Image Article - Interventional Cardiology (2023) Volume 15, Issue 6
Catastrophic case of mesenteric ischemia after routine TAVR
- Corresponding Author:
- James Gore
Department of Internal Medicine, Ochsner Clinic Foundation, New Orleans, United States of America,
E-mail: james.gore@ochsner.org
Received date: 03-Jan-2024, Manuscript No. FMIC-24-124390; Editor assigned: 05-Jan-2024, PreQC No. FMIC-24-124390 (PQ); Reviewed date: 19-Jan-2024, QC No. FMIC-24-124390; Revised date: 26-Jan-2024, Manuscript No. FMIC-24-124390 (R); Published date: 02-Feb-2024, DOI: 10.37532/1755- 5310.2023.15(6).775
Description
Surgical Aortic Valve Replacement (SAVR) has long been the mainstay of therapy for severe aortic stenosis. However, for patients who are not candidates for open surgery, Transcatheter Aortic Valve Replacement (TAVR) is now generally accepted as the new standard of care for symptomatic aortic stenosis [1]. Although TAVR outcomes continue to improve, the risk of vascular injury, stroke, paravalvular regurgitation, and valve durability remain. Acute Mesenteric Ischemia (AMI) is an uncommon, but life- threatening medical condition associated with poor prognosis. Current data on AMI after TAVR is limited. We present a case of AMI caused by an embolus following recent TAVR for severe aortic stenosis [2].
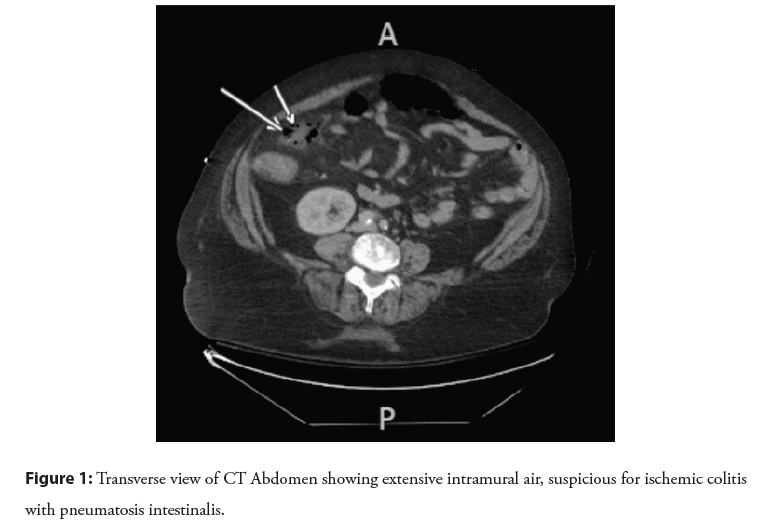
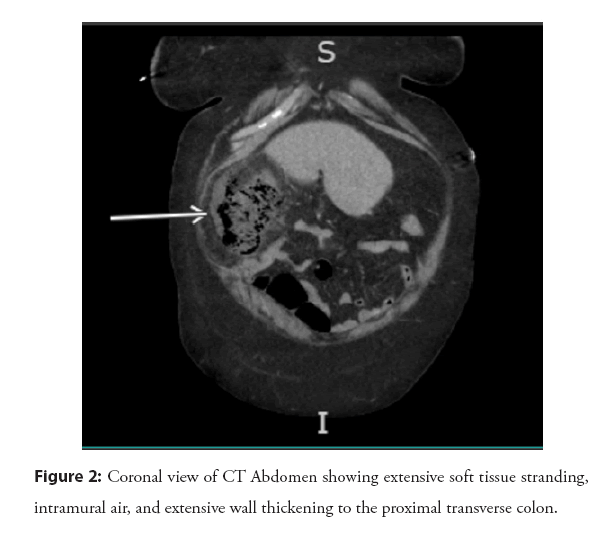
64 y/o F with severe AS who presented with abdominal pain and nausea. Patient recently underwent TAVR 1-week prior which was completed without complication. On physical exam distended protuberant abdomen, hypoactive bowel sounds, tenderness to deep palpation in all 4 quadrants. WBC of 19.5 (H), lactate of 0.8 (normal), and Procal of 7.6 (H). Patient became hypotensive, necessitating admission to the ICU for pressor support following a cardiac arrest. CT Abdomen Pelvis with Contrast showed extensive wall thickening of the cecum to the proximal transverse colon involving the Superior Mesenteric Artery (SMA) territory, with interval extensive intramural air suggesting sequela of ischemic colitis with pneumatosis intestinalis [3,4]. Colorectal Surgery decided to perform emergent exploratory laparotomy. Laparotomy revealed ischemic necrosis of R hepatic flexure. Necrotic bowel suspected to be caused by embolism from recent TAVR performed 1 week before presentation to hospital as shown in the Figures 1 and 2.
Conclusion
The occurrence of AMI after TAVR is rare, but still possible. Embolism leading to thromboembolic events should be considered in patients who have received a TAVR. Our case demonstrates how the lack of serum lactate elevation does not rule out mesenteric ischemia, and high index of suspicion is critical for a timely diagnosis. Moreover, this case exemplifies the importance of considering diagnostic laparoscopy sooner than later if inflammatory markers and physical examination findings are highly suggestive of ischemia.
References
- Noguchi M, Tabata M, Ito J, et al. Successfully treated nonocclusive mesenteric ischemia after transcatheter aortic valve replacement. Ann Thorac Surg. 103(2): e171-e173 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Val DD, Rivero F, Cuesta J, et al. Fatal acute mesenteric ischaemia following transcatheter aortic valve replacement. EuroIntervention. 17(7):588-589 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Hiranuma W, Murata Y, Matsuoka T, et al. Non-occlusive mesenteric ischemia after trans-catheter aortic valve implantation with thyroid storm: A case report. J Cardiol Cases. 27(1): 19-22 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Young MN, Inglessis I. Transcatheter aortic valve replacement: Outcomes, indications, complications, and innovations. Curr Treat Options Cardio Med. 19(10): 81 (2017).
[CrossRef] [Google Scholar] [PubMed]