Case Report - Interventional Cardiology (2017) Volume 9, Issue 5
Coronary artery aneurysms in the elderly: Case report
- Corresponding Author:
- Ricardo J. Torres
Doctors Hospital at Renaissance, Edimburg, Texas, USA
Tel: +18324346891
E-mail: ricardotorresmd@gmail.com
Submitted: 31 August 2017; Accepted: 03 October 2017; Published online: 09 October 2017
Abstract
Aneurysmal coronary disease or ectasia is defined as the dilation of a vessel at least 1.5 times the diameter of a normal adjacent segment. The prevalence of the disease has been encountered in up to 5% of patients undergoing angiographies. Atherosclerotic heart disease has been mentioned as the most common etiologic factor involved in the development of coronary aneurysms. We present a case of a 73-year-old male with a history of hypertension, dyslipidemia, and coronary artery disease with a myocardial infarction 20 years ago that was evaluated for dyspnea on mild exertion. There was no history of chronic lung disease. A left heart catheterization was done. This revealed a fusiform 14 mm aneurysm involving the whole left main (LM) coronary artery and multiple smaller aneurysms on the right coronary artery (RCA); there was also an 80% stenosis of the mid left anterior descending artery (LAD), a totally occluded left circumflex in its mid portion, and diffuse stenosis of the terminal branches of the RCA. The left ventricular ejection fraction was 35-40%. A single-vessel bypass grafting procedure with the left inferior mammary artery (LIMA) to the LAD was done. No surgical intervention was performed to the LM aneurysm due to the fusiform anatomy. On subsequent follow up the patient showed improvement of the symptoms and continued medical treatment with aspirin, statins, angiotensin receptor blockers and beta-blockers. The subsequent ejection fraction measured by echocardiography four months later, improved to 40-45%.
Keywords
Coronary aneurysm; Coronary artery disease; Cardiac catheterization; Coronary artery bypass grafting
Introduction
Aneurysmal coronary disease or ectasia is defined as the dilation of a vessel at least 1.5 times the diameter of a normal adjacent segment [1]. It has been suggested that the presence of aneurysms causes sluggish blood flow which increases the risk of ischemic manifestations and myocardial infarction depending on the presence and severity of coexisting stenotic lesions [2]. The prevalence of the disease has been encountered in up to 5% of patients undergoing angiographies1 with an overall incidence of 1.4% [3]. The right coronary artery (RCA) is the most commonly affected vessel, followed by the left circumflex (LCX) or left anterior descending (LAD) depending on the study. Involvement of three vessels or the left main coronary (LM) is rare [4-7]. Atherosclerotic heart disease has been mentioned as the most common etiologic factor involved in the development of coronary aneurysms. Other causes that may lead to coronary artery aneurysm formation include coronary angioplasty (with balloon, atherectomy, laser angioplasty, etc), congenital anomalies, mycotic aneurysm, Kawasaki disease, connective tissue disorders (eg, Marfan syndrome and Ehlers- Danlos syndrome), polyarteritis nodosa, Takayasu arteritis, syphilis, metastatic tumors and trauma [2,8,9]. Histological examination of atherosclerotic CAAs has found hyalinization and lipid deposition leading to disturbance of the intimal and medial layers of the vessel wall, and destruction of the muscular elastic components. Weakening of the vessel wall and decreased elasticity ultimately reduce the tolerance of the vessel to intraluminal pressures of blood flow, predisposing it to subsequent dilatation and aneurysm formation [10-12].
Case Description
A 73-year-old white male with a history of hypertension, dyslipidemia, and coronary artery disease with a myocardial infarction 20 years ago, was referred by his primary care physician to our clinic for evaluation and management of dyspnea on mild exertion. There was no history of chronic lung disease and acute problems were excluded. The physical examination showed a man with a BMI of 35, and bilateral lower extremity venous insufficiency. An ECG showed a possible old inferior MI, poor R-wave progression and non-specific ST-T wave abnormalities. On a follow up consult due to persistent symptoms he underwent myocardial perfusion imaging (MPI) that showed an abnormal area of inducible ischemia in the anterior wall.
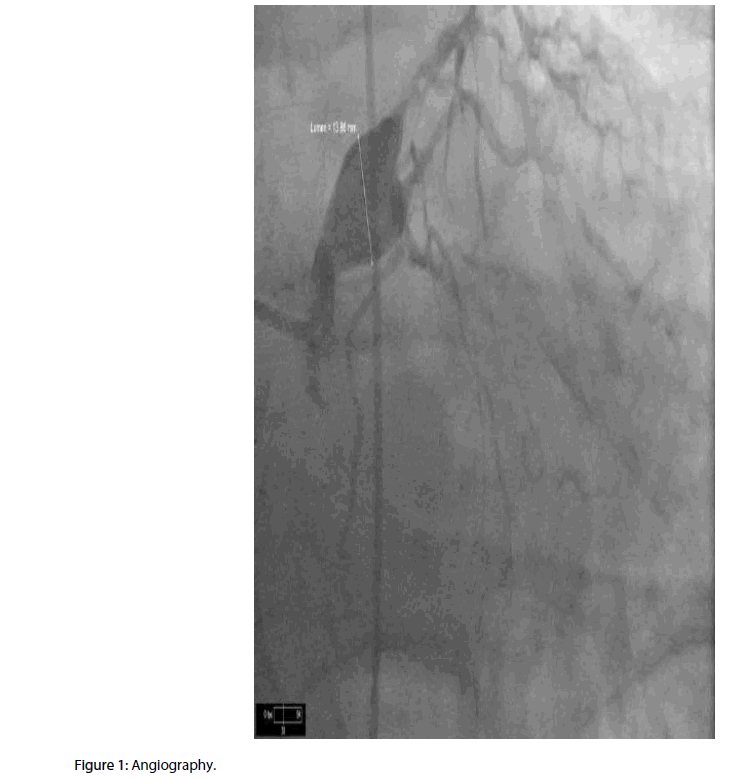
A left heart catheterization was done. This revealed a fusiform 14 mm aneurysm involving the whole left main (LM) coronary artery and multiple smaller aneurysms on the right coronary artery (RCA); there was also an 80% stenosis of the mid left anterior descending artery (LAD), a totally occluded left circumflex in its mid portion, and diffuse stenosis of the terminal branches of the RCA. The left ventricular ejection fraction was 35-40%.
A single-vessel bypass grafting procedure with the left inferior mammary artery (LIMA) to the LAD was decided because the RCA and circumflex targets were extremely poor. No surgical intervention was performed to the LM aneurysm due to the anatomy of the aneurysm. There were no complications during the surgery or in the immediate post-operative period. On subsequent follow up, one week, two months and one year after the procedure, the patient showed improvement of the symptoms and continued medical treatment with aspirin, statins, angiotensin receptor blockers and beta-blockers. The subsequent ejection fraction measured by echocardiography four months later improved to 40-45% (Figure 1).
Discussion
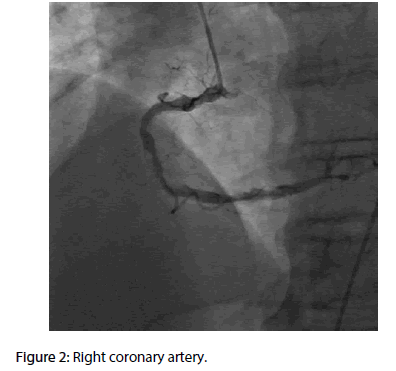
In the majority of cases, coronary aneurysms are asymptomatic, but they can also present with angina pectoris, myocardial infarction, sudden death, fistula formation, cardiac tamponade, compression of surrounding structures, or congestive heart failure [2,9,13-15]. The presentation depends on the size and number of aneurysm, and coexisting atherosclerotic coronary artery disease (ACAD). Atherosclerotic or inflammatory coronary aneurysms are usually multiple and involve more than one coronary artery. In contrast, congenital, traumatic, or dissecting aneurysms typically involve a single artery [16]. There is some evidence that angina pectoris and left ventricular dysfunction can occur with coronary artery aneurysms without coronary artery obstruction; although the specific role of the aneurysm, thrombosis and embolization has not been elucidated as the cause of myocardial infarction in patients with stenosis [2,15,17,18]. The diagnosis can be made through multiple imaging technologies including echocardiography, magnetic resonance and computed tomography, but coronary angiography remains the gold standard as it provides information regarding the size, number, position of the aneurysms, and the presence or absence of coronary artery atherosclerosis [19,20]. Our case describes an elder man with a history of dyspnea on mild exertion and high risk for ACAD. The inducible ischemia revealed on the MPI could have been caused by the stenosis, the aneurysms or a combination of both. Even though multiple aneurysms can be present with atherosclerotic heart disease, the involvement of the LM is not common. This clinical scenario imposes an additional challenge regarding the therapeutic approach (Figure 2).
There is no accepted preferred management of coronary aneurysms but surgical correction is the most commonly used therapy [8,14,19,21]. Endovascular techniques and conservative medical therapy with either antiplatelets or anticoagulants are other viable options with variable rates of success [9,21-23]. Surgical interventions include aneurysm ligation with distal bypass grafting, isolated coronary artery bypass grafting, aneurysm plication, and saphenous vein patch repair of the aneurysm. These procedures are often performed as part of a multivessel bypass operation [13,23,24]. In a fusiform aneurysm of the LM, proximal and distal ligation with bypass grafting to the LAD and circumflex is a feasible option; adequate caliber is required in both vessels. We preferred to perform a single graft to the LAD as the apparent culprit for the ischemia found on the MPI. After the procedure, medical management with antiplatelets was also indicated. Endovascular therapies (coiling and stenting) with exclusion of the aneurysm were discouraged, since these are described with satisfactory results in saccular aneurysms but not fusiform morphologies. The improvement of symptoms was sustained in the immediate and subsequent follow up.
Conclusion
In our particular case, the finding of a 14 mm fusiform aneurysm involving the left main coronary artery imposed a technical challenge regarding the therapeutic approach. Even though most of the available literature supports surgical interventions as therapy for coronary aneurysms, there is not enough pooled data about the specific anatomies encountered in the various studies. In this review, the studies under consideration described surgical and endovascular repair of saccular aneurysms but not fusiform anatomies. The frequency of involvement of the LM is also the lowest in the literature and most of the techniques described were done in other vessels. The decision to perform a distal LIMA to LAD bypass graft was based on the rationale that both circumflex and RCA were not amenable to surgery due to small caliber vessel size.
References
- Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation. 67(1): 134–138 (1983).
- Befeler B, Aranda MJ, Embi A, Mullin FL, El-Sherif N, Lazzara R. Coronary artery aneurysms: study of the etiology, clinical course and effect on left ventricular function and prognosis. Am. J. Med. 62(4): 597–607 (1977).
- Hartnell GG, Parnell BM, Pridie RB. Coronary artery ectasia: its prevalence and clinical significance in 4993 patients. Br. Heart. J. 54: 392–395 (1985).
- Demopoulos VP, Olympios CD, Fakiolas CN, et al. The natural history of aneurismal coronary artery disease. Heart. 78: 136–141 (1997).
- Packard M, Wechsler HF. Aneurysms of coronary arteries. Arch. Intern. Med. 43: 1–14 (1929).
- Syed M, Lesch M. Coronary artery aneurysm: a review. Prog. Cardiovasc. Dis. 40(1): 77–84 (1997).
- Villines TC, Avedissian LS, Elgin EE. Diffuse nonatherosclerotic coronary aneurysms. Cardiol. Rev. 13: 309–311 (2005).
- Pahlavan PS, Niroomand F. Coronary artery aneurysm: a review. Clin. Cardiol. 29(10): 439-443 (2006).
- Cohen P, O'Gara PT. Coronary artery aneurysms: a review of the natural history, pathophysiology, and management. Cardiol. Rev. 16(6): 301-304 (2008).
- Robinson FC. Aneurysms of the coronary arteries. Am. Heart. J. 109(1): 129–135 (1985).
- Kelley MP, Carver JR. Coronary artery aneurysms. J. Invasive. Cardiol. 14(8): 461-462 (2002).
- Nichols L, Lagana S, Parwani A. Coronary artery aneurysm: a review and hypothesis regarding etiology. Arch. Pathol. Lab. Med. 132(5): 823–828 (2008).
- Falsetti HL, Carrol RJ. Coronary artery aneurysm. A review of the literature with a report of 11 new cases. Chest. 69 (5): 630-636 (1976).
- Nazareth J, Weinberg L, Fernandes J, Peyton P, Seevanayagam S. Giant right coronary artery aneurysm presenting with non-ST elevation myocardial infarction and severe mitral regurgitation: a case report. J. Med. Case. Rep. 5: 442 (2011).
- Anfinsen OG, Aaberge L, Geiran O, Smith HJ, Aakhus S. Coronary artery aneurysms mimicking cardiac tumor. Eur. J. Echocardiogr. 5(4): 308-312 (2004).
- Mata KM, Fernandes CR, Floriano EM, Martins AP, Rossi MA, Ramos SG. Coronary artery aneurysms: an update. Novel strategies in ischemic heart disease. Rijeka. Croatia: InTech. pp: 381-404 (2012).
- Pavlidis AN, Malakos JS, Karavolias GK, et al. Left main coronary artery aneurysm. Herz. 37(5): 565-566 (2012).
- Newcomb EW, Youngman DJ, Burton NA, Robinowitz M, Zoltick JM. Atherosclerotic aneurysm of the left main coronary artery. J. Am. Coll. Cardiol. 4(5): 1062-1064 (1984).
- Eshtehardi P, Cook S, Moarof I, Triller HJ, Windecker S. Giant coronary artery aneurysm: imaging findings before and after treatment with a polytetrafluoroethylene-covered stent. Circ. Cardiovasc. Interv. 1(1): 85-86 (2008).
- Aqel RA, Zoghbi GJ, Iskandrian A. Spontaneous coronary artery dissection, aneurysms, and pseudoaneurysms: a review. Echocardiogra. 21(2): 175-182 (2004).
- Vranckx P, Pirot L, Benit E. Giant left main coronary artery aneurysm in association with severe atherosclerotic coronary disease. Cathet. Cardiovasc. Diagn. 42(1): 54-57 (1997).
- Keyser A, Hilker MK, Husser O, Diez C, Schmid C. Giant coronary aneurysms exceeding 5 cm in size. Interact. Cardiovasc. Thorac. Surg. 15(1): 33-36 (2012).
- Chrissoheris MP, Donohue TJ, Young RS, Ghantous A. Coronary artery aneurysms. Cardiol. Rev. 16(3): 116-123 (2008).
- Szalat A, Durst R, Cohen A, Lotan C. Use of polytetrafluoroethylene-covered stent for treatment of coronary artery aneurysm. Catheter. Cardiovasc. Interv. 66(2): 203-208 (2005).