Research Article - Interventional Cardiology (2022) Volume 14, Issue 1
Comparison of distal radial with conventional radial access in patients with ST-segment elevation myocardial infarction, undergoing primary percutaneous coronary intervention
- Corresponding Author:
- Darko Kitanoski
Department of Cardiology,
University Clinic of Cardiology,
Skopje,
Macedonia,
E-mail: darko_kitanoski85@hotmail.com
Received date: 01-Dec-2021, Manuscript No. FMIC-21-48753; Editor assigned: 03-Dec-2021, PreQC No. FMIC-21-48753 (PQ); Reviewed date: 17-Dec-2021, QC No. FMIC-21-48753; Revised date: 24-Dec-2021, Manuscript No. FMIC-21-48753 (R); Published date: 27-Dec-2021, DOI: 10.37532/1755-5310.2022.14(1).449
Abstract
Background: There is limited data available regarding the technique of dTRA, and its potential benefit in patients with STEMI. This study investigated the feasibility, safety, and potential benefit of dTRA in patients with STEMI, compared to conventional TR approach.
Methods: This was a prospective single center study that included 292 patients referred for STEMI. 152 (52%) patients had primary PCI through distal transradial access, and 140 (48%) had PPCI through conventional radial access. Exclusion criteria was absence of radial artery pulse and previous RAO. We compared clinical and procedure characteristics, access site bleeding complications, rate of Radial Artery Occlusion (RAO) and failure of primary chosen access site between two groups of STEMI patients.
Results: The success rate of the puncture for dTRA was 98.7% (150/152), and for conventional TRA 99.3% (139/140). Successful primary PCI via dTRA and conventional TRA was performed in all patients in both groups. dTRA was associated with lower rate of study clinical outcomes as rate of radial artery occlusion (dTRA: 0%, TRA 5.7%, p=0.0028) and local hematoma according to EASY score (dTRA Grade I: 15.13%, Grade II: 0%, Grade III: 0%, Grade IV: 0%, TRA: Grade I 22.9%, Grade II: 7.1%; Grade III: 0.7%, Grade IV: 0%, p=0.0009). There was no difference recorded in radial artery spasm between two access sites (dTRA: Grade I: 7.2%, Grade II: 2.7%, Grade III: 1.3%, Grade IV: 0%, TRA: Grade I 7.1%, Grade II: 2.1%, Grade III: 0.7%, Grade IV: 0%) and there was no statistically significant difference in access site crossover (dTRA: 2 patients, TRA: 1 patient). dTRA was associated with a longer access time (dTRA 38.6 sec, TRA: 36.3 sec, p=0.0077). Time of hemostasis was significantly shorter with dTRA (dTRA 30-60 min, TRA 120-150 min, p<0.0001).
Conclusion: dTRA is safe and successful in STEMI patients, when performed by experienced radial operators, with previous experience with dTRA. It is associated with lower rate of access site complications and early haemostasis in comparison with TRA.
Keywords
Distal radial access • ST-segment elevation myocardial infarction • Primary percutaneous coronary intervention
Introduction
Use of different access sites for coronary intervention have been changing over the last several decades. Access changed from transfemoral to Transradial Approach (TRA), as it has proven to have less access site complications, decreased mortality rate and is cost-effective compared to the transfemoral approach. In 2015, the European Society of Cardiology guidelines for the management of acute coronary syndrome gave class I recommendation to use the TRA as the preferred method of access for any percutaneous coronary intervention irrespective of clinical presentation [1]. However, the use of TRA is associated with certain complications: Radial Artery Occlusion (RAO), radial artery spasm, radial arterial perforation, radial artery pseudoaneurysm, arteriovenous fistula, bleeding, nerve damage, and complex regional pain syndrome. In the past few years there are publications who showed safety, feasibility and lower access site complications when using distal Radial Access (dTRA) for cardiac catheterization [2,3]. However limited data is available regarding the technique of distal radial artery access in patients presenting with ST-segment elevation myocardial infarction, treated with primary percutaneous coronary intervention. In this trial we make a comparative evaluation of dTRA and conventional TRA in patients with ST-segment elevation myocardial infarction undergoing primary percutaneus coronary intervention.
Methodology
This was a prospective single center study that included 292 patients referred for STEMI (diagnosis according to European Society of Cardiology guidelines) <12 h of symptom onset, undergoing Primary PCI. The procedure was performed by operators experienced with dTRA and conventional TRA, in a high-volume radial artery catheterization laboratory.
152 (52%) patients had primary PCI through distal transradial access, and 140 (48%) had PPCI through conventional radial access. Exclusion criteria was absence of radial artery pulse and previous RAO. We compared clinical and procedure characteristics, access site bleeding complications, rate of Radial Artery Occlusion (RAO) and failure of primary chosen access site between two groups of STEMI patients.
Technique
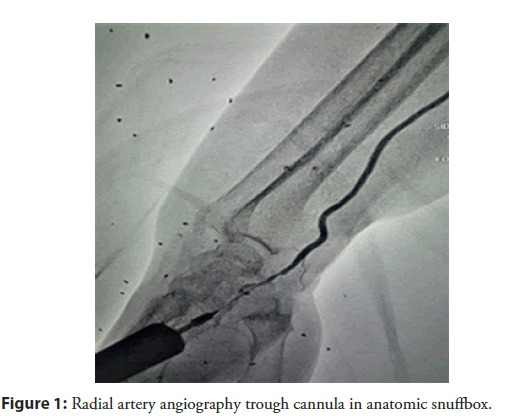
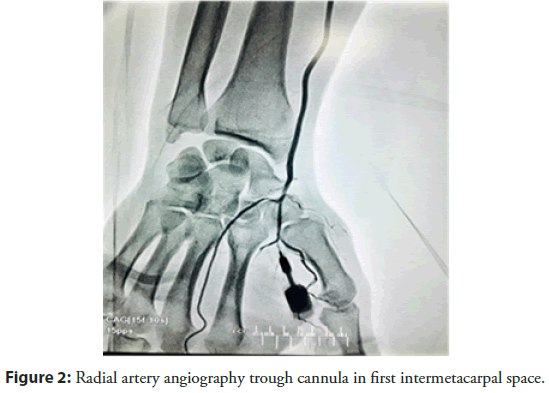
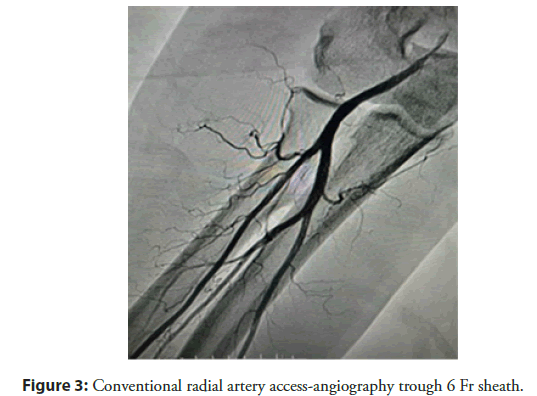
There are two sites at which the radial pulse in dTRA can be found: In the anatomic snuffbox (place were extensor pollicis brevis, abductor pollicis longus, and extensuor pollicis longus tendons made a triangular shaped depression on the radial side of the wriste) (Figure 1) and the first intermetacarpal space (Figure 2). In this study we used the snuffbox approach for dTRA. After infiltration of local anesthetic, radial artery puncture was performed using the counter puncture technique with a 20 G plastic iv cannula and 0.025-inch mini guidewire of 45 cm and followed by 6 Fr or 7 Fr hydrophilic introducer sheath placement. Vasodilators (5 mg Verapamil) were used to avoid radial artery spasm, Heparin 100 I.e/kg iv bolus, Clopidogrel 600 mg, Aspirin 300 mg and statin with maximal dose. Pre-procedural radial artery angiography was performed in all patients to provide a roadmap to successful arterial access (Figure 3). A solution of 3 ml of contrast diluted with 7 ml of blood was injected trough the cannula or through the side arm of the sheath under fluoroscopy in PA projection. The sheath was removed immediately after the procedure, and compressive dressing was applied to the wrist (Figures 4 and 5).
Figure 1: Radial artery angiography trough cannula in anatomic snuffbox.
Figure 2: Radial artery angiography trough cannula in first intermetacarpal space.
Primary outcomes of interest
Clinical: Haematoma was classified into five grades according to the EASY scale (hematoma grading system and the corresponding treatment strategies developed in the context of the Early Discharge After Transradial Stenting of Coronary Arteries (EASY) trial) [4]: (Grade I: Local haematoma, superficial<5 cm; Grade II: Haematoma with moderate muscular infiltration <10 cm; Grade III: Forearm haematoma and muscular infiltration, below the elbow; Grade IV: Haematoma and muscular infiltration extending above the elbow; Grade V: Ischaemic threat-compartment syndrome.
Radial artery occlusion assessed by duplex ultrasound and angiography of the radial artery one month after the procedure, radial artery spasm was classified according to Chugh: Grade I minimal local pain and discomfort; Grade II significant local pain and discomfort, not precluding procedure completion; Grade III severe local pain and discomfort necessitating crossover; Grade IV catheter entrapment with severe local pain and discomfort.
Procedural: Access site crossover is defined as an inability to puncture or inability for sheath insertion. Access time was defined as time from application of local anesthesia to sheath insertion.
Time of hemostasis was defined as time from sheath removal until compressive dressing removal from the wrist.
Statistical analysis
Categorical variables were expressed as numbers and percentages and continuous variables as the mean ± SD, or median. Categorical variables were compared between groups using the χ2 test. The Fisher exact test was used for categorical variables. A p value of<0.05 was considered statistically significant. Statistical analysis was performed with JMP 16.0 for Windows (SASS).
Results
All patient characteristics of both groups are presented in Table 1. The success rate of the puncture for dTRA was 98.7% (150/152), and for conventional TRA 99.3% (139/140). The difference was statistically not significant. Successful primary PCI via dTRA and conventional TRA was performed in all 150 and 139 patients. DTRa was associated with lower rate of study clinical outcomes as rate of radial artery occlusion (dTRA: 0%, TRA 5.7%, p=0.0028) and local hematoma according to EASY score (dTRA Grade I: 15.13%, Grade II: 0%, Grade III: 0%, Grade IV: 0%, TRA: Grade I: 22.9%, Grade II: 7.1%; Grade III: 0.7%, Grade IV: 0%, p=0.0009). There was no difference recorded in radial artery spasm between two access sites (dTRA: Grade I: 7.2%, Grade II: 2.7%, Grade III: 1.3%, Grade IV: 0%, TRA: Grade I: 7.1%, Grade II: 2.1%, Grade III: 0.7%, Grade IV: 0%) and there was no statistically significant difference in access site crossover (dTRA: 2 patients, TRA: 1 patient). dTRA was associated with a longer access time (dTRA 38.6 sec, TRA: 36.3 sec, p=0.0077). Time of hemostasis was significantly shorter with dTRA (dTRA 30-60 min, TRA 120-150 min, p<0.0001). Results are shown in Table 2.
| dTRA% (N=152) | TRA% (N=140) | p value | |
| Gender | Male 67.1 (102) | Male 68.6 (96) | 0.1586 |
| Female 32.9 (50) | Female 31.4 (44) | ||
| Age (years) ± SD | 61.8 ± 10.8 | 60.8 ± 8 | 0.1566 |
| BMI ± SD | 28.8 ± 2.9 | 28 ± 2.2 | 0.0047 |
| DM | 35.5 (54) | 33.6 (47) | 0.7257 |
| HTA | 62.5 (95) | 57.8 (81) | 0.4179 |
| HLP | 34.9 (53) | 24.3 (34) | 0.0482 |
| Smoker | 55.9 (85) | 52.9 (74) | 0.5994 |
| Previous PCI | 5.9 (9) | 5.7 (8) | 0.9399 |
| Sheath Fr | 97.3 (148)-6 Fr | 97.1 (136)-6 Fr | 0.9061 |
| 2.6 (4)-7 Fr | 2.8 (4)-7 Fr | ||
| Use of GP IIb/IIIa inhibitors | 5.9 (9) | 5.0 (7) | 0.7297 |
| Previous oral anticoagulants | 5.2 (8) | 4.4 (6) | 0.6961 |
| Oral anticoagulants at discharge | 6.6 (10) | 6.4 (9) | 0.9585 |
| Hgb g/L ± SD | 143.0 ± 1.1 | 141.3 ± 1.1 | 0.1471 |
| Hct% ± SD | 42.5 ± 4.1 | 42.3 ± 3.8 | 0.718 |
| PLT (10^9/L) ± SD | 239.9 ± 4.3 | 232.4 ± 4.5 | 0.1153 |
| Rbc (10^12/L) ± SD | 4.6 ± 0.04 | 4.3 ± 0.04 | <0.0001 |
Abbreviations: PCI: Percutaneous Coronary Intervention; dTRA: distal Radial Access; TRA: Transradial Approach
Table 1: Patient characteristics.
| dTRA% (N) | TRA% (N) | p value | |
|---|---|---|---|
| Successful puncture | 98.7 (150) | 99.3 (139) | 0.6106 |
| Access crossover | 1.3 (2) | 0.7 (1) | 0.6106 |
| Access time sec. | 38.6 ± 8.3 | 36.3 ± 7.8 | 0.0077 |
| Successful primary PCI | 100 | 100 | NA |
| RAO | 0 | 5.7 (8) | 0.0028 |
| EASY score hematoma | 15 (23) | 30.7 (43) | 0.0009 |
| Radial artery spasam | 17 | 14 | 0.952 |
| Hemostasis time | 34.5 ± 21.7 | 181 ± 11.8 | 0.0001 |
Abbreviations: PCI: Percutaneous Coronary Intervention; RAO: Radial Artery Occlusion; NA: Non-applicable; dTRA: distal Radial Access; TRA: Transradial Approach
Table 2: Study outcomes.
Discussion
In this study we used snuffbox puncture for dTRA, and there was no difference in procedural outcomes compared to conventional TRA. The success rate of puncture was 98.7% in dTRA and 99.3% in conventional TRA and primary PCI was successfully performed in all patients. The reason of crossover to another access site was due to loss of pulse at the site puncture after several attempts. The time of puncture was dTRA (38.6 ± 8.3 sec) vs. 36.3 ± 7.8 sec in conventional TRA. In the previous studies shown in Table 3, the success rate of puncture was 89%-100%. In these studies the patients were selected, and there was a small number of patients with STEMI.
| Study | No. of patients | Mean age, yr | Patients with STEMI | Success rate of the distal radial approach | Major bleeding |
|---|---|---|---|---|---|
| Kiemeneij, et al. [2] | 70 | 68 ± 11 | 9.0 (6/70) | 89.0 (62/70) | 0 (0) |
| Kim, et al. [7] | 150 | 66 ± 13 | 1.5 (2/132) | 88.0 (132/180) | 0 (0) |
| Lee, et al. [8] | 200 | 66 ± 12 | 8.5 (17/200) | 95.5 (191/200) | 0 (0) |
| Ziakas, et al. [9] | 49 | 64 ± 12 | 6.1 (3/49) | 89.8 (44/49) | 0 (0) |
| Soydan, et al. [10] | 54 | 59 ± 12 | 18.5 (10/54) | 100.0 (54/54) | 0 (0) |
| Valsecchi, et al. [11] | 52 | 68 ± 12 | No record | 90.0 (47/52) | 0 (0) |
| Norimatsu, et al. [12] | 74 | 70 ± 11 | 0 (0/74) | 91.9 (68/74) | 0 (0) |
Table 3: Patients with STEMI and success rate of the distal radial approach.
There are recently published studies that enrolled patients with STEMI, which showed that the success rate, and puncture time depended of operator experience [5,6]. In this study all operators had previous experience with over 100 dTRA procedures. Considering the STEMI setting, the success rate of dTRA (98.7%) and the time of puncture (38.6 sec) in this study are with acceptable results. Previous studies have reported no major complications in patients undergoing coronary angiography or PCI through the dTRA [2,7-10]. In this study all patients were loaded with clopidogrel 600 mg, unfractionated heparin 100 I.e/kg, and 5.9% of dTRA patients and 5% of the conventional TRA group received GP IIb/IIIa inhibitors. Despite the strong antithrombotic treatment, there were no cases of major bleeding requiring blood transfusion or surgical repair. The difference between two groups was in higher rate of local hematoma in the TRA group according to the EASY score (dTRA Grade I: 15.13%, Grade II: 0%, Grade III: 0%, Grade IV: 0%, TRA: Grade I: 22.9%, Grade II: 7.1%; Grade III: 0.7%, Grade IV: 0%). In previous publications the rate of radial artery occlusion in dTRA was from 0%-4% [2,11-13].
Conclusion
In this study the rate of radial artery occlusion is 0% in dTRA vs. 5.7% in TRA group, and the time of hemostasis was 30-60 min in dTRA group, which is a major predictor for the radial artery occlusion rate as shown in previous publications. dTRA is safe and successful in STEMI patients, when performed by experienced radial operators, with previous experience with dTRA. It is associated with lower rate of access site complications and early haemostasis in comparison with TRA.
Limitations of the Study
This study was conducted in an experienced high-volume transradial center, and all operators had previous experience with over 100 dTRA procedures in elective patients. Thus, our opinion is that cross-over rate and time of puncture could be higher if performed by less experienced operators.
Patent hemostasis was not performed and could be the reason for high rate of conventional access RAO.
Ethical Statement
The patient has given their written informed consent to publish their case, including publication of images.
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding
N/A
Author Contributions
All authors made substantial contributions to the conception or design of the work as well as to the acquisition, analysis, or interpretation of data for the work; participated in drafting the work or revising it critically for important intellectual content; approved the final version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Roffi M, Patrono C, Collet J-P, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 37(3): 267-315 (2016).
- Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI). EuroIntervention. 13(7): 851-857 (2017).
[CrossRef] [Google Scholar] [Pubmed]
- Nairoukh Z, Jahangir S, Adjepong D, et al. Distal radial artery access: The future of cardiovascular intervention. Cureus. 12(3): e7201 (2020).
[CrossRef] [Google Scholar] [Pubmed]
- Bertrand OF, de Larochellière R, Rodés-Cabau J, et al. Early Discharge after transradial stenting of coronary arteries study investigators. A randomized study comparing same-day home discharge and abciximab bolus only to overnight hospitalization and abciximab bolus and infusion after transradial coronary stent implantation. Circulation. 114(24): 2636-43 (2006).
[CrossRef] [Google Scholar] [Pubmed]
- Kim Y, Lee JW, Lee SY, et al. Feasibility of primary percutaneous coronary intervention via the distal radial approach in patients with ST-elevation myocardial infarction. Korean J Intern Med. 36(S1): S53-S61 (2021).
[CrossRef] [Google Scholar] [Pubmed]
- Lee OH, Kim Y, Son NH, et al. Comparison of distal radial, proximal radial, and femoral access in patients with ST-Elevation myocardial infarction. J Clin Med. 10(15): 3438 (2021).
- Kim Y, Ahn Y, Kim I, et al. Feasibility of coronary angiography and percutaneous coronary intervention via left snuffbox approach. Korean Circ J. 48(12): 1120-1130 (2018).
[CrossRef] [Google Scholar] [Pubmed]
- Lee JW, Park SW, Son JW, et al. Real-world experience of the left distal transradial approach for coronary angiography and percutaneous coronary intervention: A prospective observational study (LeDRA). EuroIntervention. 14(9): e995-e1003 (2018).
[CrossRef] [Google Scholar] [Pubmed]
- Ziakas A, Koutouzis M, Didagelos M, et al. Right arm distal transradial (snuffbox) access for coronary catheterization: Initial experience. Hellenic J Cardiol. 61(2): 106-109 (2020).
[CrossRef] [Google Scholar] [Pubmed]
- Soydan E, Akın M. Coronary angiography using the left distal radial approach: An alternative site to conventional radial coronary angiography. Anatol J Cardiol. 19(4): 243-248 (2018).
[CrossRef] [Google Scholar] [Pubmed]
- Valsecchi O, Vassileva A, Cereda AF, et al. Early clinical experience with right and left distal transradial access in the anatomical snuffbox in 52 consecutive patients. J Invasive Cardiol. 30(6): 218-223 (2018).
[Google Scholar] [Pubmed]
- Norimatsu K, Kusumoto T, Yoshimoto K, et al. Importance of measurement of the diameter of the distal radial artery in a distal radial approach from the anatomical snuffbox before coronary catheterization. Heart Vessels. 34(10): 1615-1620 (2019).
[CrossRef] [Google Scholar] [Pubmed]
- Pancholy SB, Patel TM. Effect of duration of hemostatic compression on radial artery occlusion after transradial access. Catheter Cardiovasc Interv. 79(1): 78-81 (2012).
[CrossRef] [Google Scholar] [Pubmed]