Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 7
Chronic tophaceous gout arthritis with infected giant podagra on first ray: a case report
- *Corresponding Author:
- Richard Afandi
Resident of Orthopaedics and Traumatology Department, Faculty of Medicine Udayana University, Sanglah General Hospital, Indonesia
E-mail: drrich.afandi@gmail.com
Abstract
Gout Arhritis is a purine metabolism disorder that leads to hyperuricemia and monosodium urate monohydrate crystal deposition in musculoskeletal system and others. Tophaceous deposits are well-known to lead joint destruction, which can be complicated by secondary infection condition. The prevalence and incidence of gout vary from a prevalence of < 1% to < 6.8% and an incidence of 0.58 per 1,000 person/years to 2.89 per 1,000 person/years.
We presented a case of 56-years-old male came with the complained of lumps on both ankles and feet since 9 y. From physical examination, we found multiple tophi on his feet and infected giant podagra on the right foot associated with secondary infection. This symptoms is enhanced by laboratory result and imaging that confirming chronic gout arthritis. For clinician, diagnosing gout arthritis sometimes quite challenging which requiring investigation through joint or tophi aspirations. There are some other diagnosis that often mimicking the clinical feature of gout arthritis like, cellulitis, Reiter's disease, Pseudogout and Rheumatoid Arthritis (RA).
Gout arthritis itself commonly treated with conservative treatment but 10% of patients with clinical gout developed destructive tophi. This kind of stage will need further surgical intervention, including; surgical reconstruction debridement and resection arthroplasty, joint fusion and even amputation.
Keywords
gout arthritis • multiple tophi • podagra • conservative treatment • surgical treatment.
Introduction
Gout Arhritis is a purine metabolism disorder that leads to hyperuricemia and monosodium urate monohydrate crystal deposition in musculoskeletal system and others. Tophaceous deposits are well-known to lead joint destruction, which is can complicated by secondary infection condition. The prevalence and incidence of gout vary from a prevalence of < 1% to < 6.8% and an incidence of 0.58 per 1,000 person/years to 2.89 per 1,000 person/years. In daily practice, the clinicians often find some difficulty for diagnosing gout arthritis that sometimes quite challenging which requiring investigation through joint or tophi aspirations. There are some other diagnosis that often mimicking the clinical feature of gout arthritis like, cellulitis, Reiter's disease, Pseudogout and Rheumatoid Arthritis (RA).
In this case report, we presented a case of 56-years-old male came with the complained of lumps on both ankles and feet since 9 y. The condition was already chronically established that also associated with secondary infection. The most obvious appearance is the giant podagra that showing that this process have happened in quite long period with no sufficient medication. We are aiming to provide some information and fact about one of the most frequent rheumatology disorder in the population that sometimes misdiagnosed by the clinician how to treated this kind of disease. Although the majority of this disease can be managed by conservative medication but if the late-onset and severe deformity of case was founded, the surgical medication must be elected.
Case Report
A 56-years-old male patient consulted the Orthopaedics and chiefly case of 56-years-old male came with the complained of lumps on both ankles and feet since 9 y. However, since 2015, the lump occurred to have grown bigger and spread to other areas. The condition was also accompanied by intermittent pain. From physical examination, we found multiple tophi on his feet and giant podagra on the right foot associated with secondary infection. Patient does not regularly consume the medication. He had genetic family history from his father whom also suffered of gout arthritis problem. He worked as a carpenter for last 25 y.
On the right foot region, multiple tophi and giant podagra were presented with ulcer and deformity on his first ray (Figure 1). There was also pus discharge come from the ulcer on the right foot with solid consistency sized 0.5 cm to 6 cm, which the biggest is around 1st Metatarsophalangeal Joint (MTPJ), dorsalis pedis artery was palpable with no neurological problem. Furthermore, on the left foot region, multiple tophi occurred around the ankle with swelling and without deformity, minimal tenderness was also observed with solid consistency sized 0.5 cm to 1.5 cm. Moreover, we observed multiple tophi occurred with no deformity, swelling or tenderness, solid consistency sized 0.5 cm to 2.5 cm, on the right and left ankle region (Figure 2).
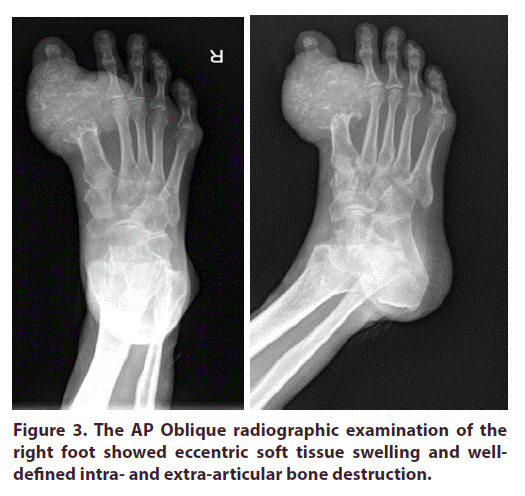
Laboratory evaluation revealed that serum uric acid level of 13 mg/dl (normal range: 2 mg/dl to 7 mg/dl). Meanwhile, the right foot radiographic imaging showed eccentric soft tissue swelling and well-defined intra and extra-articular bone destruction (Figure 3). The 1st MTPJ of the right foot seemed to have destructed.
The treatment method scheduled for this patient is limb salvage surgery. There are two stages of surgical intervention, and the first stage consists of debridement, bone excision and bone cement/ antibiotic beads surgery. Meanwhile, the second stage consists of arthrodesis and fibular graft surgery. Amputation is required when soft tissue is inadequate. Unfortunately, the patient was refused any surgical treatment and decided to choose conservative treatment.
Discussion
Gout is the most common inflammatory arthritis and occurs when hyperuricaemia, sustained elevation of serum urate levels resulting in supersaturation of body tissues with urate, leads to the formation and deposition of monosodium urate crystals in and around the joints. This condition is caused by a purine metabolism disorder that leads to hyperuricemia and monosodium urate monohydrate crystal deposition in cartilage, synovium, bone, tendon, ligament, subcutaneous fat, and skin. There are three stages of gout arthritis include acute arthritis, intercritical, and chronic tophaceous. Tophaceous deposits are well-known to initiated joint destruction, which is complicated by secondary infection. Meanwhile, a condition of secondary infection and discharging sinuses are rare complications while treatment is extremely challenging together with joint destruction, bone loss, and soft-tissue defects [1].
Recent reports of the prevalence and incidence of gout vary widely according to the population studied and methods employed but range from a prevalence of < 1% to < 6.8% and an incidence of 0.58 per 1,000 person/ years to 2.89 per 1,000 person/years. However, in some countries, prevalence rises to 10%. Gout is more prevalent in men than in women, with increasing age, and in some ethnic groups. Furthermore, the prevalence increases to 10% in men and 6% in women above 80%. Despite rising prevalence and incidence, suboptimal management of gout continues in many countries. Typically, only a third to half of patients with gout receive urate-lowering therapy, which is a definitive, curative treatment, and fewer than a half of patients adhere to treatment. Many gout risk factors exist, including. The worldwide incidence of gout increases gradually due to obesity, dietary factors and comorbid conditions, lack of exercise and metabolic syndrome [2,3].
It is important to define the relationship between uric acid, hyperuricemia, and gout to understand gout adequately. Humans cannot express urate oxidase (uricase) enzyme due to a mutation during the uricase gene's evolution, which converts urate to the more soluble and easily excreted compound allantoin. When overproduction or underexcretion of uric acid occurs, the Serum Urate (SU) concentration exceeds the solubility of urate (a concentration approximately > 6.8 mg/dL), resulting in supersaturation of the serum urate (and other extracellular spaces). This state, known as hyperuricemia, imparts a risk of urate crystal deposition in tissues from the supersaturated fluids [4,5].
Many individuals with asymptomatic hyperuricemia and serum urate concentrations greater than 7.0 mg/dl seldom develop any signs or symptoms related to gout condition. In other hand, some individuals experienced gout symptoms at the desired concentration of less than 6 mg/dl [5].
Several diagnostic recommendations have been developed for gout, with the most widely used dating back to 1977 from the American College of Rheumatology (ACR). Traditionally, a clinical diagnosis is performed in patients having podagra or acute monoarticular arthritis with an elevated serum urate concentration (> 7 mg/dl); however, this is not considered definitive without crystal identification. Aspiration of synovial fluid from an affected joint or tophus and recognizing monosodium urate crystals enables a definitive diagnosis and is considered the gold standard.
Meanwhile, each of these techniques has limitations. In some patients, selective classic gout features such as the sudden onset of joint pain, swelling, and tenderness are all absent. Also, there is possibly involvement of another joint other than the metatarsophalangeal joint. Furthermore, uric acid is considered a surrogate marker for acute gouty arthritis. Approximately one-third of patients have normal serum urate concentrations during an acute gout attack, while hyperuricemia occurs in others with no evident symptoms. These factors generally make clinical diagnosis difficult hence, requiring investigation through joint or tophi aspirations.
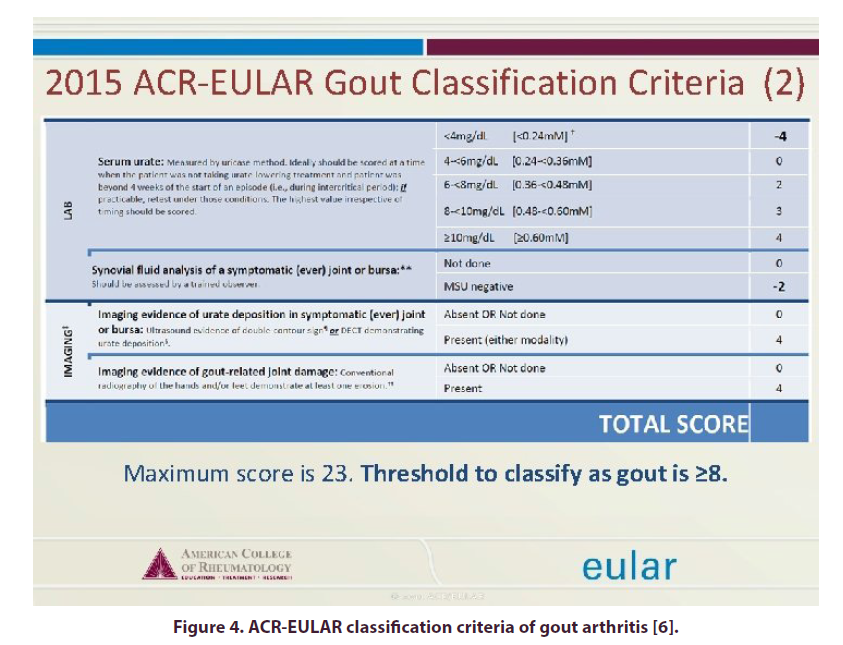
However, the skills and equipment to perform diagnostic joint aspiration in primary care are limited. Together with conventional radiography, these imaging methods have gained popularity over recent years and are widely studied. The ACR and European League Against Rheumatism (EULAR) funded the study Updated Gout Classification Criteria (SUGAR) to renew outdated recommendations. As a result of this collaboration, new ACR/EULAR gout classification criteria were provided in 2015. This is a multifaceted scoring; a score of 8 or higher (of a maximum score of 23) indicates a positive gout diagnosis [6].
Other crystal-induced arthropathies, which are also clinically presented as gouty arthritis, were considered for differential diagnosis. Meanwhile, Calcium Pyrophosphate Dehydrates Crystal Deposition (CPPD), causes rapid onset of severe pain and self-limiting synovitis with erythema attacks. Traditionally, this phenomenon is referred to as "pseudo-gout" due to symptom similarities caused by monosodium urate crystals in gout. Compared to gout, CPPD takes more time to reach peak intensity, persists for months despite therapy, and usually affects large joints. Differentiating CPPD from true gouty arthritis requires arthrocentesis to confirm the presence of calcium pyrophosphate dihydrate crystals (in CPPD) or monosodium urate crystals (in gout) in the synovial fluid. CPPD is ruled out in patients with presumed gouty arthritis and is treated with pharmacotherapy but fails to respond within an anticipated time frame. Other differential diagnosis that can mimicking this condition is including cellulitis, rheumatoid arthritis and Reiter's disease [5].
Conventional radiography, ultrasound, CT, and MRI contributes to the diagnosis and assessment of gouty arthritis. Vasil'ev and Obramenko reported that MRI enhances information obtained from the radiographic examination, improving the ratio of correctly diagnosed cases. Also, it was pointed that both X-ray and MRI images show tophus formation in affected joints [7].
Moreover, the soft tissue's radiologic features, bone and joints of chronic tophaceous gout patients are not usually seen until 6 y to 12 y after the initial attack. The soft tissue consists of calcific deposits and eccentric juxta-articular lobulated masses (hand, elbow, knee, ankle and foot). Bone findings include "mouse bites" from long-standing erosion of soft-tissue tophi, bone infarction, "punch-out" lytic bone lesions and marginal sclerosis. Joint findings comprise joint margins erosion with sclerosis, cartilage destruction and periarticular swelling [5].
Treatment is often based on the particular clinical phase the patient is experiencing. Acute gout treatment aims to reduce pain and inflammation, while the intercritical period treatment aims to maintain low levels of serum uric acid to prevent further formation of tophi. Chronic tophaceous gout is treated by initiating long-term hypouricaemic therapy. Currently, there is no evidence of the efficacy of asymptomatic hyperuricemia therapy. Furthermore, treatment is also divided into three groups, based on purpose. The first group of drugs is intended to treat acute gout and attacks that occur during this phase. The second group is used to prevent recurrent gout, while the third group is aimed at lowering serum uric acid. The medications include: Non-Steroidal Anti-Inflammatory Drugs (NSAID), Colchicine, Corticosteroid, Allopurinol [8].
Despite adequate medical treatment, 10% of patients with clinical gout developed destructive tophi. Meanwhile, surgical intervention is mainly to permit bearing shoe weights in the lower extremity to stabilize joints, relieve pain, and control infection. The surgical indications are divided into four main categories:
1. Functional, which includes excision to permit clothing
2. Symptomatic, to control drainage and infection, reduce pain and decompression of nerves.
3. Cosmetic restoration.
4. Metabolic, to lessen total body urates.
In surgical treatment, tophi involving the metaphysis and endangering the joint are curetted through a window in the bone, thereby preserving the periosteum extensively. When there is extensive bone loss occurred, the cavity is packed with cancellous bone chips. The last surgical treatment modality is amputation. Furthermore, when the curettage and bone grafting is not possible, coupled with ulcerating skin due to expansion, amputation is often the last resort [9].
Some clinicians was treated chronic gouty tophi superimposed with osteomyelitis and septic arthritis using staged surgical reconstruction of the first ray. The same algorithm was also used in performing the diagnosis. However, the treatment choice was to reconstruct the first ray. Debridement and resection arthroplasty of the first metatarsophalangeal joint was performed. Meanwhile, Polymethylmethacrylate antibiotic-loaded bone cement was used as a spacer, while an external fixation device was also applied. After 6 weeks, the spacer was removed along with reconstructing the defect using tricortical iliac crest autograft fixed with a reconstruction plate. Hence bone union was successfully achieved [10].
Surgical interventions aim to improve function, alleviate symptomatic discomfort, improve appearance, eradicate draining sinuses and remove large urate deposits. These interventions become inevitable when the overlying soft tissue ulcerates and (or) becomes infected. The surgery timing also affects the functional outcome. However, it is unnecessary to wait for either the infection or ulceration of the skin. Directly shaving the tophaceous masses is a more straightforward and rapid approach to reducing the total body urate burden. Furthermore, sinus draining surgery is associated with relatively high complications such as poor wound healing; hence, surgery before ulceration development is prudent [11].
Limb salvage surgery is the primary goal in patients that requires surgical treatment. Tophi involving metaphyses are curetted while bone defects were managed using bone grafts reconstructed with other substitutes. Joint fusion in an available position is necessary for flail joints, while amputation is considered the last option [11].
Gout arthritis is also could associated with several comorbidities, such as hypertension, cardiovascular disease, heart and renal failure, diabetes mellitus, obesity, hyperlipidemia and metabolic syndromes. These complications appear to be linked by a common pathogenetic pathway represented by insulin resistance. These comorbidities also expose patients to a high risk of cardiovascular mortality and morbidity resulting from postoperative myocardial infarction and peripheral vascular disease. Comorbidities such as heart disease, hypertension, diabetes mellitus, heart failure, and sleep apnea are more common in gout patients than normal individuals. Therefore, safe treatment selection for these patients is often a major challenge for clinicians [12].
Conclusion
Gout disease with less pronounced tophi is often managed conservatively. However, in patients with extensive bone and soft-tissue loss, the risk of superinfection justifies surgical treatment. Meanwhile, the results of complicated cases are not without morbidity. Therefore, early surgical treatment prevents extremity loss and further complications. In severe cases such as compliance issues, amputation provides acceptable results.
References
- Sariyilmaz K, Eren I, Ozkunt O et al. Bilateral first-ray amputation of the foot due to severe tophaceous gout complicated by infection and discharged sinus: A case report. J. Am. Podiatr. Med. Assoc. 108(1), 58–62 (2018).
- Dehlin M, Jacobsson L, Roddy E et al. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat. Rev. Rheumatol. 16(7), 380–390 (2020).
- Ragab G, Elshahaly M, Bardin T et al. Gout: An old disease in new perspective – A review. J. Adv. Res. 8(5), 495–511 (2017).
- Schlesinger N. Diagnosis of gout: Clinical, laboratory, and radiologic findings. Am. J. Manag. Care. 11(SUPPL. 15), 443–450 (2005).
- Wilson L, Saseen JJ. Gouty Arthritis: A Review of Acute Management and Prevention. Pharmacotherapy. 36(8), 906–922 (2016).
- Neogi T. 2015 gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis. Rheumatol. 67(10), 2557–2568 (2015).
- Obramenko IE. Magnetic resonance imaging differential diagnosis of psoriatic polyarthropathy with gouty polyarthropathy and rheumatoid polyarthritis. Vestn. Rentgenol. Radiol. (1), 29–33 (2013).
- Fang Z hua, Waizy H. Current concepts in the treatment of gouty arthritis. Orthop. Surg. 5(1), 6–12 (2013).
- Yetkîn H, Takka S, Kanatli U. Surgical treatment of chronic tophaceous gout arthritis in the feet: A case report. Foot. Ankle. Surg. 5(3), 155–157 (1999).
- Stapleton JJ, Rodriguez RH, Jeffries LC et al. Salvage of the First Ray with Concomitant Septic and Gouty Arthritis by Use of a Bone Block Joint Distraction Arthrodesis and External Fixation. Clin. Podiatr. Med. Surg. 25(4), 755–762 (2008).
- Ashley W. Blom, David Warwick, Michael R. Whitehouse. Apley & Solomon's System of Orthopaedics and Trauma. CRC. Press. 10th Edn, (2018).
- Zhong M. Research on Complications of Gout and Prevention. SSPHE. 196(Ssphe 2018), 255–257 (2019).