Case Report - Clinical Practice (2018)
Cerebral toxoplasmosis in an HIV negative patient: the first documented case report in Africa and literature review
- Corresponding Author:
- Christine Katusiime
Luvley Diseases Institute, Kampala, Uganda
E-mail: katutina1@gmail.com
Abstract
Background: Cerebral toxoplasmosis in HIV negative persons is extremely rare. To the best of our knowledge, this is the first documented case of cerebral toxoplasmosis in an HIV negative individual in Africa. Case presentation: We present a 45-year-old HIV negative Ugandan woman who was diagnosed with cerebral toxoplasmosis. Both serology for Toxoplasma gondii and cerebral magnetic resonance imaging (MRI) were positive for cerebral toxoplasmosis. The patient showed remarkable clinical improvement following initiation of chemotherapy and maintains clinical improvement. Conclusion: This case illustrates the rarity of cerebral toxoplasmosis in HIV negative persons. To the best of our knowledge, this is the first documented case of cerebral toxoplasmosis in an HIV negative person in Africa and the first documented female case of its kind. This case without a doubt, underscores the necessity of routine screening for cerebral toxoplasmosis in HIV negative patients that present with neurological symptoms.
Keywords
Toxoplasma gondii, cerebral toxoplasmosis, HIV negative.
Introduction
Globally, toxoplasmosis is recognized as an infection caused by Toxoplasma gondii, an obligate intracellular protozoan parasite that is acquired typically through intake of raw or undercooked meat containing bradyzoits, through ingestion of oocysts in cats feaces, mother-to-unborn child transmission, blood transfusion and transplantation [1,2].
A third to half of the global human population has been documented as being infected with T. gondii [3,4]. Toxoplasmosis notably causes major debilitating sequellae in the central nervous systems (CNS) of immunosuppressed persons particularly those with HIV infection. This case highlights a case of cerebral toxoplasmosis in a patient without HIV/AIDS in Uganda.
Case report
A 45-year-old African woman presented to the infectious disease unit of a private hospital in Kampala, Uganda with a 7-month history of headache, bilateral lower limb weakness and a 2-month history of visual blurring in the left eye. Her headaches were generalized, throbbing, non-radiant, with no associated or aggravating factors though were mildly relieved with non-steroidal antiinflammatory drugs. She had no history of dizziness, vomiting, loss of consciousness, loss of balance, numbness or seizures. She had no history of ever being a pet-owner-in particular owning a cat. She owned a food business in a local area of the city that was directly adjacent to a chicken raring coup for more than 10 years. She had visited several physicians who had purportedly made a diagnosis of brucellosis.
Neurological examination revealed a patient with a Glasgow coma scale 8/15, bilateral paraparesis, positive babinski’s sign and a reduced power in both lower limbs of 3/5. She also had a convergent squint in the left eye. General, dermatologic, respiratory and cardiovascular systemic review did not yield significant findings.
With continual deterioration, she was taken to yet another physician who had ordered an MRI scan of the brain. The MRI had revealed multi-focal intra-cranial lesions.
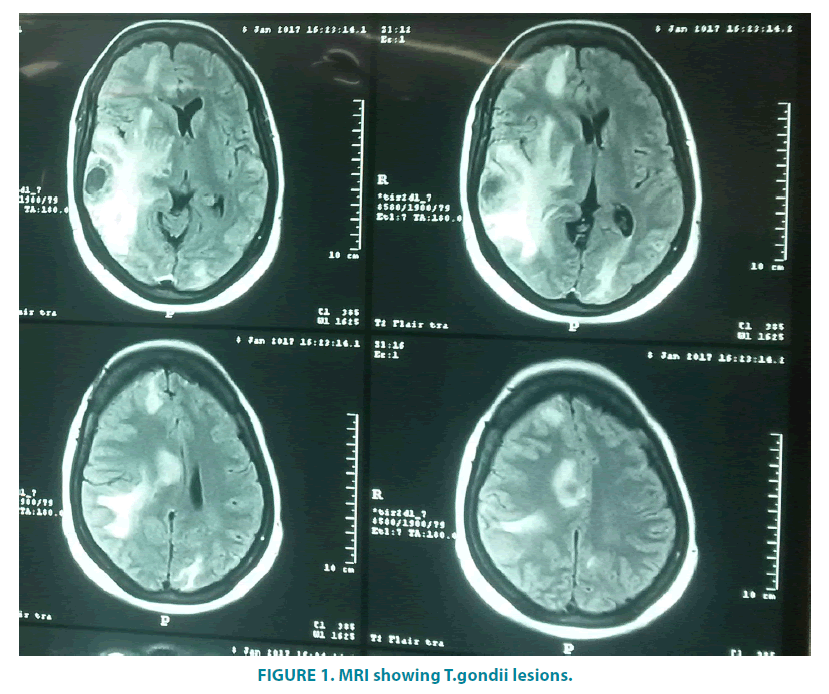
The gadolinium-enhanced MRI showed multiple variable sized; well-enhanced lesions in the right temporal-parietal, right frontal, left parietal lobes and right lentiform nucleus and part of the right thalamus and right subenpendymal area (FIGURE 1). The largest lesion in the right temporo-parietal region had extensive large perifocal edema exerting mass effect in form of subfalcine herniation measuring about 39 × 24 mm. The second largest lesion in the right lentiform nucleus and right thalamus with large perifocal edema measured about 20 × 22 mm. Other lesions were noted in the dura on the left. There was a right to left midline shift of 9 mm. All lesions depicted significant ring enhancement (FIGURE 1).
Chest and Lumbar-sacral X-rays and ultrasound scans of the pelvis and abdomen were not significant. Additional tests that were discussed with the patient’s attendant were MRI-guided brain biopsy, and ophthalmologic review which were both declined by the attendant because of financial constraints.
Laboratory investigations revealed a total white blood cell count of 7.93 × 109/L, platelet count of 201 × 109/L and hemoglobin of 12.8 g/dL. Random blood sugar, liver function tests, renal function tests and serum electrolytes were normal. Multiple HIV serological tests that had been done by the patient over a series of the past 4 years, as part of selfinitiated health status assessment at different testing centers were negative. Additional HIV antibody tests for HIV-1/2 and an HIV viral load were negative. Hepatitis B surface antigen (HBsAg), rheumatoid factor, serum CRAG and antinuclear antibody (ANA) tests were negative. Toxoplasma serological IgG was found to be positive 1.55 U/mL (reference positive range > 1.1 U/mL).
Soon after, the patient was taken to the village by her attendant to seek traditional remedies, against medical advice, for a period of 2 weeks, having initially declined to commence high-dose trimethoprim/ sulfamethoxazole for cerebral toxoplasmosis.
With continual counseling and followup, the patient was brought back to the city centre having deteriorated to a much more critical condition, with a GCS of 4/15, two weeks after the diagnosis date, and hospitalized. The patient was initiated on high-dose trimethoprim/sulfamethoxazole, dexamethasone and analgesics. Following 4 weeks of strict directly-observed therapy, the patient remarkably improved clinically with significant recovery in her alert level to a fully conscious state with the ability of short and long-term memory recall, articulation of speech, and mobility.
Discussion
This is the first documented observation of primary cerebral toxoplasmosis in an HIVnegative individual in Uganda and the first on the African continent. As high as 50% of the world’s human population, is asymptomatic with T.gondii infestation [3,4]. Studies have shown that in HIV negative individuals, T. gondii infestation was greatly linked to the consumption of either undercooked or raw meat [2,5]. HIV/AIDS is therefore not a prerequisite for cerebral toxoplasmosis.
According to country reports, the highest numbers of published cases were from USA, India, Japan and Germany.
Low endemic countries included Australia, Croatia, Romania, China, Pakistan, Switzerland, Greece, Iran, Malaysia, Czech Republic, Korea, Belgium, Portugal, Austria, Canada and Taiwan. There have virtually been no reports from African countries. This is possibly because of insufficient diagnostic facilities and a low index of suspicion of Toxoplasmosis in HIV-negative persons.
Cerebral disease denotes reactivation of latent parasitic infestation [6]. Most documented cases showed underlying conditions that contributed to toxoplasma infestation. Our patient presented with neurological symptoms: headache and bilateral paraparesis; this is in keeping with study findings that illustrate that the most common symptom of cerebral toxoplasmosis in immune-competent individuals is headache [6]. Furthermore, the differential diagnosis of toxoplasmosis was considered in our patient when the history disclosed her occupationshe had run a food business in a local area of the city for over 10 years that was adjoined to an open chicken enclosure. The suspicion of consumption of undercooked or raw meat was strongly considered and prompted us to run a serological screening test to rule out toxoplasmosis.
The MRI in our patient depicted multiple regions affected by T. gondii: the right temporal-parietal lobe, right frontal lobe, left parietal lobe, right lentiform nucleus and part of the right thalamus and right subenpendymal areas. All lesions showed significant ring enhancement. Although the patient’s spouse declined a brain biopsy, cerebral toxoplasmosis was confirmed from the positive serum toxoplasma titer levels. Radiological improvements on MRI can be detected in as little as within10 days of initiation of treatment, in keeping with the immediate and remarkable clinical improvement that we saw in our patient. Our patient showed significant clinical improvement after initiation of highdose co-trimoxazole, and she is still adhering to her medications.
The MRI in our patient depicted multiple regions affected by T. gondii: the right temporal-parietal lobe, right frontal lobe, left parietal lobe, right lentiform nucleus and part of the right thalamus and right subenpendymal areas. All lesions showed significant ring enhancement. Although the patient’s spouse declined a brain biopsy, cerebral toxoplasmosis was confirmed from the positive serum toxoplasma titer levels. Radiological improvements on MRI can be detected in as little as within10 days of initiation of treatment, in keeping with the immediate and remarkable clinical improvement that we saw in our patient. Our patient showed significant clinical improvement after initiation of highdose co-trimoxazole, and she is still adhering to her medications.
Upon review of literature, we have not come across a similar case regarding immunocompetent persons in Uganda or Africa.
Conclusion
This case underscores the necessity of screening for cerebral toxoplasmosis in immune-competent patients that present with neurological symptoms. Early diagnosis and treatment is paramount, as undiagnosed parasitic T.gondii infestation can be fatal.
Ethics approval and consent to participate
Ethics approval is not applicable.
Authors’ contributions
The author diagnosed the patient, drafted, edited and approved the final manuscript.
Funding
No funds were received towards care or manuscript preparation.
Acknowledgements
I am principally indebted to the revelation by Prophet Elvis Mbonye. I am grateful to the patient’s immediate family members particularly Mrs. Peace Mukurungu and Mr. Sam, that ensured strict drug adherence. I am also grateful for the technical assistance that was provided by Dr. Clara Komuhangi. I would also like to acknowledge the logistic assistance provided by Mr. Ronald Tusiime and Mr. Kanyesigye.
Competing interests
The author declared that she has no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
References
- Kistiah K, Winiecka-Krusnell J, Barragan A, Karstaedt A, Frean J. Seroprevalence of Toxoplasma gondii infection in HIV-positive and HIV-negative subjects in Gauteng, South Africa. South. Afr. J. Epidemiol. Infect. 26(4), 225-228 (2011).
- Walle F, Kebede N, Tsegaye A, Kassa T. Seroprevalence and risk factors for Toxoplasmosis in HIV infected and non-infected individuals in Bahir Dar, Northwest Ethiopia. Parasit. Vectors. 6(1), 15 (2013).
- Swai ES, Schoonman L. Seroprevalence of Toxoplasma gondii infection amongst residents of tanga district in north-east Tanzania. Tanzan. J. Health Res. 11(4), 205-209 (2009).
- Ganiem AR, Dian S, Indriati A, et al. Cerebral toxoplasmosis mimicking subacute meningitis in HIV-infected patients; a cohort study from Indonesia. PLoS Negl. Trop. Dis. 7(1), e1994 (2013).
- Montoya JG, Remington JS. Toxoplasma gondii. In Principles and practice of infectious diseases. 5th edition. Edited by Mandell GE, Beneth JE, Dolin R. Odon: Churchill Livingstone. 2858-2888 (2000).
- Arab-Mazar Z, Zamanian MH, Yadegarynia D. Cerebral toxoplasmosis in an HIV-Negative patient: A Case report. Arch. Clin. Infect. Dis. 11(1), e30759 (2016).