Research Article - Clinical Investigation (2020) Volume 10, Issue 3
Comparative Evaluation of MTA Pulpotomy and Laser-Assisted MTA Pulpotomy in Primary Teeth: A Randomized Clinical Trial
Submitted: 04 March 2020; Accepted: 12 March 2020; Published online: 05 July 2020
Abstract
Context and Aim: Formocresol has been used as the material of choice (gold standard) for pulpotomy procedures because of the ease of use but was discouraged due to its potential immune sensitization and mutagenic effects. Laser irradiation was first applied for pulpotomy procedure in the year 1985. Recently, diode lasers have been used for pulpotomy in primary teeth and have shown clinical success rates comparable to formocresol. The present in-vivo study was carried out to compare the clinical and radiographic success rates of Mineral Trioxide Aggregate (MTA) alone and diode laser-MTA for pulpotomy in human primary molars. Materials and Methods: The present study was a randomized clinical trial in design wherein forty primary teeth requiring pulpotomy treatment which met the selection criteria (clinical and radiographic) were divided into two groups, group 1 (n=20) wherein the pulpotomy was performed with MTA alone and group 2 (n=20) wherein laser-assisted pulpotomy was performed with MTA (L-MTA). The patients were recalled after 3, 6 and 9 months respectively and evaluated clinically and radiographically. Statistical Analysis Used: The data were analyzed using the Statistical Package for the Social Sciences (SPSS) Version 22 (IBM corporation, Washington DC, United States). Descriptive statistics were used to analyze the data while the Pearson's correlation coefficient test was used to analyze the statistical correlation between the overall success rates observed in the clinical and radiographic findings of both the groups. p<0.05 was considered statistically significant. Results: The clinical success rate in the MTA group was 90%, 84.21% and 88.23% at 3, 6 and 9 months respectively with no clinical signs or, symptoms reported at the said follow-up visits while the radiographic success rate was found to be 85%, 84.21%, and 82.3% respectively. On the contrary, the clinical success rate in the L-MTA group was found to be 95%, 94.74% and 94.44% at 3, 6 and 9 months respectively with the radiographic success rate reported being 90%, 89.47%, and 88.89% respectively. Conclusion: The combination of diode laser and MTA yielded better clinical and radiographic success rates over the pulpotomy procedures done with the help of MTA alone.
Keywords
Cpulpotomy • diode lasers • MTA
Introduction
The goals of an ideal pulpotomy procedure are removal of pulpal inflammation, maintenance of arch length and masticatory function. Formocresol has been used as the material of choice (gold standard) for pulpotomy procedures because of the ease of use but was discouraged due to its potential immune sensitization and mutagenic effects [1]. Alternative medicaments like glutaraldehyde, ferric sulfate, Mineral Trioxide Aggregate (MTA), bone morphogenic proteins, dentin bonding agents, enamel matrix derivatives, freeze-dried bone, growth factors and various techniques like electrosurgery and lasers have been tried with variable clinical, radiological and histological success rates. MTA has the ability to stimulate cytokine release from the bone cells indicating that it actively promotes hard tissue formation to provide an enhanced seal over the vital pulp and is non-resorbable [2]. Furthermore, MTA was reported to have superior biocompatibility, better sealing ability, dentinal bridge inducing materials, and is relatively less cytotoxic than other materials currently used for pulp therapies [2-4]. Lasers have been used for carrying-out pulpotomy procedures in primary teeth as they maintain a sterile environment and reduce inflammation. Laser irradiation was first applied for pulpotomy procedure by Shoji S et al. [5] in the year 1985. Lasers, also, possess hemostatic, antimicrobial and cell-stimulating properties with the added advantages of an improved wound healing and no mechanical damage on the remaining pulp tissue. For the said reasons, laser irradiation was suggested as a promising alternative to conventional pharmacotherapeutic strategies [6]. Lasers that have been tested and have demonstrated predictable outcomes in pulpotomy procedures include carbon dioxide (CO2), neodymium-doped yttrium aluminum garnet; Nd:Y3Al5O12 (Nd:YAG) and erbium-doped yttrium aluminum garnet; Er:Y3Al5O12 (Er:YAG) lasers. Recently, diode lasers have been used for pulpotomy in primary teeth and have shown clinical success rates comparable to formocresol. The choice of laser use on pulp tissue is dependent on the Tissue Resistant Temperature (TRT) values of the pulp. The TRT values are tissue-specific and directly related to the water content and vascularity. Diode laser suits the TRT values of pulp due to high absorbance at 810 nm wavelength avoiding excessive heating and charring of pulp. The present in-vivo study was carried out to compare the clinical and radiographic success rates of Mineral Trioxide Aggregate (MTA) alone and diode laser-MTA for pulpotomy in human primary molars.
Materials and Methods
The present study was a randomized clinical trial in design with approval from the Institutional Ethics Committee wherein children aged between 6 to 8 years with deeply carious primary molars (maxillary or, mandibular) with vital pulp and with no history of spontaneous pain or, any other clinical or, radiographic evidence of a periapical pathology were included. Also, the absence of an abscess or, sinus opening, absence of internal and/or, external root resorption, and interradicular and/or, furcal bone destruction were the other prominent inclusion criteria. Furthermore, the possibility of proper restoration of the teeth was an absolute criterion based on which forty primary molars requiring pulpotomy treatment were selected randomly from 60 children who had attended the Department of Pedodontics and Preventive Dentistry and were divided into two groups, group 1 (n=20) wherein the pulpotomy was performed with MTA alone and group 2 (n=20) wherein laser-assisted pulpotomy was performed with MTA (L-MTA).
Procedure
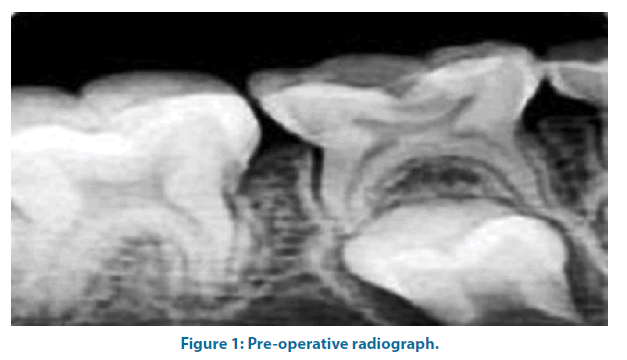
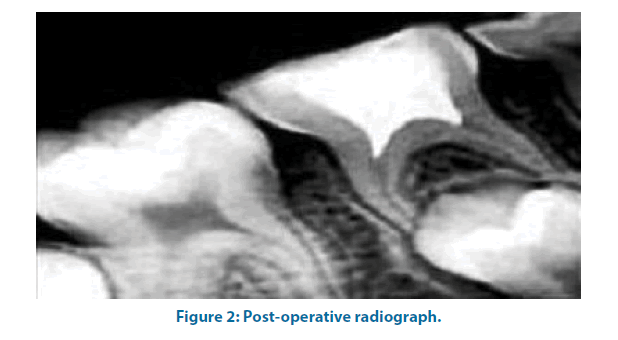
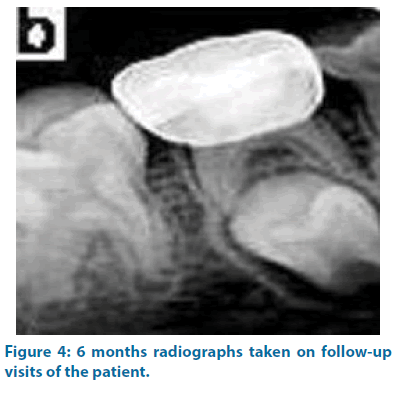
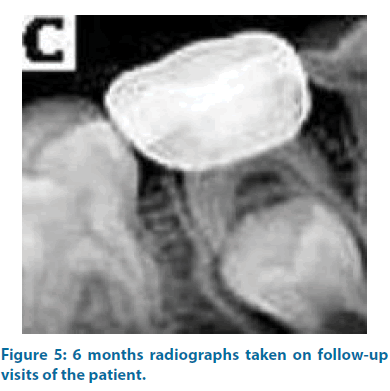
After completing the pre-operative radiographic examination of the selected tooth with the help of an Intra-Oral Peri-Apical Radiograph (IOPAR) (Figure 1), the tooth was anesthetized and isolation was done with the help of rubber dam of appropriate size. Caries and unsupported enamel/dentin were removed with a spoon excavator. Pulp chamber was approached using a round bur and further, caries was removed and coronal access was made using a #245 bur (Dentsply, USA) in a high-speed handpiece (Dentsply, USA) with water as a coolant. Coronal pulp was removed to the canal orifices with the help of a Hu-Friedy sharp spoon excavator. The pulp chamber was irrigated with saline to remove debris. Hemostasis was achieved using a dry, sterile cotton pledget gently pressed against the amputated pulp tissues for about 5 minutes. In the MTA group, after achieving hemostasis, MTA (ProRoot; Dentsply, USA) was mixed as per the prescribed manufacturer’s instructions and placed on the amputated pulp tissues with a thickness of approximately 2 mm-3 mm using a plastic filling instrument. A wet cotton pledget was, then, placed over MTA for approximately 10 minutes. In the L-MTA group, after achieving primary hemostasis, the root canal orifices were exposed to the Diode Laser (Picaso, Germany) of 810 nm with the continuous mode of application for approximately 2 seconds delivered by 200 microns optical fiber tip in contact mode at 1.5 W power. All the subjects and operators wore appropriate eye protection wears during the application of the laser. In both the groups, the treated teeth were restored with GIC Type IX (GC Fuji IX, GC Corporation Tokyo, Japan) followed by a repeat radiographic examination with the help of IOPAR (Figure 1) for the sake of future comparisons. The pulpotomized teeth were, then, restored with stainless steel crowns. The patients were recalled after 3, 6 and 9 months respectively and evaluated clinically and radiographically (Figures 2-5). The clinical symptoms assessed included spontaneous pain, draining sinus, swelling or, abscess, mobility, premature exfoliation while the radiological symptoms assessed were evidence of inter-radicular radiolucency, periodontal ligament space widening, peri-apical radiolucency and internal and/or, external root resorption.
Statistical analysis used
The data was analyzed using the Statistical Package for the Social Sciences (SPSS) Version 22 (IBM corporation, Washington DC, United States). Descriptive statistics were used to analyze the data while the Pearson’s correlation coefficient test was used to analyze the statistical correlation between the overall success rates observed in the clinical and radiographic findings of both the groups. p<0.05 was considered statistically significant.
Results
The mean age of patients in the present study was 7.08 years in the MTA group and 6.92 years in the L-MTA group. In the MTA group, male patients accounted for 40% and female patients were 60% while in the L-MTA group, male and female patients were equal in distribution. A total of 23 left and 17 right mandibular molars were treated in the MTA group while 13 left and 7 right mandibular molars were treated in the L-MTA group. Table 1 depicts the clinical and radiographic evaluation of pulpotomized teeth in the MTA group at the various follow-up intervals wherein it is shown that 88.23% of the teeth presented with no signs or, symptoms at 9 months’ follow-up visit while only 1 patient presented with pain. At the same time, 82.35% of the teeth presented with no abnormal radiographic findings after 9 months of the procedure in the MTA group. Likewise, Table 2 depicts the clinical and radiographic evaluation in the L-MTA group at various followup intervals wherein, on the contrary, 94.44% of the teeth presented with no signs or, symptoms after 9 months of the procedure while again, only 1 patient presented with pain. Furthermore, 88.89% of the teeth presented with no abnormal radiographic findings in the L-MTA group at the said follow-up visit. The clinical success rate in the MTA group was found to be 90%, 84.21% and 88.23% at 3, 6 and 9 months follow-up visits respectively (Table 1) as against the L-MTA group in which it was found to be 95%, 94.74% and 94.44% at 3, 6 and 9 months (Table 2). Likewise, the radiographic success rate was 85%, 84.21% and 82.3% in the MTA group at 3, 6 and 9 months follow-up visits respectively (Table 1) as against 90%, 89.47% and 88.89% in the L-MTA group (Table 2).
| Clinical Findings | Clinical evaluation | ||
|---|---|---|---|
| 3 months | 6 months | 9 months | |
| No sign/symptom | 18 | 16 | 15 |
| -90% | -84.21% | -88.23% | |
| Symptoms of pain | 1 | 0 | 1 |
| -5% | 0% | -5.88% | |
| Tenderness to percussion | 1 | 2 | 1 |
| -5% | -10.53% | -5.88% | |
| Swelling and/or, sinus opening | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Pathological tooth mobility | 0 | 1 | 0 |
| 0% | -5.26% | 0% | |
| Total | 20 | 19 | 17 |
| -50% | -50% | -48.57% | |
| p-value | 0.149 | 0.136 | 0.145 |
| Radiographic Findings | Radiographic Evaluation | ||
| 3 months | 6 months | 9 months | |
| No abnormal radiographic finding | 17 | 16 | 14 |
| -85% | -84.21% | -82.35% | |
| External root resorption | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Periodontal ligament space widening and furcation radiolucency | 2 | 2 | 2 |
| -1% | -10.53% | -11.76% | |
| Internal root resorption | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Furcation and/or, periapical radiolucency | 1 | 1 | 1 |
| -5% | -5.26% | -5.88% | |
| Total | 20 | 19 | 17 |
| -50% | -50% | -48.57% | |
| p-value | 0.138 | 0.136 | 0.132 |
Table 1. Clinical and radiographic evaluation in the MTA group at various follow-up intervals.
| Clinical Findings | Clinical evaluation | ||
|---|---|---|---|
| 3 months | 6 months | 9 months | |
| No sign/symptom | 19 | 18 | 17 |
| -95% | -94.74% | -94.44% | |
| Symptoms of pain | 0 | 1 | 1 |
| 0% | -5.26% | -5.56% | |
| Tenderness to percussion | 1 | 0 | 0 |
| -5% | 0% | 0% | |
| Swelling and/or, sinus opening | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Pathological tooth mobility | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Total | 20 | 19 | 18 |
| -50% | -50% | -51.43% | |
| p-value | 0.149 | 0.161 | 0.175 |
| Radiographic Findings | Radiographic Evaluation | ||
| 3 months | 6 months | 9 months | |
| No abnormal radiographic finding | 18 | 17 | 16 |
| -90% | -89.47% | -88.89% | |
| External root resorption | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Periodontal ligament space widening and furcation radiolucency | 1 | 2 | 1 |
| -5% | -10.53% | -5.56% | |
| Internal root resorption | 0 | 0 | 0 |
| 0% | 0% | 0% | |
| Furcation and/or, periapical radiolucency | 1 | 0 | 1 |
| -5% | 0% | -5.56% | |
| Total | 20 | 19 | 18 |
| -50% | -50% | -51.43% | |
| p-value | 0.149 | 0.149 | 0.146 |
Table 2. Clinical and radiographic evaluation in the L-MTA group at various follow-up intervals.
Discussion
The present study represented clinical and radiographic success rates of pulpotomy done with MTA alone and pulpotomy done with MTA assisted with laser in primary teeth. Diode laser have been considered to be the most apt for pulpotomy procedures because it suits best the Tissue Resistant Temperature (TRT) values of the pulp tissue due to high absorbance at 810 nm wavelength avoiding excessive heating and charring of pulp. Mareddy A et al. [6] reported 810 nm at 2 W for 1-and 3-seconds applications to be the most ideal for diode laser pulpotomy procedures as most of the specimens showed intact odontoblasts. Thus, in the present study, also, Diode Laser (Picaso, Germany) of 810 nm with continuous mode of application for approximately 2 seconds delivered by 200 microns optical fiber tip in contact mode at 1.5W power was used. Also, MTA is a material which is known to have proven therapeutic advantages in various endodontic procedures of primary teeth. In the present study, the clinical success rate in the MTA group was found to be 90%, 84.21% and 88.23% at 3, 6 and 9 months respectively with no clinical signs or, symptoms reported at the said follow-up visits while the radiographic success rate was found to be 85%, 84.21% and 82.3% respectively. The clinical success rate of the present study was in accordance with the studies conducted by Agamy HA et al. [7] wherein a clinical success rate of 84.2% was found at 12 months follow-up. The results of the present study, though, were in contrast with the studies conducted by Peng L et al. [8], Subramaniam P et al. [9] and Kabaktchieva R and Gateva N [10] who reported 95%, 95%, and 90.9% success rates respectively in their studies. Furthermore, amongst the 20 teeth studied, 2 teeth revealed tenderness on percussion, 1 tooth showed pathological mobility while 2 teeth showed furcal and periapical radiolucencies. The noncompliance of the patients and patient drop-outs might be the reasons for the relatively low success rate seen in the present study as compared to the said studies. Also, the clinical success rate in the L-MTA group was found to be 95%, 94.74%, and 94.44% at 3, 6, and 9 months respectively with the radiographic success rate reported being 90%, 89.47%, and 88.89% respectively. The clinical success rate in the L-MTA group in the present study was found to be distinctly higher than the other studies conducted by Cuadros- Fernández C et al. [11], Uloopi KS et al. [12] and Vahid Golpayegani M et al. [13] who reported 73.3%, 80%, and 100% success rates respectively in their studies. The higher clinical success rate of 94.44% at 9 months in the present study could be attributed to the strict aseptic/sterilization protocol and the settings of the laser used in the study which might have been responsible for a faster and efficient healing of the pulpal tissue. Nonetheless, compliance of the patients is an important attribute to the success of any procedure done. Also, human clinical trials that compare laser pulpotomies with existing pulpotomy techniques have, also, shown conflicting results with any variation in the laser application parameters including the power, frequency, exposure time and water/air dry-mode bringing variations in the response of the pulpal tissues varying the clinical and radiographic outcomes [14]. In the said group in the present study, clinical failure in the form of tenderness on percussion was seen in 1 tooth at 3 months followup while the radiographic failures in the form of periodontal ligament space widening and furcation radiolucency were seen in 1, 2 and 1 teeth at 3, 6 and 9 months follow-up. Failures of pulpotomy procedures are attributed to several reasons one of which is the failure in diagnosing chronically inflamed pulp as non-inflamed and non-infected with the lesions being silent in the process of chronic inflammation. More accurate diagnostic methods might be the pre-requisite in a proper case selection of teeth with healthy radicular pulps for successful clinical outcomes of pulpotomy procedures. Durmus B and Tanboga I14 reported diode laser pulpotomy to be a promising alternative to the conventional pharmacotherapeutic pulpotomy procedures. In the said study, 97% clinical success rate was reported for formocresolbased pulpotomy procedures as against 95% success rate for ferric sulfate and 100% for the diode laser at 12-month follow-up. Vahid Golpayegani M et al. [13] compared the effectiveness of Low-Level Laser Therapy (LLLT) and conventional formocresol in pulpotomy of primary molars and reported 100% success rate in both the groups after 6 and 12-month follow-up with no statistically significant difference observed in both the groups. The difference in the results obtained in the various studies conducted, though, is due a number of factors that decide the long-term success of the procedures starting from a proper case selection to a strict aseptic protocol, parameters of the laser being used and last, but not the least, the compliance of the patient for the procedure performed.
Limitations
One of the major limitations of the present study was that the follow-up period was relatively short in the present study for up to 9 months only because of which the long-term outcomes of the said therapy and procedures could not be predicted. Also, a lack of evaluation at the histological level becomes another possible limitation of the present study since it relied absolutely on the clinical and radiographic profile and outcomes of the procedures performed which can be misleading sometimes. The present study, therefore, mandates the need for further studies to be conducted in this regard with larger sample sizes and with longer periods of follow-up for coming to valid conclusions.
Conclusion
Within the limitations of the present study, combination of diode laser and MTA yielded better clinical and radiographic success rates over the pulpotomy procedures done with the help of MTA alone, though, considering certain factors like the cost, the clinical set-up required for lasers and ease of manipulation, still, make the use of lasers a little restricted. The present study, thus, mandates the need for further studies including more randomized clinical trials with the same methodology followed in order to achieve a better consensus.
References
- Peng L, Ye L, Guo X, et al. Evaluation of formocresol versus ferric sulphate primary molar pulpotomy: A systematic review and meta-analysis. Int Endod J 40: 751-757 (2007).
- Holan G, Eidelman E, Fuks AB. Long-term evaluation of pulpotomy in primary molars using mineral trioxide aggregate or, formocresol. Pediatr Dent 27: 129-136 (2005).
- Saltzman B, Sigal M, Clokie C, et al. Assessment of a novel alternative to conventional formocresol-zinc oxide eugenol pulpotomy for the treatment of pulpally involved human primary teeth: Diode laser-mineral trioxide aggregate pulpotomy. Int J Paediatr Dent 15: 437-447 (2005).
- Smaïl V, Courson F, Durieux P, et al. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst Rev 8: CD003220 (2014).
- Shoji S, Nakamura M, Horiuchi H. Histo-pathological changes in dental pulps irradiated by CO2 laser: A preliminary report on laser pulpotomy. J Endod 11: 773-780 (1985).
- Mareddy A, Mallikarjun SB, Shetty PV, et al. Histological evaluation of diode laser pulpotomy in dogs. J Oral Laser Appli 10: 7-16 (2010).
- .Agamy HA, Bakry NS, Mounir MM, et al. Comparison of mineral trioxide aggregate and formocresol as pulp-capping agents in pulpotomized primary teeth. Pediatr Dent 26: 302-309 (2004).
- Peng L, Ye L, Tan H, et al. Evaluation of the formocresol versus mineral trioxide aggregate primary molar pulpotomy: A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102: e40-44 (2006).
- Subramaniam P, Konde S, Mathew S, et al. Mineral trioxide aggregate as pulp capping agent for primary teeth pulpotomy: 2 year follow-up study. J Clin Pediatr Dent 33: 311-314 (2009).
- Kabaktchieva R, Gateva N. Vital pulpotomy in primary teeth with mineral teeth with mineral trioxide aggregate (MTA). JIMAB: Annual Proceeding (Scientific Papers), Book 2 (2009).
- Cuadros FC, Lorente AI, Sáez S, et al. Short-term treatment outcome of pulpotomies in primary molars using mineral trioxide aggregate and Biodentine: A randomized clinical trial. Clin Oral Investig 20: 1639-1645 (2016).
- Uloopi KS, Vinay C, Ratnaditya A, et al. Clinical evaluation of low-level diode laser application for primary teeth pulpotomy. J Clin Diagn Res 10: 67-70 (2016).
- Vahid M, Ansari G, Tadayon N. Clinical and radiographic success of low-level laser therapy (LLLT) on primary molars pulpotomy. Res J Biol Sci 5: 51-55 (2010).
- Durmus B, Tanboga I. In-vivo evaluation of the treatment outcome of pulpotomy in primary molars using diode laser, formocresol, and ferric sulphate. Photomed Laser Surg 32: 289-295 (2014).