Perspective - Interventional Cardiology (2012) Volume 4, Issue 6
Coronary bypass surgery versus percutaneous coronary intervention: the saga continues
- Corresponding Author:
- Ran Kornowski
Cardiac Catheterization Laboratories, Department of Cardiology
Rabin Medical Center, Tel Aviv University, Petah Tikva (49100), Israel
Tel: +972 3 9376441
Fax: +972 3 9231016
E-mail: ran.kornowski@gmail.com
Abstract
Keywords
coronary artery disease, multivessel coronary disease, renal failure, restenosis, revascularization, SY NTAX score
The debate over the optimal method of revascularization for patients with coronary multivessel disease (MVD) has raged on for many years, and it continues to date. In fact, the recent report of the Comparative Effectiveness of Revascularization Strategies Trial (ASCERT) has rekindled the professional debate [1]. This large sample report was one of the most comprehensive data sets published that described coronary revascularization outcomes in patients aged 65 years or older. Although no difference in mortality was evident between the methods after 1 year, the adjusted all-cause mortality after 4 years was lower with coronary artery bypass grafting (CABG) surgery than with percutaneous coronary intervention (PCI). The ASCERT data set showed a long term prognostic advantage of CABG over PCI that was independent of different subgroups. This advantage was also evident among patients that had propensity scores consistent with the selection of PCI as the preferred therapeutic strategy. However, the ASCERT trial did not provide information about the coronary anatomy of treated patients. This information is crucial to the therapeutic decision-making process.
As might be expected from a nonrandomized study, the two treatment groups differed significantly. The propensity scores were also divergent, showing a potential for selection bias. However, other observational studies showed results similar to those presented in ASCERT [2,3]. The large number of patients and the consistency of the results with previous reports lent ‘weight’ to the trial results that favored the CABG revascularization strategy. The New York Registry [2] and a meta-analysis by Hlatky [3] also demonstrated results in favor of CABG. It is notable that in those studies, the survival benefit of surgery also increased over time. In the New York Registry [2], the CABG arm had more patients with triple- vessel disease and/or multiple comorbidities than in the PCI arm. This fact reinforces the potential advantage of CABG over mutivessel PCI. The meta-analysis by Hlatky [3] showed that in patients with diabetes, mortality was substantially lower in the CABG group than following PCI. Nonetheless, in patients without diabetes, the mortality was comparable. Moreover, in patients younger than 65 years of age, no difference in long-term mortality was observed between CABG and PCI. Treatment effect was not altered by the number of diseased vessels or other baseline characteristics.
The importance of the SY NTAX score
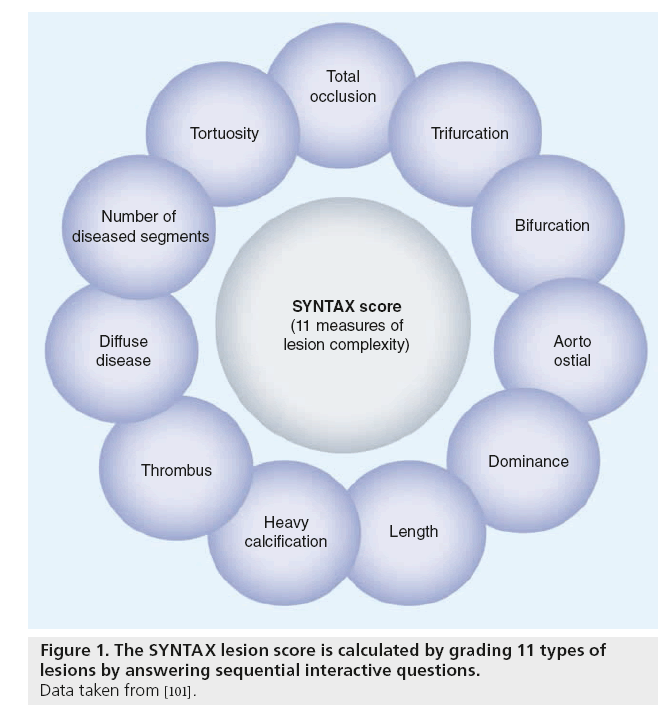
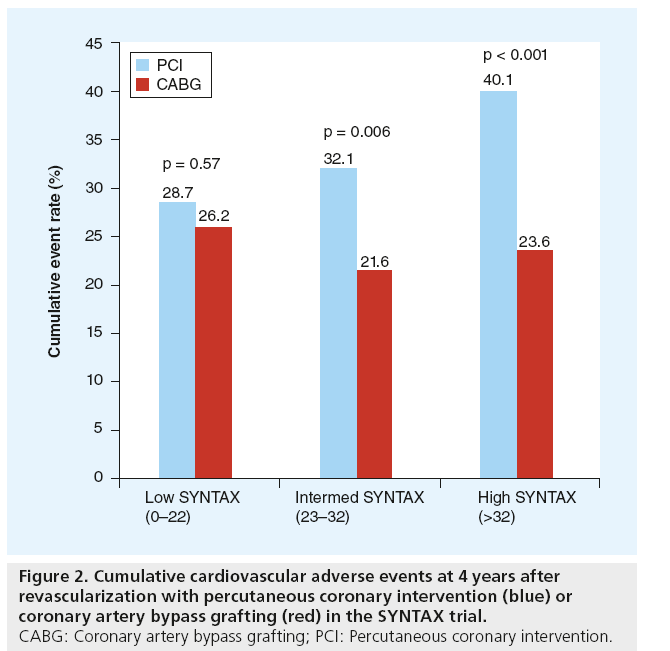
Based on those studies, the European Guidelines supported the use of CABG over PCI for severe cases of MVD and left main coronary disease [4]. Severe disease was defined primarily by a high SYNTAX score (an angiographic tool for grading the complexity of coronary artery disease [CAD]) (Figure 1) [5], and the coexistence of diabetes [4]. The SYNTAX trial was a robust, prospective randomized trial that compared the CABG and PCI approaches. The results indicated that, for more severe CAD (SYNTAX scores >22 for three-vessel or left main coronary disease), CABG offered a survival advantage, and it reduced the need for a repeat intervention and overall adverse cardiovascular events up to 4 years after revascularization (Figure 2) [6]. They also observed that CABG led to more complete revascularization [7] and/or improved long-term benefit [8]. Thus, for patients with more complex coronary milieu, such as diffuse CAD, CABG was associated with lower rates of mortality, myocardial infarction and repeated revascularization compared with PCI [9]. On the other hand, PCI offers a lower stroke rate and an easier, more rapid recovery.
Figure 2: Cumulative cardiovascular adverse events at 4 years after
revascularization with percutaneous coronary intervention (blue) or
coronary artery bypass grafting (red) in the SY NTAX trial.
CABG: Coronary artery bypass grafting; PCI: Percutaneous coronary intervention.
Upon examination of the clinical features of the participating patients in the SYNTAX trial, one may argue that the PCI arm was not equally balanced with the CABG arm. This was due in part to the fact that the European System for Cardiac Operative Risk Evaluation (EuroSCORE) indicated that the risk of peri-operative mortality was quite low (e.g., EuroSCORE less than four). Also, a significant proportion of patients had very complex coronary anatomy, including bifurcation lesions in 70% of patients and chronic total occlusions in 20%. Also, the investigators used the Taxus® drug-eluting stent, which is currently known to cause a higher rate of angiographic restenosis and stent thrombosis than either the sirolimus- or everolimus-coated stents [10]. Moreover, the mean stented length was 86 mm, and one-third of the stented lengths were at least 100 mm. However, the surgical arm could also have been improved: only 15% of those patients had off-pump procedures; only approximately 20% had complete revascularization; and only 27.6% had double arterial grafts (e.g., left internal mammary artery/right internal mammary artery); thus, the overall number of grafts per patient was actually smaller than might have been expected [6].
One important tool, already mentioned, is the SYNTAX score (Figure 1), an anatomic scoring system, based on the coronary angiogram, which quantifies lesion complexity and predicts clinical outcomes after PCI or CABG in patients with MVD and/or left main coronary artery disease [5,11]. The drawback to this score is that it does not take into consideration the clinical features of the patient. For example, the presence of diabetes, chronic renal failure or neurologic impairment could profoundly affect the treatment decision process.
SY NTAX integration
The development of the SYNTAX score has provided useful information on angiographic coronary anatomy. However, there are limitations to the SYNTAX method. The SYNTAX score has been shown to be an independent predictor for adverse cardiovascular events in patients treated with PCI, but not following CABG [6]. Also, recent studies have shown that many angiographically ‘significant’ lesions were not necessarily physiologically significant. Thus, stenting these lesions could result in over-treatment and worsened outcomes [12]. Recently, an alternative method, called the ‘functional SYNTAX score’ (FSS), was developed by Nam et al. [13]; the FSS integrates physiology into the angiographic assessment. The FSS was tested in the FAME study, where they demonstrated that treatment based on a functional flow reserve measurement in addition to angiography could reduce the rates of unnecessary revascularizations and improve clinical outcomes in patients with MVD. More importantly, patients with angiographically severe, but physiologically insignificant, lesions were reclassified. As a result, with the FSS, 32% of patients originally considered at high or intermediate risk, based on angiography, were reclassified to a lower risk level, based on function. In the latter group, the prognosis might be similar to patients that were assigned to the lower risk group based on the angiographic assessment alone [13–15]. The integration of functional flow reserve and SYNTAX showed better predictions of clinical outcome than the purely anatomic SYNTAX score [7]. Furthermore, this method enabled the diagnosis of flow-limiting lesions among coronary patients, which reduced unnecessary use of stents and potential adverse consequences [15].
The ‘Clinical SYNTAX score’ incorporates clinical elements (e.g., age, renal function and heart failure status) into the angiographic assessment [16–19]. It showed superior ability compared with the anatomic SYNTAX score for predicting major adverse cardiac events and mortality during follow-up [16,17].
Capodanno et al. performed a retrospective study to evaluate the SYNTAX score combined with the surgical EuroSCORE [18]. This analysis was aimed to predict the clinical outcomes in a registry of patients that had undergone PCI or CABG for treating unprotected left main disease. The results showed that this combination of tools provided useful information for making optimal revascularization choices. Garg et al. showed that the clinical SYNTAX score was superior to the anatomic SYNTAX score alone for predicting cardiovascular events in patients with MVD (left main not included) during a 5-year follow-up [19].
The Heart Team concept
The ‘Heart Team’ concept, which includes a consultation and decision-making forum by a multidisciplinary team (e.g., interventional cardiologist and a cardiac surgeon and other specialists as needed), is currently a Class 1C indication for managing patients with unprotected left main or complex coronary disease, according to the European Revascularization guidelines [4]. The concept of the Heart Team has also been adopted for treatments in other areas of cardiology, including valvular or structural heart diseases. A revascularization strategy should be derived from a consensus between the interventional cardiologist and the cardiac surgeon, based on the clinical and angiographic features of the patients, and according to evidence-based data.
The Heart Team concept is important, but it is by no means new or revolutionary to many centers around the world. In multiple hospitals, cardiologists routinely obtain opinions and consensus from interventionalists, surgeons and the patients themselves when deciding and recommending a course of treatment.
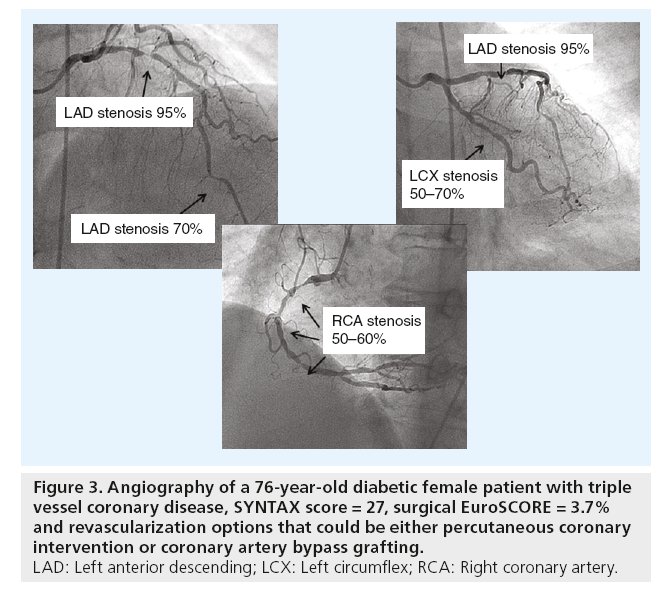
However, the Heart Team structure is the best place to discuss patients that fall in the ‘gray zone’ of complex CAD, or patients with numerous comorbidities. With invasive techniques, like PCI and CABG, patients should understand the potential benefits, risks and limitations of each treatment modality before they are asked to provide informed consent. Once fully aware of the potential benefits and risks of each revascularization strategy, the patient’s desires and expectations should be a key part of the Heart Team’s decision. The SYNTAX trial is a tool that helps to widen the gap between the outcomes of CABG and PCI; on the other hand, patient wishes and physicians agreeing to bend to this is no reason to offer an inferior treatment. This strategy implies that, in stable patients and suitable conditions, the operator should stop the coronary angiography to discuss decisions with the Heart Team and the patient. This approach provides transparency for the decision-making process. Figure 3 highlights a case example of a coronary patient with MVD who could potentially benefit from the Heart Team discussion about the mode of revascularization, with treatment decisions that could be either multivessel PCI or CABG.
Figure 3: Angiography of a 76-year-old diabetic female patient with triple
vessel coronary disease, SYNTAX score = 27, surgical EuroSCORE = 3.7%
and revascularization options that could be either percutaneous coronary
intervention or coronary artery bypass grafting.
LAD: Left anterior descending; LCX: Left circumflex; RCA: Right coronary artery.
Older patients
Treatments for older patients merit special attention. The older population is growing; these individuals run increased risk during revascularization procedures, augmented risks of complications, such as periprocedural mortality, major bleeding and stroke, often experience delayed recovery [4]. For example, a patient with a history of cerebrovascular events might recover more readily after a PCI than a CABG, despite having a high SYNTAX score. In those circumstances, immediate recovery may take precedence over other long-term prognostic measures. Moreover, considering the high incidence of stroke or cognitive impairments following the CABG, the Heart Team may deviate from basing their decision solely on the SYNTAX score. Puskas et al. shows that a different technique in surgery, like off-pump coronary artery bypass, can be of benefit in elderly and high-risk patients that do benefit from surgery, and could produce good results with these relatively novel surgical techniques [20].
PCI is not a trivial matter in older individuals either. It is one of the strongest predictors of procedural complications, morbidity and mortality [21]. Nonetheless, based on recent studies, the angiographic success rates and clinical benefits of PCI are quite similar in older and younger patients [22].
Gender
Another consideration relates to gender. Although the majority of patients with coronary disorders are men (78% in the SYNTAX trial), CAD remains the leading cause of death in women in most parts of the Western world [23]. Historically, women sustained worse outcomes during and following PCI compared with men. Also, women showed a more complex clinical preoperative presentation and were more likely to be readmitted with unstable angina and congestive heart failure after CABG [24]. Thus, it is yet unknown whether the revascularizaton guidelines are fully applicable to women. Using contemporary PCI techniques, the clinical outcomes of women undergoing PCI are equivalent to men, particularly when drug-eluting stents are utilized to treat coronary lesions [25]. Thus, there is no evidence to support the notion that gender per se should play a major role in the choice of revascularization technique. This issue should be explored further in additional trials with adequate representation of female patients.
Diabetes mellitus
The SOS trial was a randomized, controlled trial that compared outcomes after PCI or CABG for patients with MVD [26]. A total of 988 (n = 488 PCI, n = 500 CABG) patients were randomized. At a median follow-up of 6 years, a continuing survival advantage was observed for patients managed with CABG. That study has provided one of the strongest arguments in favor of the CABG versus PCI strategy for patients with diabetes and MVD. The European guidelines indicate that, for patients that require revascularization for MVD, diabetes mellitus is an important factor for selecting a revascularization strategy [4]. In particular, when complex or extensive CAD is present, the evidence supports CABG over PCI. In the most recent publication of the FREEDOM trial [27], a total of 1900 diabetic patients were randomized, 953 to PCI and 947 to CABG. The primary composite outcome of death, MI and stroke at 5 years was significantly higher in the PCI arm compared with the CABG arm (26.6 vs 18.7%; p = 0.005), driven by significant reductions in all-cause mortality (16.3 vs 10.9%; p = 0.049) and myocardial infarction (13.9 vs 6.0%; p < 0.001); strokes were lower in the PCI arm (2.4 vs 5.2%; p = 0.03). The investigators concluded that “in diabetic patients with multivessel disease, CABG is superior to DES PCI, and should remain the revascularization strategy of choice in this patient population.”
Previous CABG
Studies that focused on patients with a previous CABG that required further treatment with either a PCI or a repeat CABG reported similar survival rates for the two procedures [28]. A recent report shows that clinical outcomes are similarly unfavorable after triage for CABG or PCI in patients with a graft failure [29]. Repeat revascularization occurred more frequently after PCI, particularly following bare-metal stent implantation. These patients had undergone a previous CABG and experienced refractory myocardial ischemia. The choice of revascularization would depend on the vascular and graft anatomy and pathology; the number of diseased vessels and/or bypass grafts; the availability, course and function of the internal mammary artery; and the availability of distal targets for either an additional bypass graft placement or for a PCI. Factors that favored a PCI over CABG included high surgical risk, suitable PCI targets in the grafts or the native coronary artery, a patent graft to the left anterior descending artery, poor CABG targets and comorbid conditions.
Renal failure
Many patients with CAD experience chronic renal failure (CRF) [30]. These patients are at increased risk of morbidity and mortality following coronary revascularization [31]. Randomized comparisons of coronary revascularization strategies in patients with CRF have not been reported. Hemmelgarn et al. compared CRF patients that received a CABG, PCI or no revascularization after coronary angiography [32]. They found that in patients with CRF who received dialysis, survival was significantly higher after CABG or PCI versus no revascularization at all. Those data were not particularly helpful in selecting between the CABG and PCI strategy for patients with end-stage renal disease. The ARTS subanalysis randomly assigned 1205 participants, with and without chronic kidney disease (CKD), to CABG or PCI with multivessel stenting. In patients with multivessel CAD and CKD, treatment with CABG or PCI with multivessel stenting led to similar outcomes of death, MI or stroke. Repeat revascularization was greater with PCI. Overall, those with CKD had a substantially elevated risk of adverse clinical outcomes after coronary revascularization [32].
Of note, both revascularization techniques can aggravate renal insufficiency through different mechanisms of renal injury (i.e., contrastinduced nephropathy vs bypass machine and/or hemodynamic instability). In either case, deterioration of renal function is associated with worse outcomes. Thus, renal injury should be avoided as much as possible, and the potential for injury should be considered in the treatment algorithms.
LV systolic dysfunction
The data that exist at present on revascularization in patients with coronary artery disease and LV systolic dysfunction are more robust for CABG than for PCI [2,3]. Since there is a paucity of randomized trials in patients with LV dysfunction, the choice of revascularization in these patients is based on clinical variables, coronary anatomy, myocardial viability status, presence of diabetes mellitus, presence of CKD, magnitude of LV systolic dysfunction, patient preferences, clinical judgment, and consultation between the clinical cardiologist, heart failure specialist, interventional cardiologist and the cardiac surgeon (e.g., the multidisciplinary Heart Team) [4].
ST elevation myocardial infarction
Urgent PCI aimed at the culprit lesion only is the preferred treatment of choice during the course of ST elevation acute myocardial infarction (STEMI) [33]. In the case of MVD and STEMI, additional revascularization of the nonculprit lesion during the course of STEMI is not advisable and is probably associated with a worse prognosis [34]. A deferred PCI strategy, if needed, is thus the treatment of choice [33]. There are a small number of patients who require CABG surgery in the acute phase of STEMI. Those are patients with anatomy unsuitable for PCI where CABG may be indicated. Cardiogenic shock is another indication if the coronary anatomy is not amenable to PCI, or at the time there is an urgent need to repair a mechanical cardiac complication [33]. CABG is rarely used in the setting of STEMI and its benefits are uncertain in patients with failed PCI, coronary occlusion not amenable to PCI, and in the presence of refractory symptoms after PCI [33]. In most of these cases, the time for implementation of surgical reperfusion will be long and the risks associated with surgery are maximal in this setting. Certainly more data are needed on the value of urgent CABG during the course of complicated STEMI and/or failed PCI.
Conclusion & future perspective
In addition to intensified medical pharmacotherapy, treatments for atherosclerotic coronary disease include two very different revascularization techniques. Surgery involves placing bypass grafts beyond obstructive lesions of any complexity. It offers a long-term solution that addresses subsequent progression of the disease proximal to the distal anastomotic site. In contrast, PCI is performed with contemporary techniques, using drug-eluting stents that are placed to treat culprit lesions. However, the PCI technique does not offer a solution for disease progression, and it carries the risk of restenosis and thrombosis. Therefore, these revascularization techniques must be accompanied by intense medical treatment to provide a greater success in the long- term, and prevent disease progression.
Recovery from PCI is much faster than from CABG, and PCI does not involve open-chest thoracotomy. PCI has been the preferred choice for many physicians and patients, despite its limitations and long-term disadvantages. The PCI approach requires long-term, dual antiplatelet treatment to achieve satisfactory results. Moreover, as the diffusion and complexity of a coronary disease increases, the long-term benefit of CABG over PCI becomes more apparent and meaningful. Recommendations of either PCI or CABG for a coronary intervention should be individualized and evidence-based. The overall clinical scenario should take into consideration important variables, including the clinical presentation, anatomic SYNTAX score, patient’s age, comorbidities, renal function, mental and neurologic status, and the tolerance for long-term treatment with dual antiplatelet medications. Patient expectations and preferences should also be considered. Thus, the mode of revascularization should be carefully thought out. CABG and PCI can be viewed as complementary, rather than competitive, techniques. In addition, the use of the ‘functional SYNTAX score’ can provide a more physiologic assessment of lesion severity and true need for revascularization. The Heart Team approach can ensure that patients with coronary pathologies get the best available treatment, without unnecessary professional debates.
Executive summary
Background
▪ The debate over the optimal mode of revascularization for patients with multivessel coronary disease still continues, but recent trials and registries showed a long-term prognostic advantage for coronary artery bypass grafting (CABG) over percutaneous coronary intervention (PCI) that was independent of subgroups analysis.
The importance of the SYNTAX score
▪ The SYNTAX score is an important anatomic scoring system, based on the coronary angiogram, which quantifies lesion complexity and predicts clinical outcomes after PCI or CABG in patients with multivessel coronary disease and/or left main disease.
▪ The drawback to this score is that it does not take into account the clinical features of the patient.
SYNTAX integration
▪ ‘Functional SYNTAX score’, integrates the coronary physiology into the angiographic assessment.
▪ The ‘Clinical SYNTAX score’ incorporates clinical elements (e.g., age, renal function and heart failure status) into the angiographic assessment.
The Heart Team concept
▪ The Heart Team concept includes a consultation and decision-making forum by a multidisciplinary team.
▪ The Heart Team structure is the best forum to discuss patients that fall within the ‘gray zone’ of complex coronary disease or patients with numerous comorbidities.
Older patients
▪ The older population is growing, with increased risk during and/or following revascularization procedures.
▪ The angiographic success rates and clinical benefits of contemporary PCI are quite similar in older and younger patients.
Gender
▪ Coronary artery disease is the leading cause of death in women. Contemporary revascularization strategies and techniques should be similar for women and men.
Diabetes mellitus
▪ For patients with multivessel disease, diabetes mellitus is a strong predictor of more diffuse disease and/or adverse outcomes.
▪ In many cases, diabetes mellitus should support the use of CABG over PCI.
Previous CABG
▪ Both PCI and repeat CABG are therapeutic options. The prognosis is quite poor regardless of the mode of repeat revascularization.
Renal failure
▪ Patients with renal failure are at increased risk of morbidity and mortality following coronary revascularization.
▪ Randomized comparisons of coronary revascularization strategies in patients with renal failure have not been reported.
▪ Both revascularization techniques can aggravate renal insufficiency through different mechanisms of renal injury.
Left ventricle systolic dysfunction
▪ Current data on revascularization in patients with coronary artery disease and left ventricular systolic dysfunction are limited, but current data are more robust for CABG than for PCI.
ST elevation myocardial infarction
▪ Urgent PCI aimed at the culprit lesion only is the preferred treatment of choice during the course of ST elevation acute myocardial infarction.
▪ The role of emergent CABG during the course of ST elevation acute myocardial infarction remains for failed PCI and/or mechanical complications.
Summary & conclusion
▪ Current recommendations concerning PCI or CABG for multivessel coronary disease should be individualized and evidence-based.
▪ Important variables should be taken into consideration following the treatment decision: clinical presentation; anatomic; functional and clinical SYNTAX scores; patient’s age; associated diseases; renal function; mental and neurologic status; and the tolerance for long-term pharmacotherapy.
▪ The Heart Team approach can ensure that patients with coronary pathologies can obtain the best medical treatment.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Weintraub W, Grau-Sepulveda M, Weiss Jet al. Comparative effectiveness ofrevascularization strategies. N. Engl. J. Med.366, 1467–1476 (2012).
- Hannan EL, Wu C, Walford G et al.Drug-eluting stents vs. coronary-artery bypassgrafting in multivessel coronary disease.N. Engl. J. Med. 358, 331–341 (2008).
- Hlatky MA, Boothroyd DB, Bravata DM et al.Coronary artery bypass surgery compared withpercutaneous coronary interventions formultivessel disease: a collaborative analysis ofindividual patient data from ten randomizedtrials. Lancet 373, 1190–1197 (2009).
- Wijns W, Kolh P, Danchin N et al. Guidelineson myocardial revascularization. The taskforce on myocardial revascularization of theEuropean Society of Cardiology (ESC) andthe European Association for Cardio-ThoracicSurgery (EACTS). Eur. Heart J. 31,2501–2555 (2010).
- Sianos G, Morel MA, Kappetein AP et al.The SYNTAX score: an angiographic toolgrading the complexity of coronary arterydisease. EuroIntervention 1, 219–227 (2005).
- Serruys PW, Morice MC, Kappetein AP et al.SYNTAX investigators. Percutaneouscoronary intervention versus coronary-arterybypasses grafting for severe coronary arterydisease. N. Engl. J. Med. 360, 961–972 (2009).
- Head S, Mack MJ, Kappetein AP. Incidence,predictors and outcomes of incompleterevascularization after percutaneous coronaryintervention and coronary artery bypassgrafting. A Subgroup analysis: 3 yearfollow-up of the SYNTAX data.Eur. J. Cardiothorac. Surg. 41, 531–541(2012).
- Kappetein AP, Feldman TE, Colombo A et al.Comparison of coronary bypass surgery withdrug-eluting stenting for the treatment of leftmain and/or three-vessel disease: 30-yearfollow-up of the SYNTAX trial. Eur. HeartJ. 32, 2125–2134 (2011).
- Cohen DJ, Van Hout B, Kappetein AP.Synergy between PCI with taxus and cardiacsurgery investigators. Quality of life after PCIwith drug-eluting stents or coronary-arterybypass surgery. N. Engl. J. Med. 364,1016–1026 (2011).
- Kastrati A, Dibra A, Eberle S et al. Sirolimuselutingstents vs. paclitaxel-eluting stents inpatients with coronary artery disease:meta-analysis of randomized trials. JAMA294, 819–825 (2005).
- Serruys PW, Onuma Y, Garg S et al.Assessment of the SYNTAX scores in thesyntax study. EuroIntervention 5, 50–56 (2009).
- Pijls NH, van Schaardenburgh P, ManoharanG et al. Percutaneous coronary intervention offunctionally nonsignificant stenosis: 5yearfollow-up of the DEFER study. J. Am. Coll.Cardiol. 49, 2105–2111 (2007).
- Nam CW, Mangiacapra F, Entjes R et al.Functional SYNTAX score for risk assessmentin multivessel coronary artery disease. J. Am.Coll. Cardiol. 58, 1211–1218 (2011).
- Tonino PA, De Bruyne B, Pijls NH et al.Fractional flow reserve versus angiography forguiding percutaneous coronary intervention.N. Engl. J. Med. 360, 213–224 (2009).
- Nam CW, Mangiacapra F, Entjes R et al.Functional SYNTAX score for risk assessmentin multivessel coronary artery disease. J. Am.Coll. Cardiol. 58, 1211–1218 (2011).
- Wykrzykowska JJ, Garg S, Girasis C et al.Value of the syntax score for risk assessment in the all-comers population of the randomizedmulticenter LEADERS (Limus eluted from adurable versus erodable stent coating) trial.J. Am. Coll. Cardiol. 56, 272–277 (2010).
- Jou YL, Lu TM, Chen YH et al. Comparisonof the predictive value of EuroSCORE,SYNTAX score, and clinical SYNTAX scorefor outcomes of patients undergoingpercutaneous coronary intervention forunprotected left main coronary arterydisease. Cath. Cardiovasc. Interv. 80,222–230 (2012).
- Capodanno D, Di Salvo ME, Cincotta G,Miano M, Tamburino C, Tamburino C.Usefulness of the SYNTAX score forpredicting clinical outcome afterpercutaneous coronary intervention ofunprotected left main coronary artery disease.Circ. Cardiovasc. Interv. 2, 302–308 (2009).
- Garg S, Sarno G, Garcia-Garcia HM et al.A new tool for the risk stratification ofpatients with complex coronary artery disease:the clinical SYNTAX score. Circ. Cardiovasc.Interv. 3, 317–326 (2010).
- Puskas JD, Thourani VH, Kilgo P et al.Off-pump coronary artery bypassdisproportionately benefits high-risk patients.Ann. Thorac. Surg. 88, 11427 (2009).
- Singh M, Peterson ED, Roe MT et al. Trendsin the association between age and in-hospitalmortality after percutaneous coronaryintervention: National Cardiovascular DataRegistry experience. Circ. Cardiovasc. Interv.2, 20–26 (2009).
- Moonen LA, van’t Veer M, Pijls NH.Procedural and long-term outcome of primarypercutaneous coronary intervention inoctogenarians. Neth. Heart J. 18, 129 –1234(2010).
- Chieffo A, Hoye A, Mauri F et al. WIN Group;Women in Innovations Initiative. Gender-basedissues in interventional cardiology: a consensusstatement from the Women in Innovations(WIN) Initiative. Catheter Cardiovasc. Interv.75, 145–152 (2010).
- Guru V, Austin PC, Tu JV et al. Genderdifferences in outcomes after hospitaldischarge from coronary artery bypassgrafting. Circulation 113(4), 507–516 (2006).
- Kornowski R, Vaknin-Assa H, Assali A et al.A comparative analysis of major clinicaloutcomes with drug-eluting stents versus baremetal stents in male versus female patients.EuroIntervention 7, 1051–1059 (2012).
- Booth J, Clayton T, Pepper J et al.Randomized, controlled trial of coronaryartery bypass surgery versus percutaneouscoronary intervention in patients withmultivessel coronary artery disease: six-yearfollow-up from the Stent or Surgery Trial(SoS). Circulation 118, 381–388 (2008).
- Farkouh ME, Domanski M, Sleeper LAet al.; for the FREEDOM Trial Investigators. Strategies for multivessel revascularization inpatients with diabetes. N. Engl. J. Med.doi:10.1056/NEJMoa1211585 (2012) (Epubahead of print).
- Weintraub WS, Jones EL, Morris DC, KingSB 3rd, Guyton RA, Craver JM. Outcome ofreoperative coronary bypass surgery versuscoronary angioplasty after previous bypasssurgery. Circulation 95, 868 –8677 (1997).
- Harskamp RE, Beijk MA, de Winter RJ et al.Clinical outcome after surgical orpercutaneous revascularization in coronarybypass graft failure. J. Cardiovasc. Med. doi:10.2459/JCM.0b013e328356a4fc (2012)(Epub ahead of print).
- Hage FG, Venkataraman R, Zoghbi GJ, PerryGJ, DeMattos AM, Iskandrian AE . Thescope of coronary heart disease in patientswith chronic kidney disease. J. Am. Coll.Cardiol. 53, 2129–2140 (2009).
- Ashrith G, Elayda MA, Wilson JM.Revascularization options in patients withchronic kidney disease. Tex. Heart Inst. J. 37,9–18 (2010).
- Hemmelgarn BR, Southern D, Culleton BF,Mitchell LB, Knudtson ML, Ghali WA.Survival after coronary revascularizationamong patients with kidney disease.Circulation 110, 1890–1895 (2004).
- Van de Werf F, Bax J, Betriu A et al.Management of acute myocardial infarctionin patients presenting with persistentST-segment elevation: the task force on themanagement of ST-segment elevation acutemyocardial infarction of the EuropeanSociety of Cardiology. Eur. Heart J. 29,2909–2945 (2008).
- Kornowski R, Mehran R, Dangas G et al.Prognostic impact of staged versus “one-time”multivessel percutaneous interventions inacute myocardial infarction: analysis from theHORIZONS-AMI trial. J. Am. Coll. Cardiol.58, 704 –7011 (2011).
▪Website
101 SYNTAX Score.
www.syntaxscore.com