Case Report - Imaging in Medicine (2016) Volume 8, Issue 4
Chronic pancreatitis with extra peritoneal fluid collection misleadingly presenting as ascites
AMd Noh MSF*1, Abdul Rashid AM2, Norafida B1, Mohd. Hazeman Z1, Idris I1and Suraini MS11Department of Imaging, Faculty of Medicine and Health Sciences, Universiti Putra, Malaysia
2Department of Medicine, Faculty of Medicine and Health Sciences, Universiti Putra, Malaysia
- *Corresponding Author:
- AMd Noh MSF
Department of Imaging
Faculty of Medicine and Health Sciences
Universiti Putra, Malaysia
E-mail: msf.mdnoh@gmail.com
Abstract
A 30 year old male was admitted to our medical ward with recurrent abdominal distension. He had multiple admissions for therapeutic and diagnostic peritoneal tapping, but culture & cytology came back negative. He was initially treated as alcoholic chronic liver disease (CLD) Child-Pugh B. Despite having recurrent admissions and treated as decompensated alcoholic CLD with spontaneous bacterial peritonitis, his peritoneal fluid cultures were negative and medical therapy for CLD failed to improve symptoms. We proceeded with Computed Tomography Abdomen and showed a large collection of fluid in the extraperitoneum with mild ascites. Subsequently, pigtail catheter was inserted under ultrasound guidance to drain extraperitoneal fluid and biochemistry came back with high amylase level of 9043 U/L and total protein of 1.2 g/dL. As fluid amylase level >1000 U/L, it fulfills the criteria for chronic pancreatitis and he was managed conservatively with continuous fluid drainage. Patient improved gradually.
Introduction
Chronic pancreatitis is an inflammatory condition that causes permanent structural changes with impairment of the endocrine and exocrine functions of the pancreas. Clinical manifestations of this disorder include chronic abdominal pain and pancreatic dysfunction, which may not be clinically evident until a large portion of the pancreas is affected. It is associated with a multitude of complications, most commonly being pseudocyst formation. Rarely, it causes pancreatic ascites or pleural effusion. We report a case of a man who was initially presumed and treated as alcoholic chronic liver disease (CLD) with ascites but eventually confirmed having chronic pancreatitis and fluid in the extraperitoneum.
Clinical presentation
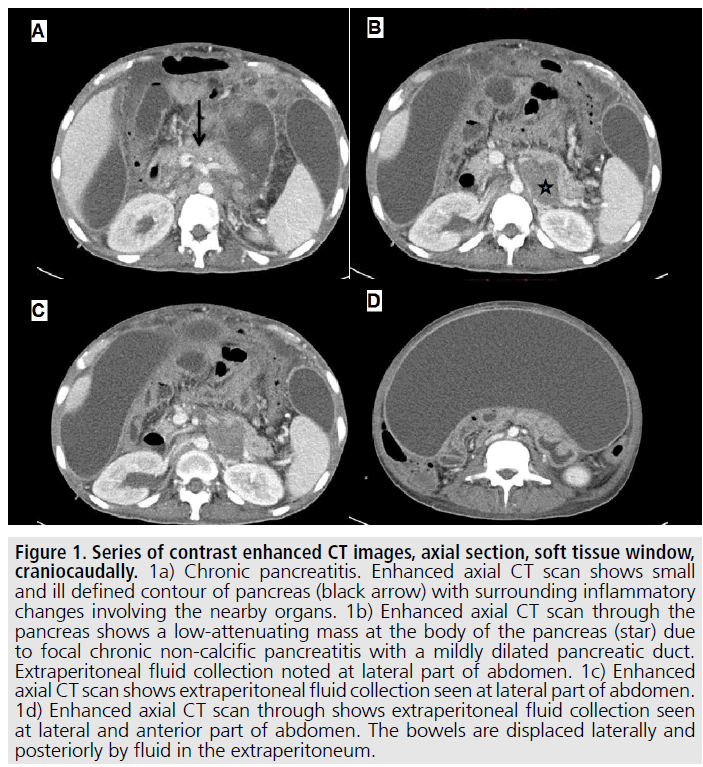
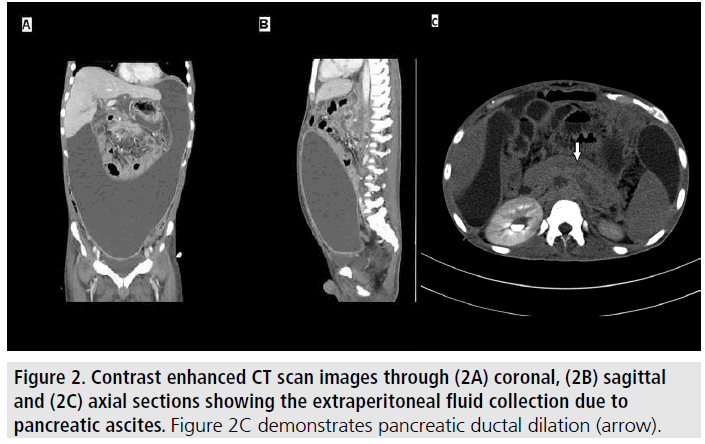
A 30 year old male, with a longstanding history of chronic alcoholic consumption was admitted to our medical ward with recurrent episodes of abdominal distension. He had multiple admissions for which therapeutic and diagnostic peritoneal tapping were done. He was initially treated as alcoholic CLD Child- Pugh B. Despite having recurrent admissions and treated as decompensated alcoholic CLD with spontaneous bacterial peritonitis, his peritoneal fluid cultures and cytology were negative and medical therapy for CLD failed to improve his symptoms. We proceeded with Computed Tomography Abdomen FIGURE 1 and 2 and showed a large collection of fluid in the extraperitoneum with mild ascites. Mild hepatomegaly, with a hypodense lesion at the pancreatic body was present.
Differential diagnosis
Peritonitis
Chronic liver disease with ascites
Hypoalbuminaemia
Pancreatic carcinoma with ascites
Treatment and outcome
Pigtail catheter was inserted under ultrasound guidance to drain extraperitoneal fluid. This revealed thick greenish fluid, mixed with blood. Extraperitoneal fluid was sent for biochemistry and came back with high amylase level of 9043 U/L and total protein of 1.2 g/dL. As fluid amylase level >1000 U/L, it fulfills the criteria for chronic pancreatitis and he was managed conservatively. Continuous fluid drainage was successfully done. Patient underwent a gradual improvement during the admission and initial outpatient appointment. He was scheduled for repeat imaging, but unfortunately was lost to subsequent follow up.
Discussion
Among the complications that may occur in patients with a background of chronic alcoholism with chronic pancreatitis is pancreatic ascites. This may also occur following acute pancreatitis or trauma to the pancreas [1]. To our knowledge, in Malaysia, there is no local data citing the prevalence of this particular complication in patients with pancreatitis (acute or chronic), or following pancreatic trauma. Men are affected more than women with a ratio of 2:1 and affected patients are between the age group of 20 to 50 years old [2].
Figure 1. Series of contrast enhanced CT images, axial section, soft tissue window, craniocaudally. 1a) Chronic pancreatitis. Enhanced axial CT scan shows small and ill defined contour of pancreas (black arrow) with surrounding inflammatory changes involving the nearby organs. 1b) Enhanced axial CT scan through the pancreas shows a low-attenuating mass at the body of the pancreas (star) due to focal chronic non-calcific pancreatitis with a mildly dilated pancreatic duct. Extraperitoneal fluid collection noted at lateral part of abdomen. 1c) Enhanced axial CT scan shows extraperitoneal fluid collection seen at lateral part of abdomen. 1d) Enhanced axial CT scan through shows extraperitoneal fluid collection seen at lateral and anterior part of abdomen. The bowels are displaced laterally and posteriorly by fluid in the extraperitoneum.
Patients would come with complaints varying from abdominal pain, abdominal distension, constitutional symptoms, nausea, and vomiting. Severe pain is however, rare. As noted in our case, patients present with vague and nonspecific complaints. This renders diagnosis and appropriate management difficult. Establishing an accurate diagnosis is important when a patient comes with such a clinical presentation.
Pancreatic ascites has to be distinguished from ascites due to liver cirrhosis, tuberculosis (TB), or malignancy. A fluid analysis that reveals elevated levels of amylase and protein leads to an accurate diagnosis. An amylase level of more than 1000 IU/L, with total protein of >3 g/dL is diagnostic of pancreatic ascites [2,3]. In our case, diagnosis was achieved by an elevated amylase level, the patient’s background history, and CT evidence of extraperitoneal fluid collection with pancreatic pathology. This is further supported by negative cytology and culture from the fluid analysis. Owing to its rare occurrence, the pathophysiology of pancreatic ascites is until this day not fully understood. A few theories have been proposed from the literature. These include disruption of the main pancreatic duct, rupture of a pancreatic pseudocyst, or due to leakage from an unknown site [1,2]. With regards to the CT findings in our case, we were unable to definitively ascertain the pathophysiology. Although it was confirmed in our case that the fluid was of pancreatic origin, we were unable to explore what lead to the large amount of fluid to be collected extraperitoneally. Preferably, we would like to have performed a magnetic resonance cholangiopancreatography, possibly with secretin enhancement, to visualize ductal disruption; as this may confidently assist in preoperative diagnosis should that be needed [4]. Unfortunately, patient was lost to follow up. Treatment should be instituted in accordance to the cause. An initial approach to treatment via an endoscopic route, that is inserting a transpapillary stent is acceptable, avoiding the need for surgery [5-7]. Following failed medical therapy and endoscopic methods, surgical intervention is warranted [6]. A conservative approach is deemed appropriate when the underlying cause is chronic alcoholism, as in our case. Treatment goals include pain management, correction of pancreatic insufficiency, and management of complications, if any. A conservative approach may include the use of somatostatin analogues to reduce pancreatic secretion [7], repeated fluid drainage for symptomatic control, use of octreotide and keeping the patient nil by mouth (NBM) with parenteral nutrition. In our case, patient presented with recurrent abdominal distension with a background of alcoholic CLD and after failed medical therapy was eventually noted to have chronic pancreatitis with extraperitoneal fluid collection. This is rare, but successfully treated by drainage and conservative management.
Learning points
Unexplained recurrent abdominal distension after peritoneal tapping warrants further investigation by imaging.
CT scan abdomen is the modality of choice for further assessment of ascites because diagnosis of extraperitoneal fluid can be missed.
Patients with background of alcoholic CLD and presenting with recurrent abdominal distension and pain, diagnosis of extraperitoneal ascites from chronic pancreatitis need to be considered.
Acknowledgement
The authors declare no conflict of interest related to this work.
References
- Yasuda T, Kamei K, Araki M, et al. Extraperitoneal fluid collection due to chronic pancreatitis. Case. Rep. Gastroenterol. 7,322-326 (2013).
- Cerezo JG, Cano AB, Suarez I et al. Pancreatic ascites: study of therapeutic options by analysis of case reports and case series between the years 1975 and 2000. Am. J. Gastroenterol. 98,568-577 (2003).
- Prakash K. Pancreatic ascites and pleural effusion, pancreatitis-treatment and complications, Prof Luis Rodrigo (Ed). ISBN: 978-953-51-0109-3. (2012).
- Sandrasegaran K, Tann M, Jennings G et al. Disconnection of the pancreatic duct: an important but overlooked complication of severe acute pancreatitis. Radiographics. 27,1389-1400 (2007).
- Kozarek RA. Management of pancreatic ascites. Gastroenterology & Hepatology. 3,362-264 (2007).
- Perwaiz A, Singh A, Chaudhary A. Surgery for chronic pancreatitis. Indian. J. Surg. 74,47-54 (2012).
- Kanneganti K, Srikakarlapudi S, Acharya B et al. Successful management of pancreatic ascites with both conservative management and pancreatic duct stenting. Gastroenterology. Res. 2,245-247 (2009).