Case Report - Interventional Cardiology (2020) Volume 12, Issue 5
Complex Percutaneous Coronary Intervention in COVID-19 and Acute Coronary Syndrome
- Corresponding Author:
- Juan Guzmán Olea
Department of Interventional Cardiology
Hospital de Especialidades Puebla
Instituto Mexicano del Seguro Social, México
E-mail: dr.jguzmanolea@gmail.com
Received Date: August 05, 2020, Accepted Date: August 19, 2020, Published Date: August 26, 2020
Abstract
A 53-year-old male was admitted with acute coronary syndrome and COVID-19 pneumonia. Given the persistence of post-infarction angina despite optimal anti-ischemic therapy, he was presented to the Interventional Cardiology department, coronary angiography revealed critical lesions in the right coronary artery, including bifurcation, so we successfully performed a complex percutaneous coronary intervention.
Keywords
Acute myocardial infarction/STEMI; Percutaneous Coronary Intervention Complex; Stenting technique; COVID-19
Introduction
Severe acute respiratory syndrome Coronavirus-2 (SARS- CoV-2), a novel coronavirus, has alarmed the health care communities across the world in a very short span of time posing an unprecedented challenge. The patients with this disease usually present with features of respiratory illness. Rarely do they have acute coronary syndrome on arrival. Studies have shown that Covid-19 infection can worsen existing cardiovascular problems or can precipitate new cardiovascular problems. Acute ST elevation myocardial infarction (STEMI) is a medical emergency which needs immediate coronary reperfusion [1]. Here, we report a 53-year-old male that was diagnosed with acute coronary syndrome and COVID-19 pneumonia underwent to complex percutaneous coronary intervention.
Case Presentation
A 53-year-old male, without any modifiable cardiovascular risk factors or cardiovascular history. 3 days before admission, presented oppressive chest pain of more than 20 minutes span accompanied by dyspnea and lipothymia, without receiving any medical attention. On July 8th, 2020 he was admitted to our emergency room for presenting typical angina again, however he also had anosmia, asthenia, adynamia and of 85-89% oxygen saturation.
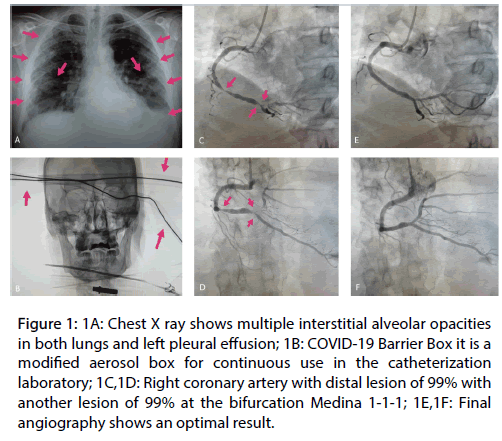
A resting 12-lead electrocardiogram was performed which revealed evolving changes of inferior ST elevation myocardial infarction. Cardiac biomarkers were elevated troponin 9 ng/ml. Echocardiogram showing basal inferior and basal inferolateral hypokinesia with left ventricle ejection fraction of 43%. Chest X ray was performed, which documented multiple interstitial alveolar opacities in both lungs and left pleural effusion (Figure 1A). A computed tomography scan of the chest was performed, showing a pulmonary parenchyma with a ground glass pattern located centrally and predominantly peripherally, involving all the lobes of both lungs and immediate changes of alveolar consolidation at the level of the lower lobes bilaterally, concluding atypical pneumonia by Coronavirus disease-2019 (COVID-19).
Figure 1: 1A: Chest X ray shows multiple interstitial alveolar opacities in both lungs and left pleural effusion; 1B: COVID-19 Barrier Box it is a modified aerosol box for continuous use in the catheterization laboratory; 1C,1D: Right coronary artery with distal lesion of 99% with another lesion of 99% at the bifurcation Medina 1-1-1; 1E,1F: Final angiography shows an optimal result.
Given the persistence of post-infarction angina despite optimal anti-ischemic therapy, he was presented to the Interventional Cardiology department. We decided to perform coronary angiography, so all medical staff wore the appropriate personal protective equipment and, for the patient the use of our COVID-19 Barrier Box, which is a modified aerosol box for continuous use in the catheterization laboratory (Figure 1B). A right radial approach was performed and the coronary angiogram revealed a left main coronary artery and circumflex normal artery, left anterior descending coronary artery intermediate lesion of 60% in the midsegment, right coronary artery with distal lesion of 99% with another lesion of 99% at the bifurcation with the posterior descending artery and posterolateral branch Medina 1-1-1, both vessels of adequate diameter (Figures 1C,1D). We decided to treat the most distal lesion with bifurcation technique, due to the context of the patient being COVID-19 positive, so a reverse T technique was used for being quick and simple. A Balance Middle Weight Universal (BMW) 0.014-inch guidewire (Abbott Vascular, Santa Clara, CA, USA) was passed distal to the posterolateral branch and Runthrough floppy 0.014-inch guidewire (Terumo) was passed distal to the posterior descending artery.
The posterolateral branch and distal right coronary artery were predilated with 2.0 x 15 mm compliant balloon at 18 atmospheres (atm), then a 2.5 x 16 mm Synergy Stent (Boston Scientific) was placed in the distal right coronary arteria toward posterior descending artery at 18 atm. After that, the BMW guidewire recrossed the posterolateral branch and non-compliant balloon 2.0 x 15 mm was advanced to post dilated the struts in ostium, after that a 2.25 x 20 mm Synergy stent (Boston Scientific) was placed in the ostium of the posterolateral branch at 18 atm, kissing balloon was performed and finally proximal optimization technique with non-compliant balloon 3.0 x 8 mm, then a 3.5 x 18 mm Resolute Onyx stent (Medtronic) was placed in the distal segment at 16 atm with TIMI3 and TMP3 result , with optimal outcome, without any complications and all the medical staff remained virus contagion free. (Figures 1E,1F).
After the procedure the patient was transferred to COVID-19 unit where he remained symptom free with improvement and resolution of pneumonia.
Discussion
The COVID-19 outbreak is an unprecedented global public health challenge. Since the end of December 2019, when the first cases of SARS-Cov-2 infection were detected in Wuhan, China, the disease has spread out exponentially [2]. On January 30th, 2020 the World Health Organization declared COVID-19; the disease caused by the novel coronavirus, as a public health emergency of international concern and later officially upgraded it to a global pandemic. More than 2,790,000 confirmed cases from more than 180 countries and more than 195,000 deaths have been documented worldwide [3]. Mexico had registered 356,255 cases and 40,400 deaths by July 21st, 2020.
SARS-CoV-2 causes not only viral pneumonia, but has major implications for the cardiovascular system. Patients with cardiovascular risk factors including male sex, advanced age, diabetes, hypertension and obesity, as well as patients with established cardiovascular and cerebrovascular disease have been identified as particularly vulnerable populations with increased morbidity and mortality when suffering from COVID-19 [4].
Moreover, a considerable number of patients may develop cardiac injury in the context of COVID- 19 which portends an increased risk of in-hospital mortality. Aside from arterial and venous thrombotic complications presenting as acute coronary syndromes and venous thromboembolism, myocarditis plays an important role in patients with acute heart failure. Besides COVID-19 disease may trigger destabilization of chronic cardiovascular disease. Owing to redistribution of health care resources, access to emergency treatment including reperfusion therapy may be affected depending on the severity of the epidemic at a local level. This is further aggravated by increasing concerns of delayed presentation of cardiovascular emergencies as patients are afraid to seek medical attention during the pandemic [4].
In case of acute coronary syndrome type ST elevation myocardial infarction, primary percutaneous coronary intervention remains the preferred option for reperfusion [5]. In our hospital we have a dedicated COVID-19 catheterization laboratory 24/7 hours available for the intervention of acute coronary syndromes and the catheterization laboratory staff wears level III personal protective equipment. We know that any intubation, suction, or cardiopulmonary resuscitation may cause aerosol dispersion of respiratory secretions with increased likelihood of exposure to the staff; for this reason, we use our COVID-19 Barrier Box, and all patients entering the catheterization laboratory must wear a surgical mask [6,7].
The treatment of coronary bifurcation lesions comprises from 15% to 20% of all percutaneous interventions. These lesions form part of the group of complex lesions and their treatment poses a major technical challenge. So far, there are no reported cases with complex percutaneous coronary intervention with COVID-19 and acute coronary syndrome. In this article we report a 53-year-old male with acute coronary syndrome and COVID-19 pneumonia with critical lesions in the right coronary artery, including bifurcation, so we successfully performed a complex percutaneous coronary intervention using the most simple and quick technique.
Conclusion
We conclude that during the outbreak of Coronavirus disease 2019 complex percutaneous coronary intervention like bifurcations in an acute context it is feasible and can be safe using the simplest technique and adequate protection equipment for catheterization laboratory staff and for the patient.
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding
There is no financial support/grant for this study.
References
- Siddamreddy S, Thotakura R, Dandu V, et al. Corona Virus Disease 2019 (COVID-19) Presenting as Acute ST Elevation Myocardial Infarction. Cureus. 12(4): e7782 (2020).
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in china, 2019. N Eng J Med. 382: 727-733 (2020).
- Ullah W, Saeed R, Sarwar U, et al. COVID.19 complicated by acute pulmonary embolism and right-sided heart failure. JACC Case Rep. 2(9): 1379-1382 (2020).
- Daniele A, Elena A, Emanuele B, et al. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. Eur Heart J. (2020).
- Gambaro A, Ho HH, Kaier TE, et al. Management of acute coronary syndrome in the COVID-19 Era Voices from the global cardiology community. JACC Case Rep. 2(9): 1429-1432 (2020).
- Juan GO, Elizabeth SR. COVID-19 barrier box in cardiac catheterization. (2020).
- Bettari L, Pero G, Maiandi C, et al. Exploring personal protection during high-risk pci in a covid-19 patient impella cp mechanical support during ulmca bifurcation stenting. JACC Case Rep. 2(9): 1279-1283 (2020).