Special Report - Imaging in Medicine (2012) Volume 4, Issue 6
Clinical decision support systems for utilization of CT in the emergency department
Ivan K Ip*1,2 & Frank S Drescher1,2,31Department of Medicine, Dartmouth-Hitchcock Medical Center, 1 Medical Center Drive, Lebanon, NH 03756, USA
2The Geisel School of Medicine at Dartmouth, Hanover, NH, USA
3VA outcomes group at White River Junction, VT, USA
- Corresponding Author:
- Ivan K Ip
Department of Medicine
Dartmouth-Hitchcock Medical Center
1 Medical Center Drive, Lebanon, NH 03756, USA
Tel: +1 617 840 2232
E-mail: ivan.k.Ip@dartmouth.edu
Abstract
Over the past two decades, healthcare costs have been growing at a rate that is unsustainable. Despite its vast utility, diagnostic medical imaging has been a culprit of the rising healthcare expenditure. Health information technology, particularly clinical decision support systems, has been promoted as a tool that can potentially improve the efficiency of imaging delivery by encouraging appropriateness of testing, thereby decreasing unnecessary radiation exposure and costs. Despite some promising early results, evidence of clinical decision support systems on imaging utilization in the emergency department remains sparse. Nevertheless, health information technology provides promising opportunities for translational and implementational research. Further research is needed to understand the barriers to clinical adoption and broad implementation in the community.
Keywords
computerized physician order entry n electronic medical records n healthcare IT n health policy n information technology n medical informatics
Over the last decade, health information technology (HIT) has revolutionized healthcare [1]. Recent research suggests that hospitals with electronic medical records, computerized order entry and clinical decision support had fewer complications, lower mortality rates and lower costs [2]. However, how HIT has impacted diagnostic imaging utilization is unclear. The aims of this article are to examine how clinical decision support systems have affected the field of imaging, specifically, the use of CT in the emergency department and to identify key features associated with successful clinical decision support.
Information technology, diagnostic imaging & radiation exposure: progress & pitfalls
Recent advancements in diagnostic imaging have enhanced physicians’ ability to diagnose diseases quickly and accurately, and have undoubtedly contributed tremendously to patient care. However, easy availability of diagnostic testing carries the risk of overutilization with resultant increased healthcare costs and medical radiation exposure [3,4]. Costs incurred by medical imaging tests are substantial. In 2007, imaging services expenditure totalled US$11.4 billion among Medicare beneficiaries alone in the USA [101]. Advanced diagnostic imaging use has similarly increased among patients enrolled in large integrated healthcare systems from 1996 to 2010 [5]. Furthermore, in recent years, there has been growing concern in both the healthcare and public sectors regarding possible cancer risk associated with diagnostic imaging [6,102]. The increased use of CT has resulted in a doubling of the mean per capita effective dose of radiation exposure [5], with great variation across institutions and study types [7]. The radiation exposure may be associated with future cancer risk [8]. It is estimated that as many as 29,000 cancers could be related to CT scans alone in the USA annually [9].
Beyond the immediate risk of radiation and incurred costs, there are concerns that overutilization and increased sensitivity of diagnostic testing may result in overdiagnosis – the detection of disease that otherwise would never have become relevant to the patient. Downstream effects of overutilization and overdiagnosis include unnecessary follow-up imaging, potentiating further radiation risks. Additionally, potentially harmful procedures and treatments may be the consequence [10]. For all these reasons, researchers and policy makers have called for a more judicious use of diagnostic imaging and many believe that HIT may provide an elegant solution.
Can a clinical decision support system improve outcome?
Computerized physician order entry (CPOE) is a process of order entry whereby physicians and other providers communicate instructions for the care of patients electronically over a computer network. An important component of CPOE is the embedded clinical decision support system (CDSS). A classic CDSS includes alerts and reminders that automatically inform the clinician of a specific action, providing real-time feedback to optimize user decisions and actions. The level of importance can be addressed in their implementation by using a variety of solutions. They can range from hard-stops that prevent providers from moving forward in the medical chart to simple educational pop-up windows or banners that pose no barrier to workflow. Thus, CDSSs can be designed to educate, encourage and enforce the use of evidence in day-to-day practice, in the hope of optimizing clinical practice. CDSSs have been shown to have a positive impact on a physician’s performance, safety and outcomes in a variety of settings. In a systematic review, Garg et al. found that clinical decision support may improve practitioner performance through improved diagnosis, preventive care, disease management, and drug dosing and prescribing [11].
CDSSs for diagnostic imaging
Diagnostic imaging has become a popular target for the application of CDSSs to guide clinicians in a more judicious utilization of diagnostic imaging. For example, a provider may place an order of a head CT on a patient with a minor head injury and the CDSS may prompt the clinician that, in the absence of red flags, a CT scan may not be necessary based on current evidence. Initial experience shows promising impact of CPOE on some physician imaging ordering practices [12–16]. While the primary target of a CDSS is clinicians, it may also have a secondary impact on patients. CDSSs may give patients the perception that clinical decisions in imaging are based on conscientious, explicit use of current best evidence. At Massachusetts General Hospital (MA, USA), the implementation of an integrated decision support system was associated with substantial decreases in the growth of outpatient CT and US procedures [12]. The same group also subsequently found that the order-entry system was associated with a decrease in low-yield outpatient examinations, from 5.4 to 1.9% [17]. However, other groups have found varying success with CDSSs [14,18].
Diagnostic imaging in emergency departments
The increase in medical imaging is most evident in the emergency department (ED) setting. The prevalence of CT or MRI use for injury-related conditions increased from 6% in 1998 to 15% in 2007 [19]. In one university-affiliated urban ED, the intensity of abdominal imaging examinations per 1000 ED visits increased by 2.7-fold in relative value units between 1990 and 2009 [20]. Repetitive imaging of the same patient frequently visiting the ED is a common occurrence [21,22]. Causes for the recent imaging expansion is probably multifactorial, with contributing factors including defensive medicine, uncertainty about imaging indications, self-referral by physicians and patient expectation [23–27].
Current state of HIT in the ED
The emergency department is an ideal setting to study the impact of a CDSS for several reasons. First, the American College of Emergency Physicians recognizes and endorses the potential benefits of HIT on improving the quality of emergency care, reducing medical errors and promoting patient safety [103]. Furthermore, much of current emergency medicine research focuses on the development of appropriateness of imaging. A number of clinical decision rules have been developed and validated, such as the Canadian CT head rule [28], the New Orleans Criteria [29], the Ottawa ankle [30] and knee [31] rules, and the NEXUS for cervical spine imaging [32,33]. The American College of Emergency Physicians has issued numerous clinical policy statements emphasizing the efficient utilization of diagnostic CT and practice variation in the ED [34,35]. However, the translation of the guideline policies into clinical practice remains challenging and variable [36]. CDSSs may help address some of the barriers in evidence translation and improve clinician decision-making at the point of care.
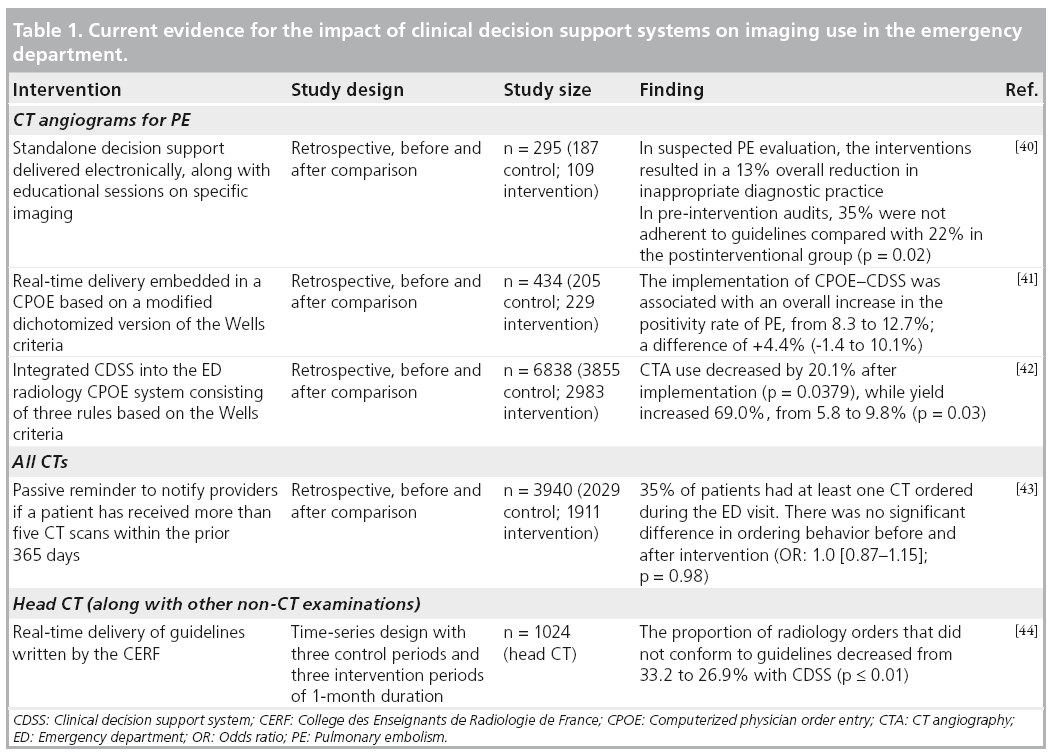
Much of the research in CDSSs in the ED has centered on pulmonary embolism (PE), repeat imaging and head CT. Please see Table 1 for summary of findings.
Clinical decision support system for suspected PE: less is more
Clinical prediction scores, such as the Wells Criteria, have been validated and are recommended for the diagnosis of venous thromboembolism by national guidelines [37,38]. The Wells score allows for the risk stratification of patients with suspected PE based on seven clinical data points [39]. Due to the strength of the evidence associated with Wells and its translatability to actionable automated decision support, chest CT angiography (CTA) in patients with suspected PE has received considerable attention as a study of target for CDSSs.
In one single-institution study, Bairstow et al. developed and implemented a standalone electronic application called the diagnostic imaging pathway to deliver decision support to assist clinicians in choosing the most appropriate imaging exam [40]. Four clinical conditions were targeted: suspected PE, ankle injury, suspected renal colic and nontraumatic acute abdominal pain. Using a retrospective observational study design, the authors were able to demonstrate that a simple CDSS intervention resulted in a 13% overall reduction in inappropriate diagnostic imaging for suspected PE. Up to 35% of studies were not adherent to guidelines in the preintervention audits compared with only 22% in the postinterventional group (p = 0.017).
Drescher et al. also assessed how CDSSs can impact inappropriate imaging by integrating real-time delivery into its CPOE in patients with suspected PE [41]. The investigators implemented a mandatory pop-up window that provided a Wells score calculator and automatically provided recommendations based on the prediction score. Implemented in one ED over a 4‑month study period, the CDSS resulted in a trend towards enhanced yield of chest CTA, but the difference was not statistically significant. A review of 434 CTA examinations found the study-positivity rate was 8.3% in the pre-intervention period, compared with 12.7% postintervention, with a difference of 4.4% (95% CI: -1.4 to 10.1%). Unfortunately, their CDSS was poorly accepted by emergency physicians, resulting in poor adherence to the CDSS and it being discontinued from the CPOE after study completion. When asked, reasons given for nonadherence to the computerized decision support system algorithm included too much time spent at the computer and away from the patient and a lack of belief that the computerized decision support system was helpful for guiding patient evaluations.
Using a similar before and after comparison study design, Raja et al., at their academic ED, retrospectively analyzed data from the radiology database, as well as radiology reports, for the presence/absence of PE [42]. They found that a CDSS is associated with a significant decrease in utilization, as well as an improvement in the yield of CTAs. The quarterly use of CT rose 82.1% before implementation of CDSS, from 14.5 to 26.4 CT scans/1000 patients (p < 0.0001). After implementation of CDSS, quarterly use decreased by 20.1%, from 26.4 to 21.1 CT scans/1000 patients (p = 0.04). Of all the CTAs performed during this 6-year period, the yield by quarter increased from 5.8 to 9.8% subsequent to the implementation of CDSS (p = 0.03).
Reducing radiation: can knowledge change behavior?
Reducing unnecessary radiation exposure to patients has been a priority ever since evidence has shown that radiation is associated with an increased cancer risk. One study examined how a passive reminder to notify providers if a patient has received more than five CT scans within the prior 365 days may influence their ordering behavior. Horng et al., in their singleinstitution study, retrospectively compared 2029 patients in the preintervention period with 1911 postintervention [43]. They found that the passive reminder resulted in no significant change in physician ordering patterns (p = 0.98, odds ratio: 1.0), even after adjusting for age, gender, disposition, acuity, number of consults, days since last ED visit and days since last CT ordered.
CT of the head: implementation of guidelines
Through a time-series study, Carton et al. made appropriate guidelines available to practitioners on alternating months during a 6-month study period in two European EDs [44]. During intervention months, onscreen reminders were displayed to illustrate the appropriate recommendations concerning the clinical context, and practitioners were alerted if requests did not conform to guidelines. The availability of guidelines in the CPOE system decreased the percentage of radiology orders that did not conform to guidelines from 33.2 to 26.9% (p = 0.0001). However, there were significant differences across the two EDs (17.6% in site A and 34.8% in site B; p = 0.0001).
Clinical adoption of CDSSs: what are the barriers?
Despite the potential of CDSSs for enhancing evidence-based practice, reducing unnecessary imaging and improving patient safety, there are barriers to the implementation of CDSSs. Based on the experience of Drescher et al., it appears that time and convenience to access CDSSs is critical to end users [41]. Ip et al. have found that, in the implementation of CPOE, feature enhancements that optimize workflow are vital to adoption and meaningful use [45]. Kawamoto et al. noted that effective CDSSs should be computer based and provide automatic provision of decision support as part of the physicians workflow [46]. The success of a CDSS is dependent on a host of factors and may vary with the nature of the clinical problem [47,48]. Bates and co-authors offer ‘ten commandments’ for effective CDSSs: speed, anticipation of needs and delivery in real time, fitting the users’ workflow, usability, recognition of physician resistance, altering rather than stopping behavior, simplicity, minimization of information requested, assessment of results with feedback and response, and monitoring and maintaining knowledge-based systems [49].
Practitioners are likely to ignore a CDSS unless it is concise, context specific and relevant to their current decision, delivered at the point of care. As noted by Lobach et al., “provision of a recommendation, not just an assessment,” “justification of decision support via provision of research evidence,” and “promotion of action rather than inaction” are all important features associated with successful CDSS implementation [104]. The optimal form of evidence is peerreviewed literature, such as those of decisionmaking rule and cost–effectiveness analysis. Practice guidelines, such as the American College of Radiology Appropriateness Criteria and the American Heart Association Cardiac Imaging Guidelines, may also be useful. Both the American College of Radiology and the American Heart Association devised imaging guidelines as a result of wide variation in practice, in the hope that such criteria would improve the value of imaging [50,51]. In addition, effective CDSSs must be easily translatable to contextspecific actions. Vague reminders that are not specific to the clinical context are less likely to influence behavior.
In the experience of the authors, constant monitoring and modifications as needed are critical to ensure that the CDSS has the desired effects. Furthermore, organizational culture is vital to adopting technology in healthcare. Even the most well-designed CDSS delivery system will ultimately fail if attention is not paid to organizational processes and corporate culture. A culture emphasizing quality and safety, and a clearly stated vision from the highest levels of the organization are essential elements in the success of HIT.
CDSSs for medical imaging in the ED: more evidence is needed
The results of research investigating the impact of the CDSS on the utilization of CT imaging in the ED are promising. However, the strength of the evidence remains sparse so far. One reason for the lack of high-quality evidence may be that this type of research is at the crossroads of outcomes research, implementation research, systems redesign and medical informatics. Researchers specifically investigating the utility of CDSSs require a broad skillset that often goes beyond clinician researchers’ traditional abilities. Another challenge is that research investigating CDSSs has to address the rapid pace at which HIT is progressing. Research that was relevant 5 years ago may be obsolete today because of advances in HIT. Investigators may therefore revert to the more easy to implement research strategies, such as observational or before- and after-study design.
Adoption rates of CDSSs in the community are unknown, but expected to be low. Financial barriers, physicians’ resistance and concern about interoperability have been cited as potential obstacles to adoption [52]. Decreasing the number of imaging procedures may actually pose a financial disincentive for private, for-profit hospitals in a fee-for-service environment. However, it is the expectation that with the Health Information Technology for Economic and Clinical Health Act and the American Recovery and Reinvestment Act, a more widespread national adoption of HIT will ensue in the upcoming years; thus, some much-needed data on global impact of CDSSs will have to be generated.
Future perspective
Without doubt, the revolution of HIT will continue at a rapid pace. The opportunities for CDSSs in healthcare systems are tremendous. As more clinical practice guidelines and appropriateness criteria are developed, CDSSs will be increasingly relied upon to function as a tool in accelerating the adoption of such evidence into clinical practice. HIT holds one key to eliminating waste and improving quality, with a potentially large impact on decreasing unnecessary cost in healthcare. However, to fully realize the benefits of HIT, HIT developers will need to collaborate with clinician researchers to implement outcomes research showing the eff icacy of CDSSs. As current research identif ies barriers to implementation of CDSSs, further work is required to specif ically address these concerns and find solutions. Clearly, CDSS development/upgrades are needed to improve user friendliness of HIT systems and provide better integration into the provider’s workflow in the ED.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Agrawal R, Grandison T, Johnson C, Kiernan J. Enabling the 21st century health care information technology revolution. Commun. ACM 50, 34–42 (2007).
- Amarasingham R, Plantinga L, Diener-West M, Gaskin DJ, Powe NR. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch. Intern. Med. 169, 108–114 (2009).
- Iglehart JK. The new era of medical imaging – progress and pitfalls. N. Engl. J. Med. 354, 2822–2828 (2006).
- Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N. Engl. J. Med. 357, 2277–2284 (2007).
- Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff. (Millwood) 27, 1491–1502 (2008).
- Amis ES Jr, Butler PF. ACR white paper on radiation dose in medicine: three years later. J. Am. Coll. Radiol. 7, 865–870 (2010).
- Smith-Bindman R, Lipson J, Marcus R et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch. Intern. Med. 169, 2078–2086 (2009).
- Cardis E, Vrijheld M, Blettner M et al. Risk of cancer after low doses of ionising radiation: retrospective cohort study in 15 countries. BMJ 331, 77 (2005).
- Berrington de González A, Mahesh M, Kim KP et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch. Intern. Med. 169, 2071–2077 (2009).
- Armao D, Semelka RC, Elias J Jr. Radiology’s ethical responsibility for healthcare reform: tempering the overutilization of medical imaging and trimming down a heavyweight. J. Magn. Reson. Imaging 35, 512–517 (2012).
- Garg AX, Adhikari NK, McDonald H et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 293, 1223–1238 (2005).
- Sistrom CL, Dang PA, Weilburg JB, Dreyer KJ, Rosenthal DI, Thrall JH. Effect of computerized order entry with integrated decision support on the growth of outpatient procedure volumes: seven-year time series analysis. Radiology 251, 147–155 (2009).
- Georgiou A, Prgomet M, Markewycz A, Adams E, Westbrook JI. The impact of computerized provider order entry systems on medical-imaging services: a systematic review. J. Am. Med. Inform. Assoc. 18, 335–340 (2011).
- Blackmore CC, Mecklenburg RS, Kaplan GS. Effectiveness of clinical decision support in controlling inappropriate imaging. J. Am. Coll. Radiol. 8, 19–25 (2011).
- Sanders DL, Miller RA. The effects on clinician ordering patterns of a computerized decision support system for neuroradiology imaging studies. Proc. AMIA Symp. 583–587 (2001).
- Solberg LI, Wei F, Butler JC, Palattao KJ, Vinz CA, Marshall MA. Effects of electronic decision support on high-tech diagnostic imaging orders and patients. Am. J. Manag. Care 16, 102–106 (2010).
- Vartanians VM, Sistrom CL, Weilburg JB, Rosenthal DI, Thrall JH. Increasing the appropriateness of outpatient imaging: effects of a barrier to ordering low-yield examinations. Radiology 255, 842–849 (2010).
- French SD, Green S, Buchbinder R, Barnes H. Interventions for improving the appropriate use of imaging in people with musculoskeletal conditions. Cochrane Database Syst. Rev. 1, CD006094 (2010).
- Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA 304, 1465–1471 (2010).
- Raja AS, Mortele KJ, Hanson R, Sodickson AD, Zane R, Khorasani R. Abdominal imaging utilization in the emergency department: trends over two decades. Int. J. Emerg. Med. 4, 19 (2011).
- Ip IK, Mortele KJ, Prevedello LM, Khorasani R. Repeat abdominal imaging examinations in a tertiary care hospital. Am. J. Med. 125, 155–161 (2012).
- Drescher FS, Kremens K, Young J. Characterization of patients undergoing repeated emergency evaluation by CT and angiography for pulmonary embolism. Am. J. Respir. Crit. Care Med. 171, A181 (2008).
- Levin DC, Rao VM. Turf wars in radiology: other causes of overutilization and what can be done about it. J. Am. Coll. Radiol. 1, 317–321 (2004).
- Studdert DM, Mello MM, Sage WM et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 293, 2609–2617 (2005).
- Margulis AR, Bhargavan M, Feldman D, Sunshine JH. Should the ordering of medical imaging examinations be reexamined? J. Am. Coll. Radiol. 2, 809–811 (2005).
- Bhargavan M, Sunshine JH. Utilization of radiology services in the United States: levels and trends in modalities, regions, and populations. Radiology 234, 824–832 (2005).
- Friedman DP, Smith NS, Bree RL, Rao VM. Experience of an academic neuroradiology division participating in a utilization management program. J. Am. Coll. Radiol. 6, 119–124 (2009).
- Stiell IG, Wells GA, Vandemheen K et al. The Canadian CT head rule for patients with minor head injury. Lancet 357, 1391–1396 (2001).
- Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N. Engl. J. Med. 343, 100–105 (2000).
- Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Worthington JR. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann. Emerg. Med. 21, 384–390 (1992).
- Stiell IG, Wells GA, McDowell I. Use of radiography in acute knee injuries: need for clinical decision rules. Acad. Emerg. Med. 2, 966–973 (1995).
- Hoffman JR, Wolfson AB, Todd K, Mower WR. Selective cervical spine radiography in blunt trauma: methodology of the National Emergency X-Radiography Utilization Study (NEXUS). Ann. Emerg. Med. 32, 461–469 (1998).
- Goergen SK, Fong C, Dalziel K, Fennessy G. Can an evidence-based guideline reduce unnecessary imaging of road trauma patients with cervical spine injury in the emergency department? Australas. Radiol. 50, 563–569 (2006).
- Jagoda AS, Cantrill SV, Wears RL et al. Clinical policy: neuroimaging and decision making in adult mild traumatic brain injury in the acute setting. Ann. Emerg. Med. 52, 714–748 (2008).
- American College of Emergency Physicians Clinical Policies Committee, Clinical Policies Committee Subcommittee on Suspected Pulmonary Embolism. Clinical policy: critical issues in the evaluation and management of adult patients presenting with suspected pulmonary embolism. Ann. Emerg. Med. 41, 257–270 (2003).
- Mendelson RM, Bairstow PJ. Imaging pathways: will they be well trodden or less traveled? J. Am. Coll. Radiol. 6, 160–166 (2009).
- Bates SM, Jaeschke R, Stevens SM et al. Diagnosis of DVT: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141(2 Suppl.), e351S–e418S (2012).
- Writing Group For The Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, d-dimer testing, and computed tomography. JAMA 295, 172–179 (2006).
- Wells PS, Anderson DR, Rodger M et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann. Intern. Med. 135, 98–107 (2001).
- Bairstow PJ, Persaud J, Mendelson R, Nguyen L. Reducing inappropriate diagnostic practice through education and decision support. Int. J. Qual. Health Care 22, 194–200 (2010).
- Drescher FS, Chandrika S, Weir ID et al. Effectiveness and acceptability of a computerized decision support system using modified wells criteria for evaluation of suspected pulmonary embolism. Ann. Emerg. Med. 57, 613–621 (2011).
- Raja AS, Ip IK, Prevedello LM et al. Effect of computerized clinical decision support on the use and yield of CT pulmonary angiography in the emergency department. Radiology 262, 468–474 (2012).
- Horng S, Reichenbach S, Nathanson LA, Fischer C, Sarwar A, Sanchez L. The effect of a passive reminder on computed tomography utilization in the emergency department. Ann. Emerg. Med. 58, S293–S294 (2011).
- Carton M, Auvert B, Guerini H et al. Assessment of radiological referral practice and effect of computer-based guidelines on radiological requests in two emergency departments. Clin. Radiol. 57, 123–128 (2002).
- Ip IK, Schneider LI, Hanson R et al. Adoption and meaningful use of computerized physician order entry with an integrated clinical decision support system for radiology: ten-year analysis in an urban teaching hospital. J. Am. Coll. Radiol. 9, 129–136 (2012).
- Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 330, 765 (2005).
- Reilly BM, Evans AT. Translating clinical research into clinical practice: impact of using prediction rules to make decisions. Ann. Intern. Med. 144, 201–209 (2006).
- Buller-Close K, Schriger DL, Baraff LJ. Heterogeneous effect of an emergency department expert charting system. Ann. Emerg. Med. 41, 644–652 (2003).
- Bates DW, Kuperman GJ, Wang S et al. Ten commandments for effective clinical decision support: making the practice of evidencebased medicine a reality. J. Am. Med. Inform. Assoc. 10, 523–530 (2003).
- Hendel RC, Berman DS, Di Carli MF et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/ SCMR/SNM 2009 Appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J. Am. Coll. Cardiol. 53, 2201–2229 (2009).
- Taylor AJ, Cerqueira M, Hodgson J et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/ NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J. Am. Coll. Cardiol. 56, 1864–1894 (2010).
- Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized physician order entry in U.S. hospitals: results of a 2002 survey. J. Am. Med. Inform. Assoc. 11, 95–99 (2004).
- Medicare Payment Advisory Commission. A data book: healthcare spending and the Medicare program. www.medpac.gov/documents/ Jun10DataBookEntireReport.pdf (Accessed 15 January 2011)
- National Cancer Institute Radiation Risks and Pediatric Computed Tomography (CT): A Guide for Health Care Providers. www.cancer.gov/cancertopics/causes/ radiation/radiation-risks-pediatric-CT (Accessed 20 October 2012)
- American College of Emergency Physicians ACEP Policy Statement on Health Information Technology. www.acep.org/Content.aspx?id=29534 (Accessed 20 October 2012)
- Lobach D, Sanders G, Bright TE et al. Enabling Health Care Decisionmaking Through Clinical Decision Support and Knowledge Management. Agency for Healthcare Research and Quality (US), MD, USA (2012). www.ncbi.nlm.nih.gov/books/NBK97318 (Accessed 20 October 2012)
■ Websites


