Review Article - Interventional Cardiology (2023)
COPD as a major risk factor for cardiovascular disease
- *Corresponding Author:
- Alberto Calderon Montero
Primary Care Health Center Doctor Pedro Lain Entralgo, Madrid, Spain
E-mail: acalderonmontero@gmail.com
Received date: 06-Mar-2023, Manuscript No. FMIC-23-91113; Editor assigned: 08-Mar-2023, PreQC No. FMIC-23-91113(PQ); Reviewed date: 22-Mar-2023, QC No. FMIC-23-91113; Revised date: 29-Mar-2023, Manuscript No. FMIC-23-91113(R); Published date: 07-Apr-2023, DOI: 10.37532/1755-5310.2023.15(S16).407
Abstract
Chronic Obstructive Pulmonary Disease (COPD) is the fifth leading cause of mortality in the Western world. Approximately 35%-40% is due to cardiovascular complications in the broad spectrum of heart failure, atherosclerotic disease, arrhythmias, and sudden death. The underlying pathophysiological substrate is an alteration in the functioning of the cardiopulmonary axis by different mechanisms. Despite the evidence, COPD is not included as a specific entity in the different cardiovascular risk tables and calculators, which leads to an underestimation of risk and insufficient treatment, both in the field of inhaled bronchodilators and drugs. Commonly used in cardiovascular diseases. Recent intervention studies have revealed how cardiovascular complications exceed respiratory complications in some populations with COPD, and how new strategies are being developed with inhaled bronchodilator drugs potentially capable of modifying the course of the disease.
Keywords
COPD; Cardiovascular risk factors; Cardiovascular events; Triple therapy inhalation; Cardiopulmonary axis
Abbreviations
AF: Atrial Fibrillation; AMI: Acute Myocardial Infarction; BBs: Beta-Blockers; BNP: Brain Natriuretic Peptide; CKD: Chronic Kidney Disease; COPD: Chronic Obstructive Pulmonary Disease; CRP: C-Reactive Protein; CVD: Cardiovascular Disease; CVR: Cardiovascular Risk; EMPHASIS-HF: Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure; ETHOS: Efficacy and Safety of Triple Therapy in Obstructive Lung Disease; EUROSCOP: European Respiratory Society Study on Chronic Obstructive Pulmonary Disease; GOLD: Global Initiative for chronic obstructive pulmonary disease; HF: Heart Failure; ICS: Inhaled Corticosteroid; LABA: Long-Acting-β2-Agonist; LAMA: Long-Acting Muscarinic Antagonist; MACE: Mayor Cardiovascular Events; MRAs: Mineralocorticoid Receptor Antagonists; NNT: Number of Patients to Treat; RAAS: Renin-Angiotensin Aldosterone System; RALES: Randomized Aldactone Evaluation Study; SCD: Sudden Cardiac Death; SGLT2: Sodium-glucose co-transporter type 2 inhibitors; SUMMIT: Study to Understand Mortality and Morbidity; COPD VA: Ventricular arrhythmias
Introduction
The estimation of Cardiovascular Risk (CVR) is one of the main activities of medical professionals to address the prevention and treatment of cardiovascular diseases. Since the early days of the Framingham cohorts, different scales and algorithms have been designed to estimate cardiovascular risk in populations and establish different strategies for both primary and secondary prevention. Likewise, the variables that have been incorporated into the different tables and algorithms have been changing as new evidence emerged. The Framingham risk tables incorporated the classic risk factors mainly for coronary diseases, such as age, arterial hypertension, gender, cholesterol levels, and smoking [1]. More recently, the SCORE risk estimate has been modified by stratifying four geographical areas in Europe, including a specific table for the population over 70 years of age that was not previously considered [2]. In addition, the current SCORE table estimates not only fatal coronary events but the 5- and 10-year risk of cardiovascular disease. Like the Framingham and other cardiovascular risk estimation tables [3], the variables included are mostly the classic risk factors with some variants. However, it is significant that pathologies as relevant to cardiovascular diseases as Chronic Kidney Disease (CKD) [4], are not always included in the estimation of cardiovascular risk. And in this sense, it is even more striking that Chronic Obstructive Pulmonary Disease (COPD) is not clearly defined as one of the main variables when estimating cardiovascular risk in the population [1-3].
Literature Review
COPD and cardiovascular disease
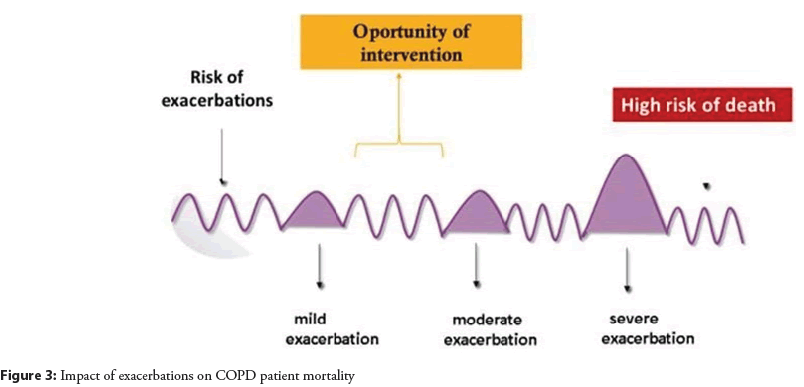
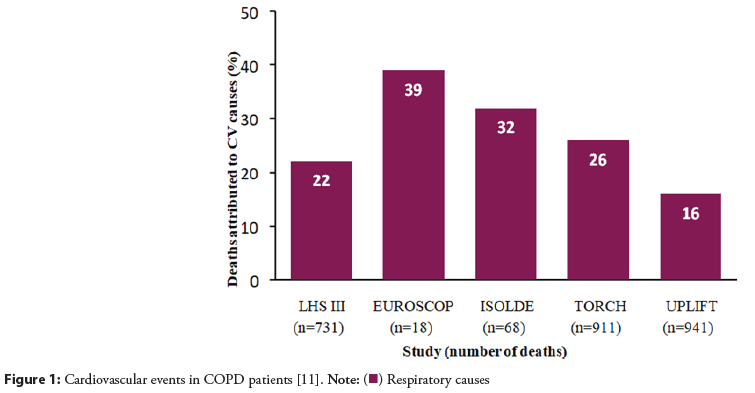
Unfortunately, until just a decade ago, COPD was considered a disease restricted to the lung territory and with little impact on other organic territories. In recent years, epidemiological evidence and experimental studies have revealed how COPD is a systemic disease with a low-intensity inflammatory pathophysiological basis, which increases during exacerbations [5,6]. This systemic activity entails the simultaneous affectation of other organs and especially the coronary and cardiovascular territory. It is estimated that at least 40% of COPD mortality is due to cardiovascular causes [7], though this figure may be underestimated. The results of the Lung Health Study have already shown how Cardiovascular Disease (CVD) is responsible for 42% of first admissions of COPD patients and 48% of readmissions [8]. Likewise, exacerbations are one of the main causes of cardiovascular events in these patients [9]. Even more, in a large meta-analysis including 27 studies [10], the risk of HF in COPD was 2.57 (95% CI 1.90-3.47), the relative risk of Acute Myocardial Infarction (AMI) in patients with moderate COPD is 1.40, and 3.00 in patients with severe disease compared with people without COPD and COPD is associated with an increased incidence of Ventricular Arrhythmias (VA), Atrial Fibrillation (AF) and Sudden Cardiac Death (SCD). Therefore, COPD is not only a risk factor for coronary heart disease and could affect all cardiovascular diseases. Data from observational and randomized studies show how cardiovascular mortality can reach up to 39% of all deaths in patients with COPD and how cardiovascular mortality in patients with moderate COPD exceeds mortality from lung cancer and respiratory causes (Figures 1 and 2) [11,12].
Figure 1: Cardiovascular events in COPD patients [11].
Note: ( ) Respiratory causes
) Respiratory causes
Based on all the evidence currently available, is no doubt that COPD must be considered a higher risk factor of cardiovascular complications and it is essential to include it in the risk estimation tables. It is true that the smoking habit is usually included in risk estimators, but it is no less true that the pathophysiology of COPD including other mechanisms dispose for cardiovascular disease in other ways than the dependents directly of tobacco. Consequently, it is necessary to know and understand the relationship between COPD and cardiovascular disease as an alteration of the cardiopulmonary axis [13], and thus adopt a new vision in the estimation of cardiovascular risk. And in that line, it is essential to keep in mind those therapeutic measures that can stabilize, delay and, where appropriate, reverse the alterations of the cardiopulmonary axis at least partially.
Cardiopulmonary axis alterations
Regardless of risk factors that COPD and cardiovascular disease share, such as smoking habit, age, cardiovascular risk factors, environmental pollution, overweight, and family history of CVD, some relevant factors are intrinsic COPD mechanisms.
Systemic low-intensity inflammation, moderate systemic inflammation during exacerbations, pulmonary insufflation, endothelial dysfunction, platelet alterations, and hypoxia plays a relevant role in the relationship between COPD and cardiovascular disease [13]. Biomarkers such as C-Reactive Protein (CRP) and fibrinogen are increased in COPD and are related to disease severity and increased morbidity and mortality. Other inflammatory markers of CVD such as troponin and pro-BNP are also elevated, both during the stable phase as well as exacerbations [14]. Data from the SUMMIT study showed a ten-fold increase in the risk of suffering a cardiovascular event after exacerbation (RR 9.9, 95% CI 6.6-14.9) [15]. In addition, thrombocytosis on admission is related to hospital mortality and mortality in the first year. Hypoxia, which is one of the major clinical consequences of COPD, enhances systemic inflammation, oxidative stress, fat cell production, and cell adhesion to the endothelium [16], all of which are predisposing factors for CVD. Furthermore, hypoxia reduces oxygen supply to the myocardium, predisposing it to coronary ischemia and type 2 AMI [17]. In older patients, low levels of lymphocytes have been observed to be associated with increased cardiovascular mortality due to heart failure [18]. Likewise, endothelial dysfunction, hypoxia, and neuroadrenergic activation common in COPD and obstructive sleep apnea syndrome are associated with increased development of atherosclerosis disease [19].
Therapeutic strategies that act on the cardiopulmonary axis
The reduction of all-cause mortality and cardiovascular mortality in particular should therefore be one of the priorities when considering the treatment of the patient with COPD. This treatment should be approached from a double perspective:
a) Optimize bronchodilator treatment with an effect on the cardiopulmonary axis to prevent cardiovascular complications.
b) Adapt cardiovascular treatment to the characteristics of the patient with COPD.
Bronchodilator treatment with effect on mortality: Most of the studies carried out on patients with COPD have been based on demonstrating the benefit of inhaled therapy on symptoms, lung function, exacerbations, and quality of life. Only recently have hard variables such as all-cause mortality and cardiovascular mortality begun to be considered as treatment goals.
Monotherapy and dual therapy have been evaluated with respect to all-cause mortality in observational and randomized studies with conflicting results. Two observational studies showed a reduction in all-cause mortality when dual therapy included an Inhaled Corticosteroid (ICs) combined with a Long-Acting-β2-Agonist (LABA), especially in those patients with prior exacerbations (HR 0.48, CI 95% 0.31-0.73 and HR 0.83, CI 95% 0.72-0.97 respectively) [20,21]. Randomized studies, however, did not demonstrate homogeneous results in terms of all-cause mortality reduction, including the SUMMIT study in which patients had a high cardiovascular risk profile (HR 0.88, 95% CI 0.74-1.04) [22].
In recent years, new trials have been published to test the possible benefit of triple bronchodilator therapy compared to dual bronchodilator therapy on all-cause mortality and cardiovascular mortality [23,24]. In a pooled analysis of three studies, a nonstatistically significant benefit on all-cause mortality was found for ICs-containing versus non-ICS-containing regimens (HR 0.71, 95% CI 0.50-1.02) [23]. However, an interesting aspect was that, when analyzed by causes of mortality, as opposed to respiratory mortality, ICs- regimens did significantly reduce nonrespiratory mortality (HR 0.62, 95%CI 0.43-0.97) [25]. Given that a significant percentage of non-respiratory mortality is of cardiovascular origin, it could be suggested that triple therapy has a beneficial effect on cardiovascular mortality.
This hypothesis has been at least partially endorsed in the ETHOS study. Briefly, the patients included in the study were classified as moderate to very severe with previously moderate or severe exacerbations in the year prior to inclusion. The study evaluated two types of triple therapy (budesonide/glycopyrronium/ formoterol) in which the IC dose varied (budesonide 320 and budesonide 160) versus dual therapy and confirmed a reduction in all-cause mortality when comparing triple therapy with budesonide 320 versus dual therapy LABA+LAMA (Long-Acting Muscarinic Antagonist) (HR 0.51, CI 95% 0.33-0.80). Especially interesting was that cardiovascular mortality was also reduced with triple therapy with budesonide 320 μg (0.5%) versus LABA/ LAMA (1.4%) and with triple therapy budesonide 160 μg (0.8%) and was like dual therapy with LABA/ICS (0.5%) [24].
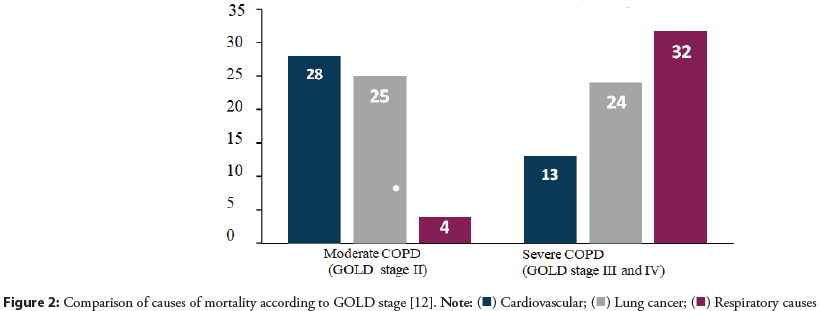
Different mechanisms may explain the beneficial effects of triple therapy on cardiovascular mortality in the ETHOS study. First, triple therapy has been shown to reduce exacerbations and pulmonary function and as a result, improve cardiac hemodynamic parameters, which indirectly could reduce cardiovascular comorbidity [23-26]. The frequency and intensity of exacerbations are directly related to the prognosis of the patient with COPD (Figure 3). Second, triple therapy also improves hypoxemia in COPD patients, which reduces pulmonary territory vascular resistance, decreases right ventricular afterload, and increases cardiac output [27]. Third, the presence of corticosteroids in triple therapy could reduce systemic inflammatory activity and the atherogenic biomarker cascade. The reduction in cardiovascular mortality in ETHOS was superior in the budesonide 320 μg arm compared with budesonide 160 μg, suggesting a dose-dependent relationship with inhaled corticosteroids, consistent with the results of the EUROSCOP study [28]. Likewise, the effect of triple therapy on pulmonary hyperinflation improves cardiac hemodynamics as another possible additional mechanism of cardiovascular protection.
Figure 3:Impact of exacerbations on COPD patient mortality
Therefore, cardiovascular mortality in COPD can be considered to have a multi- etiological origin. And as occurs in other cardiovascular pathologies such as heart failure or type 2 diabetes mellitus, triple therapy acts on the different alterations of the cardiopulmonary axis by different mechanisms, which produces a global effect greater than the sum of the individual therapies.
The importance of intervention with triple therapy has a double perspective from the cardiovascular point of view:
a) Firstly, the greatest benefits are obtained in patients in less advanced stages of COPD, which suggests that treatment should be instituted early, especially in those patients with a history of exacerbations and high risk and/or cardiovascular comorbidity.
b) The results of the studies with triple therapy allow for estimating the efficiency of the intervention by estimating the Number of Patients to Treat (NNT) to prevent events in comparison with other interventions widely implemented in the cardiovascular field (Table 1).
| Disease | Intervention | Duration (years) | Outcome | NNT (CI 95%) | Reference |
|---|---|---|---|---|---|
| COPD | FF/UMC/VI vs dual therapy | 1 | All-cause mortality | 145 | [23] |
| COPD | BD/GLP/FOR vs dual therapy | 1 | All-cause mortality | 105 | [24] |
| Primary prevention | Atorvastatin vs placebo | 5 | MACE | [29] | |
| Low risk | 146 (117-211) | ||||
| High risk | 53 (39-88) | ||||
| Diabetes | Dulaglutida vs placebo | 5,4 | MACE | 67 (38-802) | [30] |
| Diabetes | Empaglifozina vs placebo | 3,1 | MACE | 61 (31-2152) | [31] |
| Diabetes | Metformin vs diet | 10 | All-cause mortality | 141 | [32] |
| Tobacco | Smokers vs non-smokers | 14,5 | All-cause mortality | 196 | [33] |
Note: COPD: Chronic Obstructive Pulmonary Disease; NNT Number of patients Need to Treat; MACE: Mayor Cardiovascular Events (cardiovascular mortality, non-fatal myocardial infarction, non-fatal stroke); CI Confidence Interval; FF Fluticasone; UMC: Umeclidinium; VI: Vilanterol; BD: Budesonide; GLP: Glycopirronium; FOR: Formoterol.
Table 1: Number of patients Needed to Treat (NNT) for preventing cardiovascular events or all-cause mortality.
Optimization of cardiovascular treatment in the patient with COPD: The prevention and treatment of cardiovascular disease in patients with COPD have often been controversial. On the one hand, the selection criteria for patients in randomized cardiovascular studies have frequently excluded patients with COPD, even more so in moderate or more advanced stages. On the other hand, observational studies and clinical practice conditions show that cardiovascular drugs are underused in these patients [34]. This may be another additional cardiovascular risk factor of the high cardiovascular morbidity and mortality of the patient with COPD, so it is essential to optimize treatments in this field.
Beta-Blockers (BBs) are indicated in patients with cardiovascular disease regardless of the presence of COPD according to the ESC guidelines. However, they are underused based on the risk of bronchospasm. There is abundant evidence that this is not the case with selective beta-1 blockers such as bisoprolol, carvedilol, metropolol, or atenolol, which have a 20-fold greater affinity for beta-1 receptors than beta-2 receptors.
Different studies show how selective BBs do not act negatively on the different pathophysiological mechanisms involved in cardiovascular complications in COPD, such as exacerbations, inflammation, worsening lung function, pulmonary hyperinflation, or hypoxemia [35,36]. Likewise, maintenance of beta-blocker treatment during hospitalization does not increase the length of stay or in-hospital mortality [37]. Consequently, they should be used under the same conditions as in patients without COPD, and thus avoid increasing the cardiovascular risk of these patients due to under treatment.
Blockade of the Renin-Angiotensin Aldosterone System (RAAS) may have a beneficial effect by inhibiting inflammatory products that contribute to pulmonary fibrosis. In general, AT2 receptor blockers should be preferred because of their lower incidence of coughing. A sub analysis of the PARADIGM-HF study has recently been published showing that the benefit of sacubitril valsartan versus enalapril is similar in patients with COPD and without COPD, so patients with COPD may benefit from this dual RAAS blockade [38].
The potential benefits of statins in patients with COPD are controversial considering the existing evidence, but they appear to be safe and do not adversely affect pulmonary function.
Mineralocorticoid Receptor Antagonists (MRAs) are drugs of first choice in patients with HF and reduced ejection fraction, a common comorbidity in patients with COPD. A pooled analysis of the RALES (spironolactone) and EMPHASIS-HF (eplerenone) studies showed that the benefits of MRAs versus placebo on the primary endpoint of cardiovascular mortality and HF hospitalization are consistent between patients with and without COPD (RR 0.66 and 0.65, interaction p 0.93) [39].
Finally, a recent meta-analysis of SGLT2i receptor inhibitors (SGLT2i) including 1,292 patients with COPD showed that SGLT2i versus placebo reduced the composite endpoint of cardiovascular mortality and HF hospitalization by 28% (RR=0.72, 95% CI 0.60-0.86) [40].
Conclusion
Cardiovascular complications account for approximately more than 40% of morbidity and mortality in patients with COPD, especially in those with a moderate stage of the disease (stage II GOLD). And it is very important to know how they affect the broad spectrum of heart failure, arrhythmias, ischemic heart disease, stroke, and sudden death. Despite this, COPD is not considered in the cardiovascular risk tables, which should be modified, since it leads to an underestimation of cardiovascular risk and, as a consequence, a less proactive attitude with the consequent undertreatment. For this reason, it is essential to sensitize the group of doctors who treat these patients about the importance of implementing bronchodilator treatments, preferably triple therapy, early, as well as using cardiovascular drugs in similar conditions to patients without COPD.
References
- D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The framingham heart study. Circulation. 117(6): 743-53 (2008).
- SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 42(25): 2439-2454 (2021).
- NICE guidelines. Cardiovascular disease: Risk assessment and reduction, including lipid modification. (2014).
- Jankowski J, Floege J, Fliser D, et al. Cardiovascular disease in chronic kidney disease: Pathophysiological insights and therapeutic options. Circulation. 143(11): 1157-1172 (2021).
- André S, Conde B, Fragoso E, et al. COPD and cardiovascular disease. Pulmonology. (3): 168-176 (2019).
- Schmidt SA, Johansen MB, Olsen M, et al. The impact of exacerbation frequency on mortality following acute exacerbations of COPD: A registry-based cohort study. BMJ Open. 4(12): e006720.
- Halpin DM, Miravitlles M, Metzdorf N, et al. Impact and prevention of severe exacerbations of COPD: A review of the evidence. Int J Chron Obstruct Pulmon Dis. 12: 2891-2908 (2017).
- Anthonisen NR, Connett JE, Enright PL, et al. Hospitalizations and mortality in the lung health study. Am J Resp Crit Care Med. 166: 333-339 (2002).
- Rothnie KJ, Connell O, Müllerová H, et al. Myocardial infarction and ischemic stroke after exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 15(8): 935-946 (2018).
- Chen W, Thomas J, Sadatsafavi M, et al. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis. Lancet Respir Med. 3: 631-639 (2015).
- Christenson SA, Smith BM, Bafadhel M, et al. Chronic obstructive pulmonary disease. Lancet. 399(10342): 2227-2242 (2022).
- Mannino DM, Doherty DE, Buist AS, et al. Global initiative on Obstructive Lung Disease (GOLD) classification of lung disease and mortality: Findings from the Atherosclerosis Risk in Communities (ARIC) study. Respir Med. 100(1): 115-122 (2006).
- Calderón Montero A. Cardiopulmonary axis and cardiovascular mortality in patients with COPD. Semergen. 49(4): 101928 (2023).
- Pavasini R, Tavazzi G, Biscaglia S, et al. Amino terminal pro brain natriuretic peptide predicts all-cause mortality in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis. Chron Respir Dis. 14: 117-126 (2017).
- Kunisaki KM, Dransfield MT, Anderson JA, et al. Exacerbations of chronic obstructive pulmonary disease and cardiac events. a post hoc cohort analysis from the SUMMIT randomized clini- cal trial. Am J Respir Crit Care Med. 198: 51-57 (2018)
- Fisk M, McEniery CM, Gale N, et al. Surrogate markers of cardiovascular risk and chronic obstructive pulmonary disease. Hypertension. 71: 499-506 (2018).
- Goedemans L, Bax JJ, Delgado V, et al. COPD and acute myocardial infarction. Eur Respir Rev. 29: 190139 (2020).
- Acanfora D, Scicchitano P, Carone M, et al. Relative lymphocyte count as an indicator of 3-year mortality in elderly people with severe COPD. BMC Pulm Med. 18(1): 116 (2018).
- Ciccone MM, Scicchitano P, Mitacchione G, et al. Is there a correlation between OSAS duration/severity and carotid intima-media thickness? Respir Med. 106(5): 740-746 (2012).
- Soriano JB, Vestbo J, Pride NB, et al. Survival in COPD patients after regular use of fluticasone propionate and salmeterol in general practice. Eur Respir J. 20(4): 819-825 (2002).
- Di Martino M, Agabiti N, Cascini S, et al. The effect on total mortality of adding inhaled corticosteroids to long-acting bronchodilators for COPD: A real practice analysis in Italy. COPD. 13(3): 293-302 (2016).
- Mintz M, Barjaktarevic I, Mahler DA, et al. Reducing the risk of mortality in chronic obstructive pulmonary disease with pharmacotherapy: A narrative review. Mayo Clin Proc. 98(2): 301-315 (2023).
- Day NC, Kumar S, Criner G, et al. Single- inhaler triple therapy fluticasone furoate/umeclidinium/vilanterol versus fluticasone furoate/vilanterol and umeclidinium/vilanterol in patients with COPD: Results on cardiovascular safety from the IMPACT trial. Respir Res. 21:139. (2020).
- Martinez FJ, Rabe KF, Ferguson GT, et al. Reduced all- cause mortality in the ethos trial of budesonide/glycopyrrolate/formoterol for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 203: 553-564 (2021).
- Vestbo J, Fabbri L, Papi A, et AL. Inhaled corticosteroid containing combinations and mortality in COPD. Eur Respir J. 52(6): 1801230 (2018).
- Calverley PM, Celli BR, Crim C, et al. Risk of death and chronic obstructive pulmonary disease (COPD) hospitalization with fluticasone furoate containing therapy: post hoc subgroup analysis from the SUMMIT trial in patients with COPD and a history of exacerbation. Chest. 158(4): A1755-A1760 (2020).
- Morales DR, Lipworth BJ, Donnan PT, et al. Respiratory effect of beta-blockers in people with asthma and cardiovascular disease: Population- based nested case control study. BMC Med.15: 18 (2017).
- Pauwels RA, Löfdahl, CG, Laitinen LA, et al. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. N Engl J Med . 340(25): 1948-1953 (1999).
- Rossignol M, Michel Labrecque MI, Michel Cauchon M, et al. Number of patients needed to prescribe statins in primary cardiovascular prevention: Mirage and reality. Fam Pract. 35 (4): 376-382 (2018).
- erstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): A double-blind, randomised placebo-controlled trial. Lancet. 394(10193): 121-13 (2019).
- Zinman B, Wanner C, Lachi JM et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 373: 2117-2128 (2015).
- Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 352(9131): 854-865 (1998).
- Anthonisen NR, Skeans MA, Wise RA, et al.The effects of a smoking cessation intervention on 14.5-year mortality: A randomized clinical trial. Ann Intern Med. 142: 233-239 (2005).
- Leitao Filho FS, Choi L, Sin DD, et al. Beta-blockers in chronic obstructive pulmonary disease: The good, the bad and the ugly. Curr Opin Pulm Med. 27(2): 125-131 (2021).
- Gulea C, Zakeri R, Alderman V, et al. Beta-blocker therapy in patients with COPD: A sys-tematic literature review and meta-analysis with multiple treatment comparison. Respir Res. 22:64 (2021).
- Du Q, Sun Y, Ding N, et al. Beta-blockers reduced the risk of mortality and exacerbation in patients with COPD: A meta-analysis of observational studies. PLoS One. 9:e113048 (2014).
- Yang YL, Xiang ZJ, Yang JH, et al. Association of β-blocker use with survival and pulmonary function in patients with chronic obstructive pulmonary and cardiovascular disease: A systematic review and meta-analysis. Eur Heart J. 41: 4415-44122 (2020).
- Ehteshami-Afsar S, Mooney L, Dewan P, et al. Clinical characteristics and outcomes of patients with heart failure with reduced ejection fraction and chronic obstructive pulmonary disease: Insights from paradigm-HF. J Am Heart Assoc. 2021;10: e019238 (2021).
- Yeoh SE, Dewan P, Serenelli M, et al. Effects of mineralocorticoid receptor antagonists in heart failure with reduced ejection fraction patients with chronic obstructive pulmonary disease in EMPHASIS- HF and Rales. Eur J Heart Fail. 24: 529-538 (2022).
- Patoulias P, Papadopoulos C, Fragakis N, et al. Meta-analysis assessing the cardiovascular efficacy of sodium-glucose co-transporter-2 inhibitors in patients with chronic obstructive pulmonary disease. Am J Car- diol. 174: 188-189 (2022)
 ) Cardiovascular; (
) Cardiovascular; ( )
)