Research Article - Neuropsychiatry (2018) Volume 8, Issue 6
Chinese Version of Groningen Frailty Index: Validation in a Chinese Elderly Population
Ray-Ling Luh1,2, Shu Yu1,* and Cheng-Hung Yang3,4
1School of Nursing, National Yang-Ming University, Taipei, Taiwan
2Department of Nursing, Taipei Veterans General Hospital, Taipei, Taiwan
3Assistant Professor, Division of Psychiatry, School of Medicine, National Yang-Ming University, Taipei, Taiwan
4Chief of Geriatric Psychiatry, Department of Psychiatry, Taipei Veterans General Hospital, Taipei, Taiwan
- *Corresponding Author:
- Shu Yu, Professor and Dean
School of Nursing, National Yang-Ming University, No. 155, Sec. 2, Li-Nong St., Peitou, Taipei 11221, Taiwan
Tel: +886-2-28267174
Fax: +886-2-28229973
Abstract
Objective
Early recognition and assessment of frailty status in elderly is essential for clinical treatment. The standard frailty assessment tools normally include a comprehensive but timeconsuming geriatric assessment requiring special training. We translated the Groningen Frailty Indicator (GFI), a 15-item frailty screening tool, into Chinese language and validated the translated version.
Methods
The English version GFI was translated into Chinese following the Brislin’s forward and backward translation model, and validated in a group of community-dwelling elderly. Content validity index (CVI), confirmatory factor analysis (CFA) and exploratory factor analysis (EFA) were used to evaluate the content validity and construct validity, respectively. A total of 331 participants were recruited for construct validity and 54 of them were interviewed twice for the use of test-retest reliability. All statistical analyses were calculated using SPSS 18.0 for Windows.
Results
The Chinese GFI demonstrated excellent test-retest reliability. The I-CVI values ranged from 0.83 to 1.0, and the S-CVI was 0.98. The EFA yielded a 4-factor structure and subsequent CFA results were satisfactory. Individual linear regressions showed that gender, age and marital status were associated with frailty.
Conclusion
The Chinese GFI is a valid and specific screening tool for frailty in Chinese population. A priority of preventive care in very old subjects is recommended with distinguished strategies in different genders according to our findings. Further investigation of possible reasons of lower frailty prevalence in Chinese population and necessity of additional items to increase sensitivity of the tool are warranted.
Keywords
Aging, Geriatrics, Psychometrics, Validation
Introduction
Aging is a natural biological process over the course of life. In this process, functional capacity declines gradually and easily resulted in a variety of clinical conditions. A few concepts have been used to describe the health conditions generally seen in aging adults, e.g., comorbidity or multiple chronic conditions, and disability. These terms are not sufficient to describe the whole health picture of aging adults. Fried et al. [1] proposed a comprehensive concept-frailty, as substitute for the conceptually restricted terms. Frailty has been conceived as a state of vulnerability for adverse health outcomes, including disability, dependency, falls, need for long-term care, and mortality, which are clinically meaningful as an overall description for the elderly. Although the risk of frailty increases with age, it is not an inevitable aging process and may be prevented or treated [2]. As the population ages, early recognition of frailty becomes increasingly important.
Screening and early identification of potential frailty conditions are important for proactive primary care for elderly. Such screening tool should include multiple frailty domains and easy to use. However, most of these tools are impractical for bedside or community screening which normally include a comprehensive geriatric assessment requiring special training and also, time-consuming. This research aimed to translate and adapt a frailty screening tool to be used on Taiwan subjects so that Taiwan data may be compared with previous findings or to be used for international collaboration. The Groningen Frailty Indicator (GFI), a 15-item frailty screening tool developed by Steverink and colleagues has been used in old age studies on primary and community care [3,4]. It measures the loss of functions and resources in physical (question 1-9), cognitive (question 10), social (question 11-13) and psychological (question 14-15) domains, available in both professional and self-report versions. Most items can be answered with “yes” or “no”; for cognitive and psychosocial items, the option ‘sometimes’ is added. Scores on the GFI range from zero to fifteen. A total score of 4 or higher is considered moderate to severe frailty [5,6]. The feasibility and validity of the self-reported version GFI has been described in European populations, including the Netherlands [6] and Romanian [5]; the multidimensional structure of the self-reported GFI was also examined in the Netherlands [7]. A study by Steverink and colleagues [4] suggested that the GFI is an internally consistent scale with positive indications for construct and clinical validity. The internal consistency reliability (KR20) for the GFI is 0.71. The higher the score, the weaker the elderly, and the finding of a score ≥ 4 was defined as frailty in study [3,4]. It was used in a recent Taiwan study comparing the relationships between questionnaires and important dialysis-related complications [8], however, details related to the validity in Chinese population has not been described. In this study, we translated the professional GFI into Chinese and had the tool validated in an elderly sample. Additionally, we examined the associations of the demographic variables on frailty.
Methods
▪ Study design
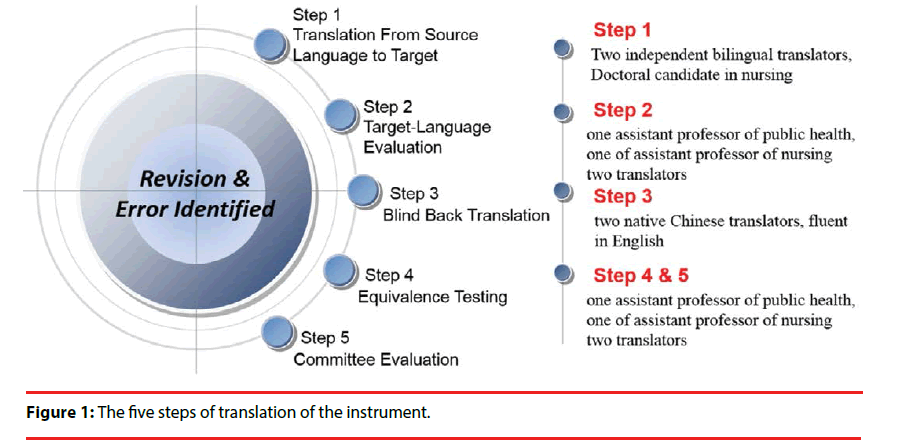
Brislin’s model guided tool preparation in a crosscultural investigation. Brislin [9] introduced the back-translation method, which involves the original document being translated into the target language and then translated back to the original language by a different translator for further content comparison. This well-known method includes translation, back translation, and verification to prepare valid and reliable tools for cross-cultural research [9,10]. Thus, our study consisted two phases: (1) developing the Chinese version GFI by implementing translation and back translation of GFI, and (2) validity and reliability test of the Chinese GFI.
▪ Instruments and translation procedure
• Phase I: Translation and back-translation
(1) Translation from English to Chinese: After obtaining consent from the authors of GFI, the English version was translated into Chinese following the Brislin’s forward and backward translation model (Figure 1) [9,10]. The forward translation was conducted by two bilingual translators competent in both English and Chinese, knowledgeable in geriatrics nursing, instrument development, and Chinese cultures. They translated the source GFI into Chinese independently.
(2) An assistant professor of public health and an assistant professor of nursing, both with bilingual ability, evaluated and compared the translated GFI with the source GFI to identify any incomprehensible or ambiguous phrases and grammatical errors, and substituted the questionable with more culturally and linguistically appropriate words and phrases. Necessary revisions were made after thorough discussion.
(3) Blind back translation: Back-translation of all 15 items into English was conducted by two native Chinese translators proficient in English.
(4) Equivalence testing and committee evaluation of the Chinese GFI: To reduce cultural bias and achieve a better semantic equivalence of the translated GFI [10,11], the 15 items were again reviewed by four bilingual experts [12]. These four experts included of two doctoral candidates in nursing, one assistant professor of public health, and one assistant professor of nursing. The four experts reviewed pairs of items considered nonequivalent in the English and Chinese versions in wording, meaning, grammatical structure, comparability of concepts, and format, and revised on consensus. The Chinese GFI used the same scoring as GFI.
• Phase II: Psychometric examination of the final version
Participants: The Chinese GFI was tested in a group. The participants were communitydwelling elderly in Taipei City selected using purposive sampling method [13]. The inclusion criteria were: (1) aged 65 years or older, (2) non-institutionalized, (3) ambulatory, (4) able to communicate orally or in writing, and (5) available to the author for 10-20 min data collection. Individuals were excluded if they had severe health problems, either physical (e.g., terminal stage cancer) or mental (e.g., schizophrenia), to ensure that the research contents were apprehensible. A total of 331 participants (158 males and 173 females) were conveniently sampled and 54 of them were interviewed twice for test-retest reliability over a 2-week period.
Ethical consideration: This study was approved by the Human Subjects Review Committee of the Institutional Review Board of a Medical Center. The rights and obligations of the participants and their family members were clearly explained, and written consents were obtained from the participants. Confidentiality was maintained during the data collection and data entering procedures.
Statistical analysis: Descriptive statistics were used to illustrate the demographic characteristics and means of items. The internal consistency reliability performed in this study was testretest reliability; the repeated measures over a 2-week period were examined using intraclass correlation coefficient (ICC). The item content validity index (I-CVI) and scale content validity index (S-CVI) were used to evaluate the content validity with a four-point scale ranging from 1 (not relevant) to 4 (highly relevant). Finally, a logistic regression was used to examine the potential contributions of variables on frailty. Quantitative data were analyzed using SPSS 18.0 for Windows (Statistical Package of Social Sciences; SPSS Inc).
Results
▪ Phase I: Translation and backtranslation
• Translation of GFI
The whole translation process emphasized the cross-cultural reliability of Chinese GFI in Taiwanese population. Initially, the two translators’ version of the forward-translated questionnaire used slightly different terms and phrases, but consensus was reached during the group discussion. The back-translated and original version of the GFI were found equivalent by the two English experts, and the back-translated version was also approved by the authors of GFI (letter not shown). All translators approved the draft version Chinese GFI before validity and reliability testing.
▪ Phase II: Psychometric examination of the final version
• Content validity index
We invited six experts including physicians, nursing scholars, and public health researchers to examining the content validity. The experts rated most of the items in the Chinese GFI as highly relevant, leading to an acceptable average. The I-CVI values ranged from 0.83 to 1.0, and the S-CVI was 0.98 (S-CVI/UA = 0.66).
• Construct validity
By using the principle component analysis with varimax rotation, the EFA found component loadings ranged from 0.487 to 0.866, and with item-4 gaining the highest value. The factor loadings of each item are acceptable [14]. Four factors had eigenvalues 1. The first component had an eigenvalue of 4.375 and explained 29.2% of the total variance. A 4-factor structure which accounted for 59.95% of the variance was therefore yielded.
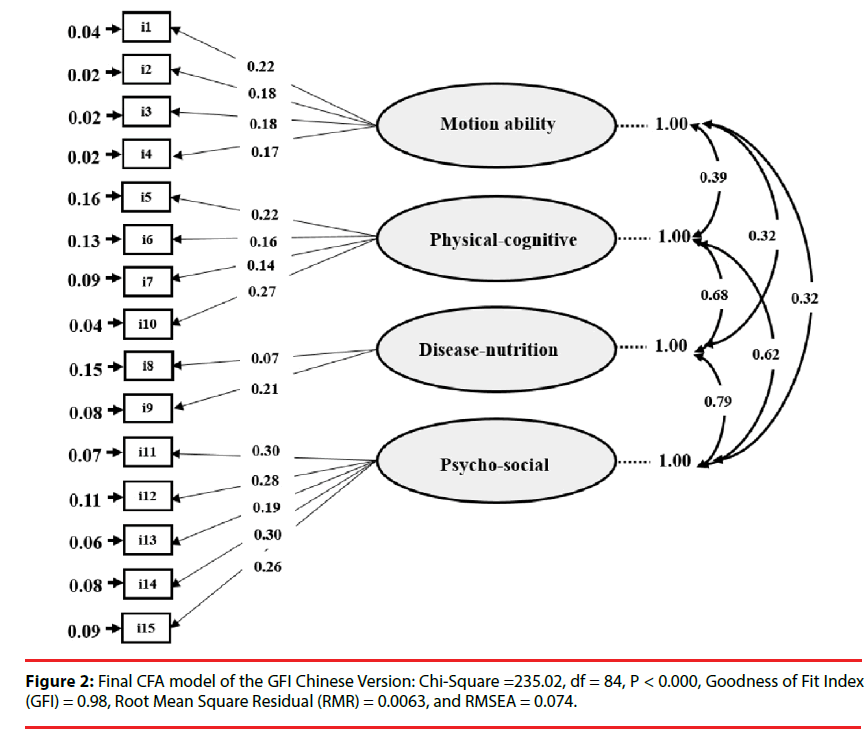
Then we named the first factor (F1) consisting 4 items motion ability (i1, i2, i3, and i4), the second factor (F2) consisting 4 items physicalcognitive (i5, i6, i7 and i10), the third factor (F3) consisting 2 items disease-nutrition (i8, and i9), and the fourth factor (F4) consisting 5 items psycho-social (i11, i12, i13, i14 and i15).
Then, we conducted a CFA to confirm the factor structure and to determine the goodness of fit. The 4-factor model analysis yielded satisfactory results, with a χ2-value of 235.02 (df = 84, p <0.0001), goodness of fit index of 0.98, root mean squared residual of 0.0063, and RMSEA of 0.074 (Figure 2).
Figure 2: Final CFA model of the GFI Chinese Version: Chi-Square =235.02, df = 84, P < 0.000, Goodness of Fit Index (GFI) = 0.98, Root Mean Square Residual (RMR) = 0.0063, and RMSEA = 0.074.
• Test-retest reliability by intraclass correlation coefficient
The results of test-retest reliability of the Chinese GFI over 2-week period are summarized in Table 1. The ICC of the total scale was 0.95; the ICCs of physical, cognitive, social and psychological domains ranged from 0.89 (psychological domain) to 0.96 (physical domain). ICCs of ≤ 0.40, 0.41-0.60, 0.61-0.80, and 0.81-1.00 have been designated as poor to fair agreement, moderate agreement, good agreement, and excellent agreement between the same repeated tests, respectively [15,16]. The ICCs of each domain of Chinese GFI ranged between 0.89 and 0.96, and thus support an excellent testretest reliability (internal consistency reliability).
| Domain | Number of items | ICC |
|---|---|---|
| Motion ability | 4 | 0.97 |
| Physical-cognitive | 4 | 0.92 |
| Disease-nutrition | 2 | 0.91 |
| Psycho-social | 5 | 0.90 |
| Total score | 15 | 0.95 |
Agreement as determined by intraclass correlation coefficient (ICC). ICC ≤ 0.40, poor to fair agreement; 0.41-0.60, moderate agreement; 0.61-0.80, good agreement; and 0.81-1.00, excellent agreement
Table 1: The intraclass correlation coefficients of test-retest reliability of 4 domains and total score of Chinese Groningen Frailty Indicator (N = 54).
• Demographic characteristics of the participants
The age of the participants ranged from 65 to 99 years, with a mean of 73.7 ± 7.2. Among the participants, 74.3% were married (n = 246), 24.2% (n = 80) were single, and 1.5% (n = 5) were non-married. Most of the participants lived with family members, including 26.6% (n = 88) who lived with spouse and 56.5% (n = 187) who lived in three-generation family (living with spouse, children and grandchildren).
• Mean, minimum score, maximum score and sum of Chinese GFI
The mean, minimum score, maximum score and sum of Chinese GFI are summarized in Table 2. The mean score of GFI of all participants was 2.35±2.78. Fitness represents the most common problem in the elderly. The second most common problem reported was disease comorbidity and the least reported problem was weight loss.
| Item | Mean ± SD | Minimum | Maximum | Sum |
|---|---|---|---|---|
| Total | 2.35 ± 2.78 | 0 | 13 | 779 |
| Motion ability | ||||
| Shopping | 0.094 ± 0.292 | 0 | 1 | 31 |
| Walking | 0.060 ± 0.239 | 0 | 1 | 20 |
| Dressing | 0.054 ± 0.227 | 0 | 1 | 18 |
| Toileting | 0.051 ± 0.221 | 0 | 1 | 17 |
| Physical-cognitive | ||||
| Fitness | 0.308 ± 0.462 | 0 | 1 | 102 |
| Vision | 0.193 ± 0.396 | 0 | 1 | 64 |
| Hearing | 0.124 ± 0.330 | 0 | 1 | 41 |
| Cognitive | 0.193 ± 0.396 | 0 | 1 | 64 |
| Disease-nutrition | ||||
| Weight loss | 0.048 ± 0.215 | 0 | 1 | 16 |
| Comorbidity | 0.254 ± 0.436 | 0 | 1 | 84 |
| Psycho-social | ||||
| Memory | 0.193 ± 0.396 | 0 | 1 | 64 |
| Emptiness | 0.202 ± 0.402 | 0 | 1 | 67 |
| Missing someone | 0.251 ± 0.434 | 0 | 1 | 83 |
| Feel abandoned | 0.109 ± 0.312 | 0 | 1 | 36 |
| Depressed mood | 0.224 ± 0.417 | 0 | 1 | 74 |
| Anxious | 0.187 ± 0.391 | 0 | 1 | 62 |
Table 2: Mean ± standard deviation (Mean ± SD) of the 15 items in Chinese GFI (n = 331).
Results of subgroup comparisons by individual linear regressions and χ2-tests are summarized in Table 3. In terms of frailty status, 28.4% (n = 94) of the participants had a Chinese GFI score ≥ 4; the proportion of frailty subjects was significantly higher in males as compared to females (35.8% versus 20.3%, p = 0.0017). There were more frailty subjects in older subjects (p = 0.0132), especially among those at age 80 or older (42.5%). No significant difference was observed in marital status (p = 0.1946) or family bonding (p = 0.9895). One interesting pointed worth mentioning is that none of the subjects admitted a clear widower, separated or divorced status. Thus, “singlehood” was used to describe those who mentioned that there were married but alone at the research period. The results of linear regression for demographic variables in which the total score of Chinese GFI was used as dependent variable were similar to those of Pearson’s χ2-tests, except for marital status (p = 0.0146). The mean total score of Chinese GFI was highest in single participants, followed by married and unmarried participants.
| Variables | N (%) | Chinese GFI Mean ± SD |
P-valueLR | Non-frailty N (%) |
Frailty N (%) |
P-valuePearson’s |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 158 (47.7) | 1.75 ± 2.41 | 0.0002* | 126 (79.7) | 32 (20.3) | 0.0017* |
| Male | 173 (52.3) | 2.90 ± 2.99 | 111 (64.2) | 62 (35.8) | ||
| Age (years) | ||||||
| 65–69 | 113 (34.1) | 1.59 ± 2.23 | 0.0001* | 90 (79.6) | 23 (20.4) | 0.0132* |
| 70–74 | 91 (27.5) | 2.46 ± 2.91 | 66 (72.5) | 25 (27.5) | ||
| 75–79 | 54 (16.3) | 2.26 ± 2.61 | 39 (72.2) | 15 (27.8) | ||
| ³ 80 | 73 (22.1) | 3.47 ± 3.16 | 42 (57.5) | 31 (42.5) | ||
| Marital status | ||||||
| Married | 246 (74.3) | 2.16 ± 2.67 | 0.0146* | 179 (72.8) | 67 (27.2) | 0.1946 |
| Singlehood | 80 (24.2) | 3.06 ± 3.04 | 53 (66.3) | 27 (33.7) | ||
| Unmarried | 5 (1.5) | 0.60 ± 1.34 | 5 (100.0) | 0 (0) | ||
| Family bonding | ||||||
| Live alone | 27 (8.21) | 2.78 ± 2.97 | 0.772 | 19 (70.4) | 8 (29.6) | 0.9895 |
| Live with spouse | 88 (26.6) | 2.31 ± 2.77 | 62 (70.5) | 26 (29.5) | ||
| Three generations | 187 (56.5) | 2.37 ± 2.83 | 135 (72.2) | 52 (27.8) | ||
| Others | 29 (8.8) | 2.00 ± 2.35 | 21 (72.4) | 8 (27.6) |
Frailty was defined when the total score of Chinese Groningen Frailty Indicator ³ 4
Three generations: live with spouse, children or grandchildren.
LR: Linear regression.
Pearson’s: Pearson’s c2-test
*: significant p value
Table 3: Number, mean ± standard deviation (mean ± SD), and results of individual tests.
Discussion
In our study, the findings revealed that the Chinese GFI demonstrated a satisfactory validity and reliability for evaluating the frailty of the elderly in Taiwan. The 15-item four-factor C-GFI was determined to be reliable through both EFA and CFA.
In this study, a liner regression analysis revealed that frailty was associated with age, gender, and marital status. The findings for age and gender are in accordance with those reported in previous GFI studies.
Frailty was associated with both age and gender in individual linear regressions. These findings are in accordance with those reported in previous GFI studies [17].
A common answer given by the married subjects declaring singlehood was “my spouse is not here anymore” and no further explanations were provided. For ethnic reasons, we did not pursue a definite answer after a simple attempt to clarify the answer. Marital status affects health and frailty status. For example, A populationbased cross-sectional study in Columbia found that widowhood in men was associated with poorer self-rated health than married men, while other marital status (single/separated/divorced) was associated with better self-rated health in women [18]; Garre-Olmo et al. [19] found that widowhood a risk of social frailty in a Spanish elderly cohort. In a GFI study investigating 1549 elderly patients in a Dutch primary care center, being widowed or divorced was also found an independent predictor of frailty status [20]. From the ambiguousness of the answer, it is not difficult to figure out that discussion on widower, separated or divorced status might have been viewed as an interdiction among the elderly. Understanding of the cultural taboo may unravel important social factors in frailty.
There are three major limitations in this study. First, physical and psychiatric comorbidity that may affect frailty status of the research subjects, were not evaluated. For example, obesity in the later life, has been consistently shown to contribute to frailty [21]. These diseases may be more prevalent in specific subgroups and confound the statistical analysis. Second, our sample size was rather small. This restricts further stratified analysis of discriminant validity in elderly subgroups. Third, the research subjects were not randomly selected from community.
Previous studies in Taiwan have reported lower frailty prevalence rates as compared with our findings. Lin et al. [22] conducted populationbased cross-sectional study of frailty in a sample consisting 1009 valid subjects aged 65 and older from eight administrative neighborhoods in Taichung City, Taiwan. The Fried’s 5 components criteria [1] (i.e., unintended weight loss, weakness, poor endurance and energy, slowness, and low physical activity level) were used to define frailty with modification on weight loss. The overall prevalence of frailty reported was 13.8%. Li et al. [23] examined a community sample of 903 elderly persons ( ≥ 65 years) in middle Taiwan and reported 11.8% of frail subjects and 47.4% of prefrail subjects using the 5 components criteria [24]. Chang et al. [25] conducted a telephone screening on 2900 subjects randomly selected from a Northern Taiwan Community with the Chinese Canadian Study of Health and Aging Clinical Frailty Scale (CCSHA-CFS) and found an approximate 11.0% of frailty subjects in the sample. Further assessments on a subset of 275 subjects of the sample revealed a prevalence of frailty of 11.3% (95% CI = 7.6–15.0) by Fried’s components and 14.9% (95% CI= 10.7–19.1) by Edmonton Frail Scale (EFS). The frailty prevalence rates reported in these Taiwan studies were much lower than those of Western countries which ranged from 32% to 59% [26-28]. Although Fried’s definitions were used in the Taiwan studies at some point, the assessment approaches and criteria of the definitions varied. Nevertheless, the difference of social structure and elderly characteristics between Eastern and Western world may also contribute the difference prevalence. Like many translated assessment tools, additional items may be required to increase the sensitivity of the Chinese GFI. Further investigations should be conducted before drawing a conclusion.
Inputs from medical professionals are important in the development of an assessment tool and their perceptions on relevance influence its applications. Five or more experts are recommended to calculate the CVI [29]. In this study, we included six experts for this purpose. The experts rated most of the items in the Chinese GFI highly relevant, leading to an acceptable average S-CVI score of 0.94, which is comparable to results from other content validation studies [30].
Conclusion
The present study examined the factorial validity, content validity, and internal consistency reliability of the Chinese GFI. The results confirm that the Chinese GFI was a valid and reliable instrument and an appropriate for assessing the frailty in Chinese population. A priority of preventive care in very old subjects is recommended with distinguished strategies in different genders according to the statistical findings of the sample. Given the potential characteristic differences between different elderly populations and undetected frailty features in Chinese population, further study in randomly selected elderly subjects from community and evaluation of additional frailty items are warranted.
Acknowledgments
The authors would like to express thank to all the participants who contributed to the study. Gratitude also goes to Dr. Nardi Steverink who agrees me to use his GFI Chinese translation for my study.
References
- Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty and comorbidity: implications for improved targeting and care. J. Gerontol. A Biol. Sci. Med. Sci 59(1), 255-263 (2004).
- Ahmed N, Mandel R, Fain MJ. Frailty an emerging geriatric syndrome. Am. J. Med 120(1), 748-753 (2007).
- Schuurmans H, Steverink N, Lindenberg S, et al. Old or frail: what tells us more? J. Gerontol. A Biol. Sci. Med. Sci 59(A), 962-965 (2004).
- Steverink N, Slaets JPJ, Schuurmans H, et al. Measuring frailty: developing and testing the GFI (Groningen Frailty Indicator). Gerontologist 41(1), 236-237 (2001).
- Olaroiu M, Ghinescu M, Naumov V, et al. The psychometric qualities of the Groningen Frailty Indicator in Romanian community-dwelling old citizens. Fam. Pract 31(1), 490-495 (2014).
- Peters LL, Boter H, Buskens E, et al. Measurement properties of the Groningen Frailty Indicator in home-dwelling and institutionalized elderly people. J. Am. Med. Dir. Assoc 13(1), 546-551 (2012).
- Bielderman A, van der Schans CP, van Lieshout MR, et al. Multidimensional structure of the Groningen Frailty Indicator in community-dwelling older people. BMC. Geriatr 13(1), 1-9 (2013).
- Chao CT, Hsu YH, Chang PY, et al.Simple self-report FRAIL scale might be more closely associated with dialysis complications than other frailty screening instruments in rural chronic dialysis patients. Nephrology 20(1), 321-328 (2015).
- Brislin RW. Back-translation for crosscultural research. J. Cross-Cult. Psychol 1(1), 185-216 (1970).
- Brislin RW. The wording and translation of research instrument. In: WJ Lonner, JW Berry (Eds.), Field Methods in Cross-Cultural Research Newbury Park, CA: Sage Publications, USA (1986).
- Grant JS, Davis LL. Selection and use of content experts for instrument development. Res. Nurs. Health 20(1), 269-274 (1997).
- Herdman M, Fox-Rushby J, Badia X. A model of equivalence in the cultural adaptation of HRQoL instruments: the Universalist approach. Qual. Life. Res 7(1), 323-335 (1998).
- Silverman D. Doing Qualitative Research: A Practical Handbook. Thousand Oaks, CA: Sage Publications, USA (2001).
- Hair JF, Black B, Babin B, et al. Multivariate Data Analysis. New York (1992).
- Fayers PM, Machin D. Quality of Life: Assessment, Analysis and Interpretation. Wiley, New York (2000).
- Wilson KA, Dowling AJ, Abdolell M, et al. Perception of quality of life by patients, partners and treating physicians. Qual. Life. Res 9(1), 1041-1052 (2000).
- Peters LL, Boter H, Burgerhof JG, et al. Construct validity of the Groningen Frailty Indicator established in a large sample of home-dwelling elderly persons: evidence of stability across age and gender. Exp. Gerontol 69(1), 129-141 (2015).
- Ocampo-Chaparro JM, Zapata-Ossa HJ, Cubides-Munévar AM, et al. Prevalence of poor self-rated health and associated risk factors among older adults in Cali, Colombia. Colombia. Med. (Cali) 44(1), 224-231 (2013).
- Garre-Olmo J, Calvó-Perxas L, López-Pousa S, et al. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age. Ageing 42(1), 46-51 (2013).
- Drubbel I, Bleijenberg N, Kranenburg G, et al.Identifying frailty: do the Frailty Index and Groningen Frailty Indicator cover different clinical perspectives? A cross-sectional study. BMC. Fam. Pract 14(1), 1-8 (2013).
- Porter Starr KN, McDonald SR, Bales CW. Obesity and physical frailty in older adults: a scoping review of lifestyle intervention trials. J. Am. Med. Dir. Assoc 15(1), 240-250 (2014).
- Lin CC, Li CI, Meng NH, et al. Frailty and its associated factors in an elderly Taiwanese metropolitan population. J. Am. Geriatr. Soc 61(1), 292-294 (2013).
- Li CI, Lin CH, Lin WY, et al.Successful aging defined by health-related quality of life and its determinants in community-dwelling elders. BMC. Public. Health 14(1), 1-8 (2014).
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci 56(A), 146-156 (2001).
- Chang CI, Chan DC, Kuo KN, et al. Prevalence and correlates of geriatric frailty in a northern Taiwan community. J. Formos. Med. Assoc 110(1), 247-257 (2011).
- Daniels R, Metzelthin S, van Rossum E, et al. Interventions to prevent disability in frail community-dwelling older persons: an overview. Eur. J. Ageing 7(1), 137-155 (2010).
- Levers MJ, Estabrooks CA, Ross Kerr JC. Factors contributing to frailty: literature review. J. Adv. Nurs 56(1), 282-291 (2006).
- Slaets JPJ. Vulnerability in the elderly: frailty. Med. Clin. N. Am 90(1), 593-601 (2006).
- Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 29(1), 489-497 (2006).
- Larsson H, Tegern M, Monnier A, et al. Content validity index and intraand inter-rater reliability of a new muscle strength/endurance test battery for Swedish soldiers. PLoS. One 10(1), e0132185 (2015).