inflammation in adipose tissue, by increasing the production of pro-inflammatory adipokines, such as IL-6 and TNF-α. Thus, the proportion between pro-inflammatory and anti-inflammatory cytokines becomes unbalanced [8]. Consequently, damage to the vascular system occurs, promoting endothelial dysfunction, characterized by a decrease in the production of nitric oxide and an increase in the synthesis of reactive oxygen species, which establishes an inflammatory and oxidative stress state [9].
In this sense, meta-inflammation describes the junction of inflammation with the metabolic changes that occur in the body of obese patients [7]. Several toxic mediators that contribute to the inflammatory state and tissue damage are present in obesity, such as Free Fatty Acids (FFA), toxic lipid derivatives, such as diacylglycerol, toxic nitric oxide metabolites, and inflammatory mediators, such as protein C reactive, cytokines, chemokines, macrophages, and TNF-α. Highlighted [8]. As a corollary to the exacerbated inflammatory process, the coagulation cascade is unregulated, causing hypercoagulability. Therefore, the endothelial dysfunction caused by SARS-CoV-2 justifies why patients with blood vessel-related comorbidities such as cardiovascular disease, hypertension, diabetes, and obesity are more likely to develop severe COVID-19, even death [6]. Therefore, the present study aimed to conduct a summarized systematic review on the main relationships of COVID-19 with cardiovascular diseases and obesity, highlighting the main physiometabolic and pathological mechanisms.
Methods
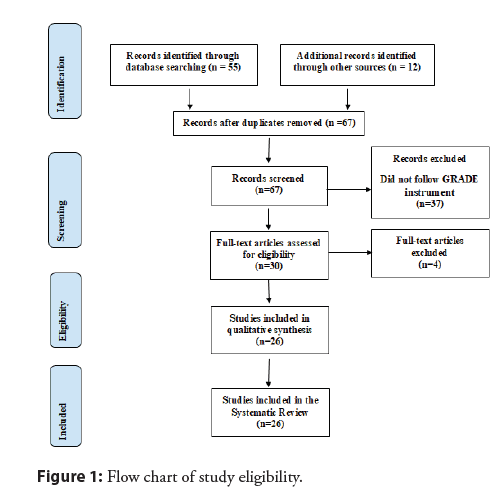
Study design: The present study followed a concise systematic review model, following the rules of systematic review-PRISMA (Transparent reporting of systematic reviews and meta-analyzes).
Search strategy and information sources: The search strategy was carried out in the databases PubMed, Embase, Ovid and Cochrane Library, Web of Science, and Scopus, following the following steps: -search for descriptors: SARS-CoV-2. COVID-19. Cardiovascular diseases. Obesity. Inflammatory processes, and the use of Booleans “and”, “or” and “not” among historical findings.
Study quality and bias risk: The quality of the studies was based on the GRADE instrument, with randomized controlled clinical studies, prospective controlled clinical studies, and studies of systematic review and meta-analysis listed as the studies with the greatest scientific evidence. The risk of bias was analyzed according to the Cochrane instrument.
Development and Discussion
After the literary search criteria, a total of 67 studies were found that were submitted to the eligibility analysis, and, after that, 26 studies of high to medium quality and with risks of bias were selected that do not compromise the scientific basis of the studies (Figure 1). After a complete analysis of these selected studies, in the scenario of cardiovascular diseases (CVD), obesity initially favors the development of inflammation in adipose tissue, by increasing the production of pro-inflammatory adipokines, such as IL-6 and the TNF-After the literary search criteria, a total of 67 studies were found that were submitted to the eligibility analysis, and, after that, 26 studies of high to medium quality and with risks of bias were selected that do not compromise the scientific basis of the studies (Figure 1). After a complete analysis of these selected studies, in the scenario of cardiovascular diseases (CVD), obesity initially favors the development of inflammation in adipose tissue, by increasing the production of pro-inflammatory adipokines, such as IL-6 and the TNF-α [7].
Consequently, damage to the vascular system occurs, promoting endothelial dysfunction, characterized by a decrease in the production of nitric oxide and an increase in the synthesis of reactive oxygen species. Highlighted, the endothelial dysfunction caused by SARS-CoV-2 justifies blood vessel-related comorbidities such as cardiovascular disease, hypertension, diabetes, and obesity [6].
Also, the presence of Diabetes Mellitus (DM) and CVD can increase the risk of death by 12 times [10-14]. As evidence, in a cohort study of 191 patients from Wuhan, China, any comorbidity was present in 48% (67% of non-survivors), hypertension in 30% (48% of non-survivors), DM in 19% (31% of non-survivors) and CVD in 8% (13% of non-survivors) [15].
Besides, in a cohort of 138 hospitalized patients with COVID-19, similar prevalent comorbidities were 46% overall and 72% in patients requiring care in the Intensive Care Unit (ICU), as well as cardiovascular comorbidities such as hypertension in 31% (58% in patients requiring care in the ICU), CVD in 15% (25% in patients requiring care in the ICU) and DM in 10% (22% in patients requiring care in the ICU) [16].
Also, an analysis of an outpatient and hospital cohort of 1,099 patients with COVID-19 revealed that 24% had some comorbidity (58% among those with intubation or death), with 15% having hypertension (36% among those with intubation or death), 7.4% DM (27% among those with intubation or death) and 2.5% of coronary disease (9% among those with intubation or death) [6].
In this context, data from the National Health Commission of China showed that 35% of patients diagnosed with COVID-19 had hypertension and 17% had coronary disease [17]. A recent meta-analysis of 8 studies from China, including 46,248 infected patients, showed that the most prevalent comorbidities were hypertension [18]. Possible explanations include CVD being more prevalent in patients with advanced age and immune system with functional deficiency or high levels of ACE2 or patients with CVD who are predisposed to COVID-19 [16,17].
In this sense, there are two patterns of myocardial injury with COVID-19. Thus, a study demonstrated that four days after the onset of symptoms, the mean levels of hs-cTnI were 8.8 pg / mL in non-survivors versus 2.5 pg/mL in survivors. During follow-up, the median hs-cTnI among survivors did not change significantly (2.5 to 4.4 pg/mL), while it rose to 24.7 pg/mL on day 7, to 55.7 pg / mL in the day 13, to 134.5 pg/mL on day 19 and 290.6 pg/mL on day 22 in non-survivors [15]. The mean time of death since the onset of symptoms was 18.5 days (interquartile range, 15 to 20 days). The increase in the hs-cTnI range with other inflammatory biomarkers (D-dimer, ferritin, interleukin-6, lactate dehydrogenase), raising the possibility that this reflects a storm of cytokines or secondary hemophagocytic lymphohistiocytosis more than isolated myocardial injury [15].
In the context of ACE2, the use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers is common in cardiovascular disorders (hypertension, coronary artery disease, congestive heart failure, and DM) [18]. However, there is conflicting data on whether these drugs increase [19-22] or have a minimal effect on ACE2 levels. The entry of SARS-CoV-2 into cells is dependent on ECA2, however, ECA2 appears to have a protective function against acute lung injury [23,24]. In this regard, losartan is being studied for potential mitigation of lung injury among hospitalized and outpatients with COVID-19 [25,26]. The use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers (ACEI and ARB) does not appear to affect the morbidity and mortality of COVID-19 combined with CVD. Aggravating causes of death include fulminant inflammation, accumulation of lactic acid, and thrombotic events [24-26].
Therefore, patients with COVID-19 combined with cardiovascular disease are associated with an increased risk of mortality [25]. Critical patients are characterized by fewer lymphocytes. The highest BMI is seen most frequently in critically ill patients, not survivors. The use of ACEI/ARB does not affect the morbidity and mortality of COVID-19 in combination with CVD. Aggravating causes of death include fulminant inflammation, accumulation of lactic acid, and thrombotic events. Therefore, cardiovascular metabolic comorbidities made patients more susceptible to COVID-19 and exacerbated the infection [26].
Also, in the obesity scenario, adiponectin and leptin are the most abundant adipokines synthesized by adipose tissue, although there are others such as TNF-α, IL-6, IL-1, CC-Chemokine Ligand 2 (CCL2), visceral adipose -tissue-derived serine protease inhibitor (vaspin), and Retinol-Binding Protein 4 (RBP4) [6]. The excess of adipose tissue increases the production of several adipokines that have a great impact on several bodily functions. In this case, food intake control and energy balance, immune system, insulin sensitivity, angiogenesis, blood pressure, lipid metabolism, and body homeostasis stand out, situations strongly correlated with cardiovascular disease [22]. The adipokines with anti-inflammatory action stand out as the IL1 receptor antagonist (IL-1ra), transforming growth factor-β (TGF-β), those produced by Th2 cells (IL-4, IL-5, and IL -10) and adiponectin [6]. The imbalance between pro and anti-inflammatory cytokines can induce inflammatory or hypersensitive responses. Also, high plasma adiponectin concentrations are associated with a reduced risk of myocardial infarction in men. Adiponectin is inversely proportional to the concentration of C-Reactive Protein (CRP). It can negatively regulate the gene expression of CRP in the adipocyte [6].
Besides, it should be noted that the adipose tissue of obese individuals has an upregulation of the expression of the ECA2 enzyme, which functions as an input receptor for SARS-CoV-2 in the cell. Thus, adipose tissue serves as a target and a potential viral reservoir. Thus, obesity is a pathology that causes damage to the immune system and amplifies inflammatory responses and this contributes to understanding the interaction between COVID-19 and obesity [6].
Conclusion
COVID-19 disease is associated with a high inflammatory burden that can induce vascular inflammation, myocarditis, and cardiac arrhythmias. Thus, cardiovascular risk factors and conditions must be carefully controlled according to evidence-based guidelines. Cardiovascular disease and pharmacological inhibition of COVID-19 increase ACE2 levels, which can increase coronavirus virulence in the lung and heart. Also, obesity is an important predictor of worsening SARS-CoV-2 pathology. There are a complex interaction between multiple metabolic, immunological and inflammatory factors that result in metainflammation.
Conflict of Interest
The authors declare no conflict of interest.
Funding
None.
Data Sharing Statement
No additional data are available.
References
- WHO: World Health Organization (2020).
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 34: 101623 (2020).
- Wenzhong L, Hualan L. COVID-19: Attacks the 1-Beta chain of hemoglobin and captures the porphyrin to inhibit human heme metabolism. Chem Rxiv (2020).
- OMS: Organização Mundial de Saúde. Disponível (2020).
- Associação Brasileira Para O Estudo DA Obesidade E DA síndrome metabólica. Diretrizes brasileiras de obesidade (2016).
- Kass DA, Duggal P, Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 395 (10236): 1544-1545.
- Schetz M, De Jong A, Deane AM, et al. Obesity in the critically ill: A narrative review. Intensive Care Med. 45 (6): 757‐769 (2019).
- Apovian CM. Obesity: Definition, comorbidities, causes, and burden. Am J Manag Care. 22 (S7): S176‐S185 (2016).
- Andolfi C, Fisichella PM. Epidemiology of obesity and associated comorbidities. J Laparoendosc Adv Surg Tech A. 28 (8): 919‐924 (2018).
- Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 141 (20): 1648-1655 (2020).
- Chan JW, Ng CK, Chan YH, et al. Short term outcome and risk factors for adverse clinical outcomes in adults with Severe Acute Respiratory Syndrome (SARS). Thorax. 58 (8): 686-689 (2003).
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382: 1708-1720 (2020).
- Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 289 (21): 2801-2809 (2003).
- Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): A systematic review and meta-analysis. Int J Infect Dis. 49: 129-133 (2016).
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 395 (10229): 105401062 (2020).
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 323 (11): 1061-1069 (2020).
- Zheng YY, Ma YT, Zhang JY, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 17 (5): 259-260 (2020).
- Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int J Infect Dis. 94: 91-95 (2020).
- Klimas J, Olvedy M, Ochodnicka-Mackovicova K, et al. Perinatally administered losartan augments renal ACE2 expression but not cardiac or renal Mas receptor in spontaneously hypertensive rats. J Cell Mol Med. 19 (8): 1965-1974 (2015).
- Walters TE, Kalman JM, Patel SK, et al. Angiotensin converting enzyme 2 activity and human atrial fibrillation: increased plasma angiotensin converting enzyme 2 activity is associated with atrial fibrillation and more advanced left atrial structural remodelling. Europace. 19 (8): 1280-1287 (2017).
- Burchill LJ, Velkoska E, Dean RG, et al. Combination renin-angiotensin system blockade and angiotensin-converting enzyme 2 in experimental myocardial infarction: Implications for future therapeutic directions. Clin Sci (Lond). 123 (11): 649-658 (2012).
- Burrell LM, Risvanis J, Kubota E, et al. Myocardial infarction increases ACE2 expression in rat and humans. Eur Heart J. 26 (4): 369-375 (2005).
- Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 436 (7047): 112-116 (2005).
- Kuba K, Imai Y, Rao S, et al. A crucial role of Angiotensin Converting Enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 11 (8): 875-879 (2005).
- Randomized controlled trial of losartan for patients with COVID-19 not requiring hospitalization. (2020).
- Randomized controlled trial of losartan for patients with COVID-19 requiring hospitalization (2020).