Research Article - Clinical Practice (2018) Volume 15, Issue 3
Clinical and epidemiological characteristics analysis of measles in Shenzhen, China from 2010 to 2016
- Corresponding Author:
- Yan-rong Wang
Pediatrics department, Shenzhen Third People’s Hospital, Shenzhen, China
E-mail: 123rong@sohu.com
Abstract
The aim of this study is to explore the epidemiological trend, clinical characteristics and treatment of hospitalized measles from 2010 to 2016. Totally 1890 cases of measles were diagnosed in Shenzhen Third People’s Hospital from January 2010 to December 2016. The morbidity of measles increased during 2013-2015. Measles mostly occurred in June and July. 39.0% cases had not been vaccinated. 209 patients were younger than 6 months among which half patients’ mother had been vaccinated. 421 patients were older than 18 years. The majority of the patients presented with the typical manifestations such as persistent fever, rash, tears, photophobia, rough oral mucosa and Koplik’s spot. Pertussis-like symptom occurred in 10 patients younger than 3 years old. Liver dysfunction occurred more frequently in adult measles. All patients were cured. The number of measles patients increases in infants younger than 8 months old, so it is urgent to suggest that vaccination might be given to those younger than the designated age of vaccination. The adults presented with more liver damage, which should be paid more attention in the process of diagnosis and treatment.
Keywords
measles, epidemiology, clinical characteristics, vaccination
Introduction
Measles is a universal highly contagious illness which usually occurred in children under 5. In spite of the routine national childhood vaccination throughout China for more than 20 years, measles remains a public health concern. In 2005, the Chinese State Council proclaimed that immunization was required at the time of entry to primary school or kindergarten in order to ensure that school-age children have beenvaccinated against measles. As a matter of fact, measles morbidity decreased dramatically, from 99.5 cases per million people in 2008 to 7.4 in 2011. However, measles transmission continued mainly among unvaccinated preschool-aged children, younger than 8-month-old infant and vaccinated adults [1-3]. Adults and atypical measles increased recently. To better understand the main point of measles elimination in Shenzhen, we explore the epidemiological trend, clinical characteristics, treatment of hospitalized patients with measles from 2010 to 2016.
Materials and methods
Ethical consideration
This investigation was approved by the Ethics Committee of Shenzhen Third People’s Hospital on April 23, 2016. Informed consent was obtained from the patients or the patients’ guardians.
Data collection
We reviewed the medical records of all cases of measles diagnosed in Shenzhen Third people’s Hospital by medical practitioners from January 1st 2010 to December 31st 2016. All the enrolled cases meet the requirements for diagnostic criteria of measles. Clinical, laboratory and epidemiological data were analyzed. We used SPSS 13.0 for data collection and analysis. Typical measles presented as manifestations such as persistent fever, rash, tears, photophobia, rough oral mucosa and Koplik’s spot. Atypical cases presented without Koplic’s spot. All hospitalized patients were confirmed by positive IgM enzyme-linked immunosorbent assay in a World Health Organization (WHO) Global Measles and Rubella Laboratory [4-7].
Statistical analysis
The χ2 test was used for categorical data. P<0.05 was considered statistically significant in all cases. All statistical analysis was performed using SPSS 13.0.
Results
Age and gender distributions of measles patients
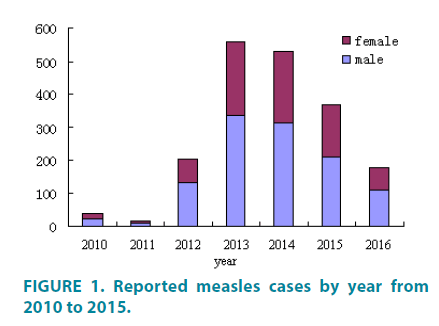
During 2010 and 2016, a total of 1890 measles cases were identified. The annual number of measles cases fluctuated between 38 and 558 (FIGURE 1). High measles incidence occurred in 2013 and 2014.
Figure 1: Reported measles cases by year from 2010 to 2015.
The age distribution of measles in 2016, compared with 2012, 2013 and 2014, changed significantly (p<0.0001) (TABLE 1). Infants (younger than 1 year and older than 6 months) had the highest age-specific incidence. There was a newborn case in 2012 and 2014 respectively accounted for their mothers’ infection. In 2013, the highest incidence (48.2%) occurred in children aged 6 months -1 year, followed by 14.2% in those aged 1-3 years. 209 patients were younger than 6 months among which half patients’ mother had been vaccinated. Of 1890 measles cases, 1135 cases are boys and 755 girls. There was a male predominance of measles cases, with a male-to-female ratio between 1.36:1 and 2.25:1 (TABLE 2).
| Group | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|---|---|---|
| <1 m | 0 | 0 | 1(0.5%) | 0 | 1(0.2%) | 0 | 0 |
| 1-6 m* | 4(10.5%) | 1(7.7%) | 22(10.7%) | 48(8.6%) | 119(22.5%) | 12(3.3%) | 3(1.7%) |
| 6 m-1 y* | 23(60.5%) | 8(61.5%) | 96(46.8%) | 269(48.2%) | 205(38.8%) | 22(6.0%) | 8(4.5%) |
| 1-3 y | 4(10.5%) | 0 | 44(21.5%) | 79(14.2%) | 42(7.9%) | 192(52.2%) | 82(45.8%) |
| 3-4 y | 1(2.6%) | 0 | 5(2.4%) | 21(3.8%) | 12(2.3%) | 9(2.4%) | 9(5.0%) |
| 4-7 y | 2(5.3%) | 0 | 4(2.0%) | 10(1.8%) | 4(0.8%) | 7(1.9%) | 0 |
| 7-14 y | 0 | 1(7.7%) | 1(0.5%) | 15(2.7%) | 30(5.7%) | 19(5.2%) | 6(3.4%) |
| 14-20 y | 0 | 1(7.7%) | 1(0.5%) | 17(3.0%) | 0 | 9(2.4%) | 3(1.7%) |
| 20-30 y | 2(5.3%) | 2(15.4%) | 16(7.8%) | 47(8.4%) | 52(9.8%) | 62(16.8%) | 46(25.6%) |
| >30 y | 2(5.3%) | 0 | 15(7.3%) | 52(9.3%) | 64(12.0%) | 36(9.8%) | 22(12.3%) |
| Total | 38 | 13 | 205 | 558 | 529 | 368 | 179 |
*P<0.001
Table 1: Age distribution of measles from 2010 to 2016.
| Year | Number | Male | Female | Ratio |
|---|---|---|---|---|
| 2010 | 38 | 22 | 16 | 1.73 |
| 2011 | 13 | 9 | 4 | 2.25 |
| 2012 | 205 | 132 | 72 | 1.83 |
| 2013 | 558 | 338 | 220 | 1.54 |
| 2014 | 529 | 313 | 216 | 1.45 |
| 2015 | 368 | 212 | 156 | 1.36 |
| 2016 | 179 | 109 | 70 | 1.56 |
Table 2: Gender distribution of measles from 2010 to 2016.
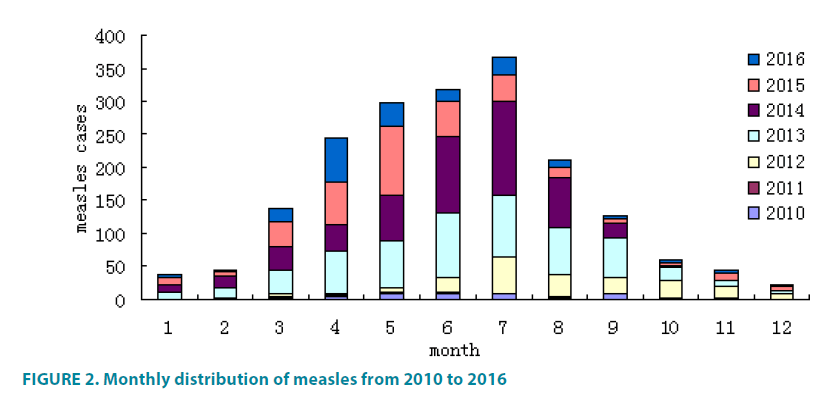
Monthly distributions of measles cases
A seasonal peak presents between June and July (FIGURE 2). About one third (36.9%) of measles occurred during this period. 83.3% (1574/1890) of patients were admitted to hospital. The number of hospitalized cases in 2010 was 29. Then in 2011, 2012, 2013, 2014, 2015 and 2016, the number was 10, 190, 408, 450, 358 and 129 respectively. There is a peak hospitalized cases by year in 2013 and 2014.
Figure 2: Monthly distribution of measles from 2010 to 2016
Status of measles vaccination
The status of measles vaccination was known in 89%. 39.0% cases had not been vaccinated. The other patients had vaccination once. No patient had vaccination twice. In 2014,119 (22.5%) cases aged 1-6months (the undesignated age of vaccination) were diagnosed as measles.
Clinical and laboratory characterization of measles cases
The most common clinical characterizations were rash, persistent fever, tears, photophobia, rough oral mucosa and Koplik’s spot. Pertussislike symptom occurred in 10 patients younger than 3 years old [8,9]. 70.2% patients presented with complications such as bronchopneumonia or pneumonia. The majority (76.8%) of the patients presented with throbocythemia during the recovery stage. No death occurred in our patients. Bronchopneumonia or pneumonia was more common among the patients <4 years of age (75%) than among adult measles>18 years of age. On the contrary, liver dysfunction occurred more often in those patients >18 years of age (65%). The common cases received symptomatic treatment and the severe patients were treated with additional intravenous immunoglobulin. All the patients were cured.
Discussion
Our findings presented varied incidence of measles in different years. The different incidence might be attributed to varying degrees of vaccination. Measles is a vaccine-preventable disease with reproduction rates about 12-18 indicating that average person with measles might infect 12-18 other people if his or her contact were susceptible. It is difficult to take an interruption of indigenous transmission in the early stages when symptoms are non-specific. Isolation can be a problem if a large number of children present with possible infective rash illness [10-13]. Although an effective vaccine against measles has been available for the past 40 years, the disease is still endemic in many countries or parts. From 2010 to 2016, 1890 cases were reported in our patients and the disease appears more frequently in summer [14-18]. Similar to previous studies, our report suggested that its seasonal peak occurred in June and July. Routine epidemiological surveillance and more preventive protocols should be carried out during the period. The high measles incidence in 2013 and 2014 attributed to the delayed diagnosis of those atypical cases and the inadequate vaccination coverage in nomadic population.
With rapid urbanization, many families migrate with young children for employment opportunities in Shenzhen City. In spite of China’s Expanded Program on Immunization (EPI) system officially declaring that all ageeligible children receive free vaccines regardless of residency status, it is difficult for immunization practitioners to be aware of children who are new arrival to an area. So those children of migrant workers missed opportunities to immunize. Our patients without measles vaccination comprising 78% accounted for the importance of vaccination. Similar to previous report, the measles resurgence in Shenzhen from 2013 to 2014 was largely a result of missed opportunities to immunize. Missed opportunities to immunize delayed the elimination efforts and immunization programs for decades. Local Centers for Disease Control and Prevention and immunization practitioners should implement policies about the frustration in Shenzhen [19].
Our study provided the evidence that patients younger than 1 year old accounted for more than 44.5% of the reported cases with measles. The proportion of patients was the highest in those children below 8 months of age who received no vaccination which comprised about half of the reported cases. So it is urgent to suggest that vaccination might be given to those younger than the designated age of vaccination.
About 421 patients were older than 20 years in our patients. So measles cannot be regarded solely as a childhood contagious disease. Increased transaminases were observed in 65.0% adult measles but photophobia might not be seen regularly. The atypical characteristics might contribute partly to the delayed diagnosis of adult patients. Consequently, it is desirable to isolate the suspected adult patients urgently and pay more attention in the process of diagnosis and treatment. 76.8% patients presented with throbocythemia during the recovery stage. Further studies could be investigated about the relationship between the laboratory feature and the measles’s diagnosis and outcome.
Previously measles outbreak from 1985 to 1986 presented that about 60% of nonpreventable measles cases were appropriately vaccinated with 1 dose after 12 months and that 67% of outbreaks occurred in school-age children not eligible for vaccination under the then existing 1-dose policy [20]. Hence, in 1989, 2 doses of measles-containing vaccine were recommended to be given to all children. Initially the second dose of measles-containing vaccine recommended as 11-12 years, at present it was revised as 5-6 years because revaccination of children at school entry was more practical than the revaccination of older children and to further prevent school-based outbreaks. No cases in our patients received 2 doses of measlescontaining vaccine. It is obliged to increase the immunization coverage levels and approaches to new entrants into elementary schools.
Our data collection may have been partial and artificial. The inpatients’ laboratory data may not be representative as all children with measles residing in Shenzhen. We have designed the study rationally and interpreted the results to solve the problem [21]. Firstly, Shenzhen Third People’s Hospital is the only institution in the city to specialize in infectious diseases. The majority of patients were diagnosed in the hospital and the patients that were suspected of Measles and seen in other hospitals in the city were transferred to the hospital. Secondly, patients’ blood samples were collected to identify by positive IgM enzyme-linked immunosorbent assay.
In summary, the study supports recommendations [1] vaccination might be given to those younger than the designated age of vaccination [2]. The infant measles presented a greater morbidity of pulmonary infection, and the adults characterized with more liver damage, which should be paid more attention in the process of diagnosis and treatment [3,21]. It is obliged to identify the vaccination record check at school entry.
Declaration of interest
The authors declare that they have no competing interests.
Authorship
Yan-rong Wang, Xian-feng Wang drafted the manuscript. Dong-ming Pan collected and chose the cases. Yan-rong Wang finalized the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank Pei-fa Zhang for his contribution to the revised figures and tables.
References
- Moss WJ, Griffin DE. Measles. Lancet. 379(9811), 153-164 (2012).
- Berti E, Martino DE, Chiappini E, et al. Analysis of measles-related hospitalizations in Tuscany from 2000 to 2014. Epidemiol. Infect. 144(12), 2605-2612 (2016).
- Muscat M. Who gets measles in Europe? J. Infect. Diseases. 204 Suppl 1, S353-365 (2011).
- Perry RT, Marta GD, Alya D, et al. Centers for Disease Control and Prevention (CDC). Progress toward regional measles elimination-worldwide, 2000-2013. Morbidity Mortality Weekly Report. 63(45), 1034-1038 (2014).
- Chao M, Zhijie A, Lixin H, et al. Progress toward measles elimination in the People’s Republic of China, 2000-2009. J. Infect. Diseases. 204(Suppl 1), S447-454 (2011).
- Chao M, Lixin H, Gregory CJ, et al. Risk factors for measles in children aged 8 months-14 years in China after nationwide measles campaign: A multi-site case-control study, 2012-2013. Vaccine. 34(51), 6545-6552 (2016).
- Choi WS, David HS, Youngmee J, et al. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J. Infect. Diseases. 204(Suppl 1), S483-490 (2011).
- John TJ, Plotkin SA, Orenstein WA. Building on the success of the expanded programme on immunization: enhancing the focus on disease prevention and control. Vaccine. 29(48), 8835-8837 (2011).
- Jacqui Wise. Doctors call for better management of suspected measles cases. BMJ. 346, f1127 (2013).
- Muscat M, Bang H, Wohlfahrt J, et al. Measles in Europe: an epidemiological assessment. Lancet. 373(9661), 383-389 (2009).
- Gao J, Chen E, Zhu BP, et al. Epidemic of measles following the nationwide mass immunization campaign. BMC Infect. Dis. 13, 139 (2013).
- Mekonen G, Beyene B, Ademe A, et al. Epidemiology of laboratory confirmed measles virus cases in Amhara Regional State of Ethiopia, 2004-2014. BMC Infectious Dis.16, 133 (2016).
- Carrillo-Santisteve P, Lopalco PL. Measles still spreads in Europe: who is responsible for the failure to vaccinate? Clin. Microbiol. Infect. Suppl5, 50-56 (2012).
- Sun M, Zhang J, Hou W, et al. Immunization status and risk factors of migrant children in densely populated areas of Beijing, China. Vaccine. 28(5), 1264-1274 (2010).
- The measles epidemic. The problems, barriers, and recommendations. The National Vaccine Advisory Committee. JAMA. 266(11), 1547-1552 (1991).
- Hu Y, Li Q, Luo S, et al. Timeliness vaccination of measles containing vaccine and barriers to vaccination among migrant children in East China. PLoS One 8, e73264 (2013).
- Biswas AB, Mitra NK, Nandy S, Sinha RN, Kumar S. Missed opportunities for immunization in children. Indian J. Public Health. 44(1), 23-27 (2000).
- Centers for Disease Control and Prevention (CDC). Epidemiology and Prevention of Vaccine-Preventable Diseases. Chapter 10, Measles. Pink Book 13th Edition, (2015).
- Allam MF. Measles vaccination. J. Prev. Med. Hyg. 50(4), 201-205 (2009).
- Sugerman DE, Waters-Montijo K, Lebaron CW, et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally under vaccinated. Pediatrics. 125(4), 747-755 (2010).
- American Academy of Pediatrics. Committee on Infectious Diseases. Age for routine administration of the second dose of measles-mumps-rubella vaccine. Pediatrics. 101(1), 129-133 (1998).