Research Article - Interventional Cardiology (2021)
Chronic obstructive pulmonary disease is associated with increased mortality in patients undergoing MitraClip therapy: A systematic review and meta-analysis
- Corresponding Author:
- Chanavuth Kanitsoraphan
Department of Medicine, University of Hawaii Internal Medicine Residency Program,Honolulu, HI,USA,
E-mail: chanavuth.kan@gmail.com
Received date: April 28, 202; Accepted date: May 12, 2021;Published date: May 19, 2021
Abstract
Introduction: Chronic Obstructive Pulmonary Disease (COPD) is highly prevalent in patients undergoing MitraClip with up to 39% reported. Nonetheless, whether COPD has effect on mortality in this patient population remains unclear. We conduct a systematic review and meta-analysis to evaluate the effect of COPD on the outcome in patient undergoing MitraClip therapy.
Methods: We comprehensively searched the data bases of MEDLINE and EMBASE from inception to August 2020. Published cohort and randomized controlled trials of patients undergoing MitraClip therapy which reported univariate or multivariate analyses on the effect of COPD to mortality were included. Data were integrated using the random-effects, generic inverse variance method of DerSimonian and Laird.
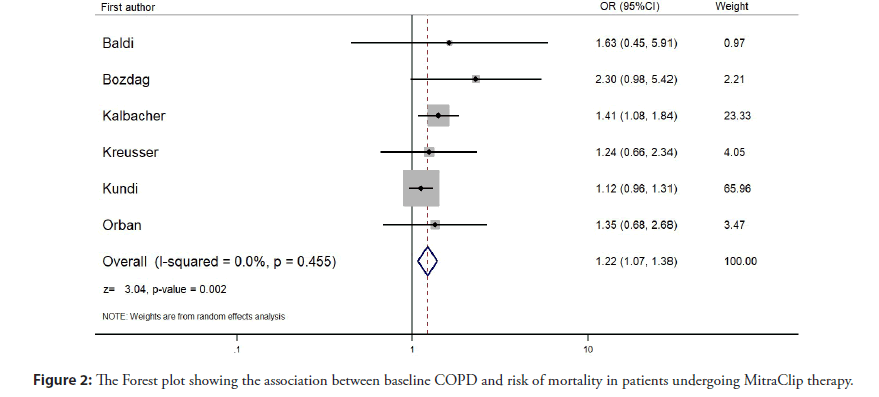
Results: Six studies from 2014-2018 involving 5,076 patients undergoing MitraClip therapy were included. Baseline COPD was associated with increased mortality (Risk Ratio [RR]=1.22, 95% Confidence Interval [CI]: 1.07-1.38, p=0.002, I2=0.00%).
Conclusion: COPD is associated with increased mortality in patient undergoing MitraClip therapy up to 1.22 folds. Therefore, COPD could be a predictor of outcome in patients undergoing Mitraclip therapy and could be potentially integrated in risk stratification in this patient population.
Keywords
Percutaneous mitral valve repair • MitraClip • Chronic obstructive pulmonary disease • Mortality
Abbreviations
COPD: Chronic Obstructive Pulmonary Disease; FEV: Forced Expiratory Volume; HF: Heart Failure; HR: Hazard Ratio; LVEF: Left Ventricular Ejection Fraction; MR: Mitral Regurgitation; NOS: The Newcastle-Ottawa Quality Assessment Scale; OR: Odds Ratio; PFT: Pulmonary Function Test; PMVR: Percutaneous Mitral Valve Repair; RR: Relative Risk; TAVR: Transcatheter Aortic Valve Replacement.
Introduction
Secondary Mitral Regurgitation (MR) due to left ventricular dilation, or functional MR, is widely known to be associated with a worse outcome regarding rehospitalization and mortality in Heart Failure (HF) patients [1]. The geometric dislocation of the papillary muscles and chordae tendineae lead to an incomplete closure of the mitral leaflets causing MR [1]. Guideline-directed medical therapy has been the cornerstone treatment to reduce symptoms, improve Left Ventricular Ejection Function (LVEF), which then decrease the severity of MR [2]. However, in patients who failed medical treatment or with significant LV chamber distortion, surgical options are necessary [3,4]. Percutaneous Mitral Valve Repair (PMVR) with MitraClip has emerged as a relatively safe therapeutic option for patients with prohibitively high surgical risks [5-9]. The COAPT trial demonstrated that MitraClip therapy in patients with moderate-to-severe or severe functional MR secondary to heart failure who failed guideline-directed medical therapy had a lower rate of hospitalization for heart failure and lower all-cause mortality at 2 years follow-up [10]. However, despite a promising result of MitraClip, there are several factors that should be taken into consideration in selecting appropriate patients to undergo the intervention [11]. A thorough risk assessment can help physicians select patients who will likely benefit from the procedure and will help in making a shared decision with patients. This includes procedural tolerability, severity of MR, degree of LV dilatation, comorbidities and life expectancy.
Chronic Obstructive Pulmonary Disease (COPD) is long known to have a close relationship with cardiovascular disease, including HF, and is associated with worse prognosis when the two diseases combine [12,13]. Common risk factors are shared between COPD and cardiovascular diseases (i.e., smoking, elderly), and several features of COPD can predispose patients to cardiovascular diseases (i.e., abnormal gas exchange, chronic inflammation, sedentary lifestyle) [14]. There is currently limited data regarding the association between COPD and outcome in patients with severe MR undergoing MitraClip therapy. Thus, we aimed to evaluate this association via systematic review and meta-analysis.
Methodology
Search strategy
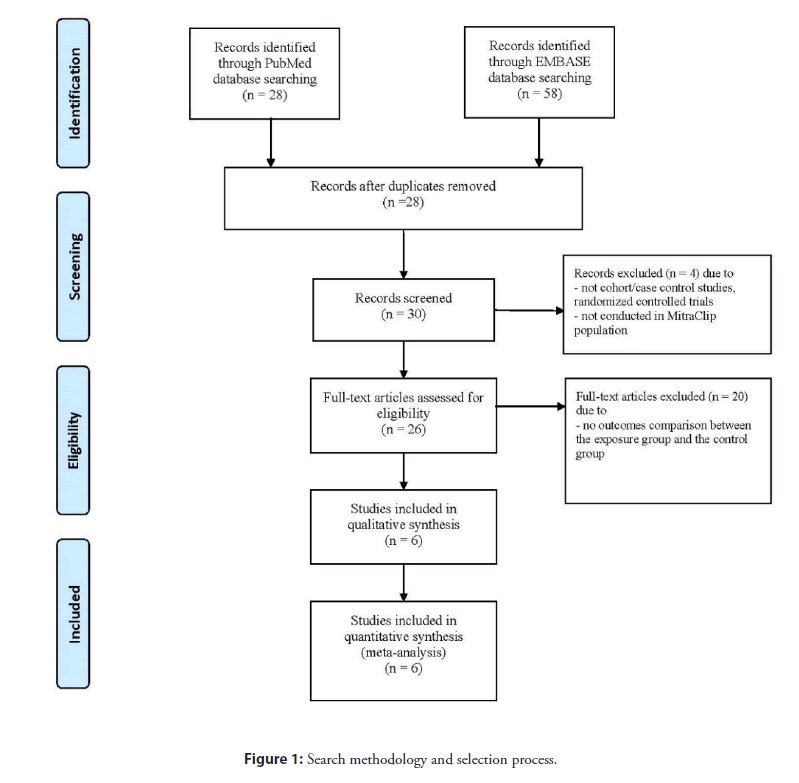
Two investigators (JK and CT) independently searched for published studies indexed in MEDLINE and EMBASE databases from inception to August 2020 using a search strategy that including the terms “percutaneous mitral valve repair”, “chronic obstructive pulmonary disease” as described in Figure 1. Only full articles in English were included. A manual search for additional pertinent studies and review articles using references from retrieved articles was also completed.
Inclusion criteria
The eligibility criteria included the following:
• Cohort studies (prospective or retrospective), case-control studies, cross-sectional studies, randomized control trials reporting
• Relative Risk (RR), Odds Ratio (OR), Hazard Ratio (HR) or adjusted hazard ratio with 95% Confidence Interval (CI) or sufficient raw data for the calculation were provided. Patients without COPD were used as controls.
Two investigators (JK and CT) independently determined study eligibility and discussed to reach mutual consensus should there were discrepancies. The Newcastle-Ottawa Quality Assessment Scale (NOS) was used to assess each study’s quality in three domains, recruitment and selection of the participants, similarity and comparability between the groups, and ascertainment of the outcome of interest among cohort and case-control studies [15].
Data extraction
A standardized data collection form was used to obtain the following information from each study: name of first author, year of publication, country of origin, study design, study population, total population, type of MR, median follow-up time, surgical risk profile, participants demographic, and confounders that were adjusted in the multivariable analysis, if available.
Two investigators (JK and CT) independently performed this data extraction process to ensure accurate data extraction. Any data discrepancy was resolved by reviewing the primary data from the original articles.
Definition
Mortality defined was all-cause mortality, both short-term and long-term, following MitraClip therapy.
Statistical analysis
Randon-effects model was used to perform meta-analysis of included studies. We pooled the point estimates of risk ratio and rate ratio from each study by using the generic inverse-variance method of Der Simonian and Laird [16]. The I2 statistic, which ranges from 0% to 100% (I2<25%, low heterogeneity; I2=25%-50%, moderate heterogeneity; and I2>50%, substantial heterogeneity) was used to quantify the heterogeneity of effect size estimates across the studies [17]. A sensitivity analysis was performed to assess the influence of the individual studies on the overall results by omitting one study at a time. Publication bias was assessed using a funnel plot and the Egger’s regression test [18]. All data analyses were performed using the STATA SE version 14.2.
Sensitivity analysis
We used a sequential exclusion strategy to examine whether overall estimates were influenced by the substantial heterogeneity among studies [19]. We sequentially and cumulatively excluded studies that accounted for the largest share of heterogeneity until I2 was less than 50%. We then examined whether RR estimates were consistent.
Results
Search results
Our search strategy yielded 58 potentially relevant articles (58 articles from EMBASE and 28 articles from MEDLINE). After the exclusion of 28 duplicated articles, 30 articles underwent title and abstract review. Four articles were excluded at this stage since they were not cohort/case control studies, randomized controlled trials or were not conducted in MitraClip population, or topics. Remaining 16 articles underwent full-length review. Ten articles were excluded at this stage as there were no comparing outcomes between the exposure group and the control group. Finally, a total of 6 studies were included in this meta-analysis. Figure 1 reveals the search and literature review process.
Description of included studies
A total of 6 studies from 2014 to 2020 were included in our meta- analysis with a total of 5,076 patients who underwent MitraClip therapy. Median follow-up duration ranged from 12 to 43 months, mean age ranged from 71.6 to 79.4 years old. Female gender represented 20.6% to 27.4% of the study participants. Table 1 demonstrates characteristics of all included studies.
| First author, year | Country | Study design | Study population | Total population (n)+ | Type of MR | Median follow-up duration (Months) | COPD (%) | Mean age (years) | Male (%) | Mean LVEF (%) | Mortality at follow-up (%) | STS score | Euroscore II | Adjusting factors |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baldi, 2018 | Italy | Prospective cohort | Symptomatic moderate-to-severe or severe MR | 74 | Functional MR | 13.9 | 39.2 | 71.6 ± 8.3 | 78.4 | 33.2 ± 6.8 | 35.10% | N/A | 6.1 | N/A |
| Bozdag-Turan, 2014 | Germany | Prospective cohort | Severe MR (at least grade 3+) | 121 | Primary MR and Secondary MR | 12 | 28.1 | 77 ± 7 | 57 | 42 ± 16 | 23.10% | 10.9 ± 6.4 | 10.6 ± 5.6 | EuroSCORE II, STS score, mTPG, mVOA, LVEF<=30, MR grade after MitraClip |
| Kalbacher, 2018 | Germany | Prospective cohort | Severe MR | 799 | Functional MR (69.3%) | 34.5 | 21.9 | 75.3 ± 8.6 | 60.7 | N/A | 45.70% | 8.5 ± 7.5 | Logistic EuroSCORE 23.7 ± 16.0 | Gender, Prior cardiac decompensation, Previous aortic valve intervention, Renal function, Severe TR, LVEF<30% |
| Kreusser, 2018 | Germany | Prospective cohort | Symptomatic moderate-to-severe or severe MR with reduced EF | 174 | Functional MR | 12 | 19 | 75.2 | 69.5 | 25 | 17.80% | 14.7 | 5.7 | N/A |
| Kundi, 2018 | United States | Retrospective cohort | Patients who had undergone MitraClip procedures | 3782 | N/A | 13.6 | 27.1 | 79.4 ± 9.3 | 55.2 | N/A | 29.50% | N/A | N/A | Age, CHF, AF, Gender, History of valvular surgery, Non-cardiac history, Presentation characteristics, Nontraditional risk factors |
| Orban, 2017 | Germany | Prospective cohort | Severe symptomatic MR | 126 | Primary MR and Secondary MR | 43 | 18.3 | 72.6 ± 10.6 | 62.7 | 48.4 ± 15.6 | 35.70% | 14.0 ± 15.5 | Logistic EuroSCORE 19.1 ± 20.0 | LVEF, TR severity, Renal function, Post-procedural MR severity |
Abbreviations: COPD: Chronic Obstructive Pulmonary Disease; EF: Ejection Fraction; MR: Mitral Regurgigation; MVOA: Mitral Valve Orifice Area; mTPG: mean Transmitral Pressure Gradient; TR: Tricuspid Regurgitation; TRAMI: The Multicentre Industry-Independent German Transcatheter Mitral Valve Interventions.
Table 1: Characteristics of included studies.
Quality assessment of included studies
The NOS of included studies are described in the Table 2. The NOS uses a scoring system to evaluate qualities of studies on 3 domains, including selection, comparability, and outcomes.
| First author, year | Selection | Comparability | Outcome | Total score | |||||
|---|---|---|---|---|---|---|---|---|---|
| Represent-ativeness | Selection of the non-exposed cohort | Ascertainment | Endpoint not present at start | Comparability | Assessment of outcome | Follow-up duration | Adequacy follow-up | ||
| (Confounding) | |||||||||
| Baldi, 2018 | * | * | * | * | * | * | * | * | 8 |
| Bozdag-Turan, 2014 | * | * | * | * | ** | * | * | * | 9 |
| Kalbacher, 2018 | * | * | * | * | ** | * | * | * | 9 |
| Kreusser, 2018 | * | * | * | * | * | * | * | * | 8 |
| Kundi, 2018 | * | * | * | * | ** | * | * | * | 9 |
| Orban, 2017 | * | * | * | * | ** | * | * | * | 9 |
Notes: The Newcastle-Ottawa scale uses a star system (0 to 9) to evaluate included studies on 3 domains: Selection, comparability, and outcomes. Star (*)=item presents. Maximum 1 star (*) for selection and outcome components and 2 stars (**) for comparability components. Higher scores represent higher study quality.
Table 2: Newcastle-Ottawa quality assessment scale of included studies in meta-analysis.
Meta-analysis results
We found that baseline COPD is associated with an increased risk of mortality following MitraClip therapy (pooled HR=1.22, 95%CI: 1.07-1.38, I2=0.0%, p=0.002). Forest plot is demonstrated in Figure 1.
Sensitivity analysis
To assess the stability of the results of the meta-analysis, we conducted a sensitivity analysis for each outcome by excluding one study at a time. There were no significant alterations of results for every outcome.
Discussion
Despite a lot of evidence indicating COPD as an independent predictor of mortality in patients undergoing cardiac surgeries or other transcatheter interventions i.e., transcatheter aortic valve replacement [20-24], conflicting data exist regarding its impact on outcomes of patients undergoing MitraClip. There has yet to be a dedicated study on impact of COPD on outcomes of patients undergoing MitraClip procedure. Five out of six studies included in our meta-analysis did not shown statistically significant increase in mortality in patients with COPD undergoing MitraClip therapy. Our study is the first meta-analysis to assess the relation COPD and mortality among patients undergoing MitraClip therapy (Figure 2).
Figure 2: The Forest plot showing the association between baseline COPD and risk of mortality in patients undergoing MitraClip therapy.
Mechanism to explain increased mortality rate in patient with COPD has yet to be elucidated. First, patients with COPD were more likely to have associated cardiovascular, renal, neurologic, infectious, liver, and respiratory comorbidities [25,26]. COPD patients were also more often found to have lower BMI which may be resulted from nutritional deficiency [25]. Protein malnutrition is commonly seen in patients with lower BMI and can cause more pulmonary complications, due to respiratory muscle strength impairment, reduction in diaphragmatic muscular mass, and maximum voluntary ventilation [27]. COPD patients also have gas exchange and mucociliary clearance of aspirated bacteria dysfunction, which predispose patients to postoperative pneumonia and respiratory failure [28,29]. COPD patients were also found to have increased risk of postoperative wound dehiscence [30], sepsis [25], cardiac arrhythmia and myocardial infarction [31], as well as acute kidney injuries [32].
Currently, preoperative surgical risk evaluation for patients undergoing MitraClip is based on Society of Thoracic Surgeons (STS) risk score, with predicted operative mortality of ≥ 8 percent being used as a prohibitive cut-point [6]. However, the STS does not include the presence of COPD in its risk formula. The STS score only utilizes only FEV1 from Pulmonary Function Test (PFT) to define chronic lung disease. In addition to STS score, COPD diagnosis should also be considered separately in risk stratification as well.
Obtaining accurate COPD diagnosis is thus important for pre- operative assessment for patients undergoing MitraClip. COPD many times is diagnosed in clinical practice based on symptoms of dyspnea and history of smoking without confirmation with PFTs [33]. Adabag et al. [34] had shown that preoperative PFTs done in patients undergoing cardiac surgeries in a tertiary cardiac center revealed COPD status of 30% of patients were misclassified, and half of these patients were newly diagnosed with COPD by the these pre-operative PFTs. With accurate diagnosis of COPD, appropriate medical optimization and improvement of pulmonary hygiene can subsequently be done to prevent morbidities and mortalities in these groups of patients, although there is no study of benefits of these interventions in patients undergoing MitraClip thus far.
Limitations
There are a few limitations in our meta-analysis. First, there were minor differences among baseline patient, which are illustrated in Table 1. Secondly, as a nature of cohort studies which are used in the meta-analysis, causal relationship cannot be inferred. Third, all studies were conducted in European countries. Therefore, extrapolation of the results to apply in other ethnicities could be limited. Fourth, despite attempts to adjust with possible confounders in some studies, these confounders were not adjusted identically in all studies and there were potential confounders that remained unadjusted.
Conclusion
COPD is associated with increased mortality in patient undergoing MitraClip therapy up to 1.22 folds. Therefore, COPD could be a predictor of outcome in patients undergoing Mitraclip therapy and could be potentially integrated in risk stratification in this patient population.
Financial Support
None
Acknowledgement
None
Conflict of Interest
None to declare
References
- Asgar AW, Mack MJ, Stone GW. Secondary mitral regurgitation in heart failure: pathophysiology, prognosis, and therapeutic considerations. J Am Coll Cardiol. 65(12): 1231-48 (2015).
- Dwivedi A, Vainrib A, Saric M. Functional mitral regurgitation in patients with heart failure and depressed ejection fraction. Curr Opin Cardiol. 31(5): 483-92 (2016).
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 70(2): 252-89 (2017).
- Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 38(36): 2739-91 (2017).
- Baldus S, Schillinger W, Franzen O, et al. MitraClip therapy in daily clinical practice: initial results from the German transcatheter mitral valve interventions (TRAMI) registry. Eur J Heart Fail. 14(9): 1050-5 (2012).
- Lim DS, Reynolds MR, Feldman T, et al. Improved functional status and quality of life in prohibitive surgical risk patients with degenerative mitral regurgitation after transcatheter mitral valve repair. J Am Coll Cardiol. 64(2):182-92 (2014).
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med. 364(15): 1395-406 (2011).
- Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: Early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe. J Am Coll Cardiol. 62(12): 1052-61 (2013).
- Nickenig G, Estevez-Loureiro R, Franzen O, et al. Percutaneous mitral valve edge-to-edge repair: In-hospital results and 1-year follow-up of 628 patients of the 2011-2012 Pilot European Sentinel Registry. J Am Coll Cardiol. 64(9): 875-84 (2014).
- Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 379(24): 2307-18 (2018).
- Atianzar K, Zhang M, Newhart Z, et al. Why did COAPT win while MITRA-FR failed? Defining the appropriate patient population for MitraClip. Interv Cardiol. 14(1): 45-7 (2019).
- Khanji MY, Stone IS, Boubertakh R, et al. Chronic obstructive pulmonary disease as a predictor of cardiovascular risk: A case-control study. COPD. 17(1): 1-9 (2019).
- Budnevsky AV, Malysh EY. Clinico-Pathogenetic relationship of cardiovascular diseases and chronic obstructive pulmonary disease. Kardiologiia. 57(4): 89-93 (2017).
- Rabinovich RA, MacNee W. Should we treat chronic obstructive pulmonary disease as a cardiovascular disease? Expert Rev Respir Med. 9(4): 459-72 (2015).
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 25(9): 603-5 (2010).
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 7(3): 177-88 (1986).
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 327(7414): 557-60 (2003).
- Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J Clin Epidemiol. 54(10): 1046-55 (2001).
- Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. Int J Epidemiol. 37(5): 1148-57 (2008).
- Simmonds M. Quantifying the risk of error when interpreting funnel plots. Syst Rev. 4: 24 (2015).
- Debray TPA, Moons KGM, Riley RD. Detecting small-study effects and funnel plot asymmetry in meta-analysis of survival data: A comparison of new and existing tests. Res Synth Methods. 9(1): 41-50 (2018).
- Dvir D, Waksman R, Barbash IM, et al. Outcomes of patients with chronic lung disease and severe aortic stenosis treated with transcatheter versus surgical aortic valve replacement or standard therapy: insights from the PARTNER trial (placement of AoRTic TraNscathetER Valve). J Am Coll Cardiol. 63(3): 269-79 (2014).
- Le Jemtel TH, Padeletti M, Jelic S. Diagnostic and therapeutic challenges in patients with coexistent chronic obstructive pulmonary disease and chronic heart failure. J Am Coll Cardiol. 49(2): 171-80 (2007).
- Gunter RL, Kilgo P, Guyton RA, et al. Impact of preoperative chronic lung disease on survival after surgical aortic valve replacement. Ann Thorac Surg. 96(4): 1322-8 (2013).
- Gupta H, Ramanan B, Gupta PK, et al. Impact of COPD on postoperative outcomes: Results from a national database. Chest. 143(6): 1599-606 (2013).
- Corsonello A, Pedone C, Incalzi RA. Comorbidities and risk assessment in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 186(8): 804 (2012).
- Windsor JA, Hill GL. Risk factors for postoperative pneumonia. The importance of protein depletion. Ann Surg. 208(2): 209-14 (1988).
- Gupta PK, Gupta H, Kaushik M, et al. Predictors of pulmonary complications after bariatric surgery. Surg Obes Relat Dis. 8(5): 574-81 (2012).
- Smetana GW, Lawrence VA, Cornell JE, et al. Preoperative pulmonary risk stratification for non-cardiothoracic surgery: Systematic review for the American College of Physicians. Ann Intern Med. 144(8): 581-95 (2006).
- Saleh HZ, Mohan K, Shaw M, et al. Impact of chronic obstructive pulmonary disease severity on surgical outcomes in patients undergoing non-emergent coronary artery bypass grafting. Eur J Cardiothorac Surg. 42(1): 108-13 (2012).
- Bertges DJ, Goodney PP, Zhao Y, et al. The Vascular Study Group of New England Cardiac Risk Index (VSG-CRI) predicts cardiac complications more accurately than the Revised Cardiac Risk Index in vascular surgery patients. J Vasc Surg. 52(3): 674-83 (2010).
- Rodrigues AJ, Evora PR, Bassetto S, et al. Risk factors for acute renal failure after heart surgery. Rev Bras Cir Cardiovasc. 24(4): 441-6 (2009).
- Joish VN, Brady E, Stockdale W, et al. Evaluating diagnosis and treatment patterns of COPD in primary care. Treat Respir Med. 5(4): 283-93 (2006).
- Adabag AS, Wassif HS, Rice K, et al. Preoperative pulmonary function and mortality after cardiac surgery. Am Heart J. 159(4): 691-7 (2010).