Case Report - Interventional Cardiology (2022) Volume 14, Issue 0
Coronary stent fracture and in-stent restenosis due to severe calcification treated with shockwave coronary intravascular lithotripsy with drug eluting balloon
- Corresponding Author:
- Amarpal Singh Gulati
Department of Cardiology,
Synergy Institute of Medical Sciences,
Ballupur,
Dehradun,
India,
E-mail: amarpal6@hotmail.com
Received date: 24-Jan-2022, Manuscript No. FMIC-22-52355; Editor assigned: 26-Jan-2022, PreQC No. FMIC-22-52355 (PQ); Reviewed date: 08-Feb-2022, QC No. FMIC-22-52355; Revised date: 15-Feb-2022, Manuscript No. FMIC-22-52355 (R); Published date: 22-Feb-2022, DOI: 10.37532/1755-5310.2022.14(s8).189
Abstract
Background: We report the case of a stent under-expansion and In-Stent Restenosis (ISR) due to a severely calcified lesion at the mid Right Coronary Artery (RCA) treated with the Shockwave Intravascular Lithotripsy (S-IVL) and Drug-Eluting Balloon (DEB).
Methods and findings: A 61-year-old man underwent coronary angiography, and intravascular ultrasound revealed mid-RCA stent under expansion and ISR due to calcified plaque. S-IVL with DEB disrupted the calcium sheet around the stent, thereby allowing optimal stent expansion.
Conclusion: This case demonstrates that S-IVL can successfully treat stent underexpansion and ISR due to heavily calcified lesions in previous stents.
Keywords
Coronary calcification • Coronary stent fracture • Drug eluting balloon • Intravascular ultrasound • In-stent restenosis • Shockwave intravascular lithotripsy
Introduction
Coronary calcification represents a challenge to the interventional cardiologist as it may cause stent under-expansion in a few cases [1]. Stent underexpansion is associated with intervention failure and adverse outcomes, including restenosis and stent thrombosis [1]. The treatment of stent under-expansion due to heavily calcified lesions is more difficult with conventional percutaneous transluminal coronary angioplasty. Another treatment plan relies on high-pressure noncompliant balloons [2], which may lead to vascular wall injury and non-performing in a few cases [3]. The Shockwave Intravascular Lithotripsy (S-IVL) has recently been approved to treat calcified coronary lesions [4]. However, its safety and efficacy for treating under-expanded, fractured stent and in-stent restenosis due to severely calcified sheets are yet to be established.
Here, we report a case of stent fracture under expansion and in-stent mid-Right Coronary Artery (RCA) restenosis successfully treated with the S-IVL and Drug- Eluting Balloon (DEB) under Intravascular Ultrasonography (IVUS) guidance.
Case Presentation
A 61 year old male presented with chief complaints of recurrent chest pain, and the last episode was reported on the night before (08 Sep 2021). His medical history included systemic hypertension, and he underwent Coronary Artery Bypass Graft (CABG) (LIMA to D1, SVG to OM1) in 2018. Echocardiography revealed regional wall motion abnormality in RCA with mild left ventricle systolic dysfunction (EF 49%), grade I left ventricle diastolic dysfunction, concentric left ventricular hypertrophy, dilated left atrium, and tachycardia during the study. The routine blood investigations showed positive troponin. The patient was advised for coronary angiography.
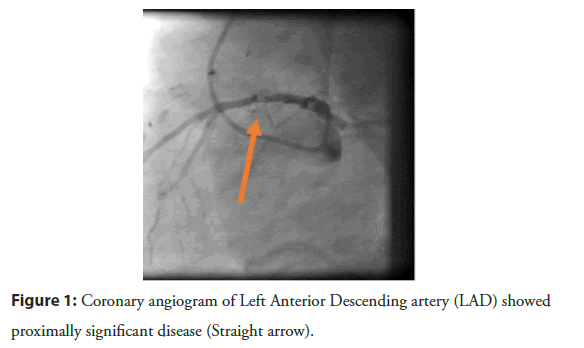
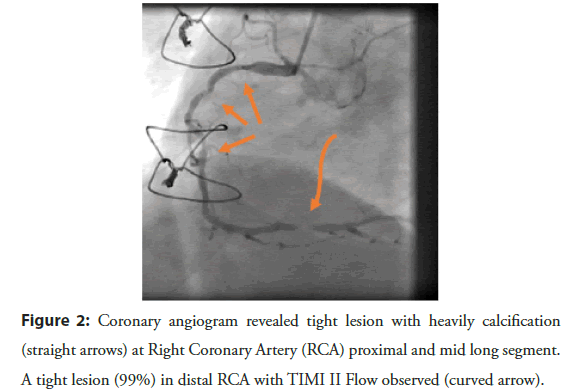
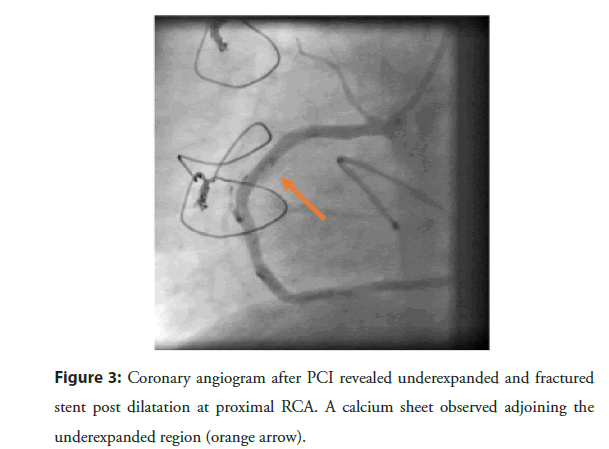
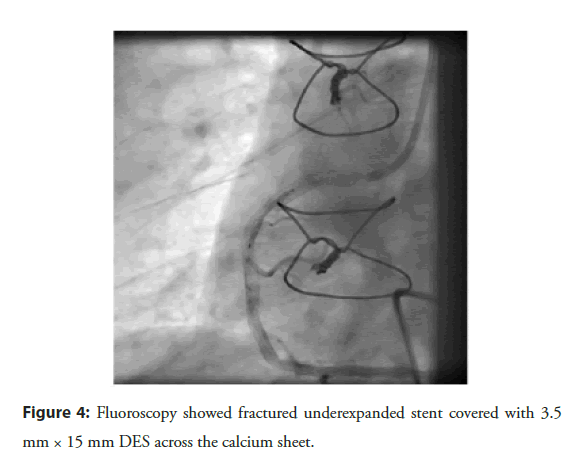
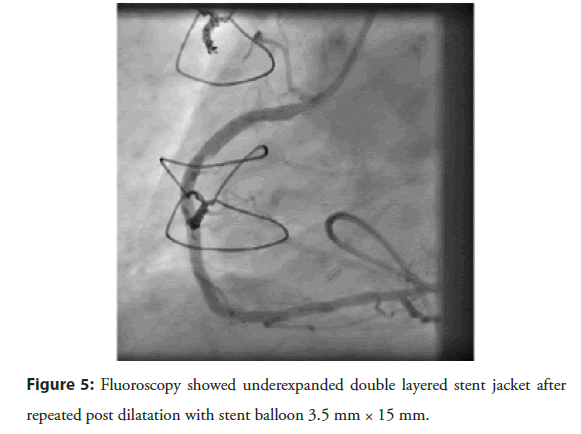
On 13 Sep 2021, coronary angiography revealed native triple vessel disease with patent grafts to D1 and large OM1. Significant stenosis (40% at ostial and 80% proximally) was recorded in the Left Anterior Descending artery (LAD) and RCA with 80% calcified lesion at the proximal and mid-portion, and 99% distal near apex, respectively (Figures 1 and 2). His electrocardiography showed q wave with T wave inversion in inferior leads. The patient was preoperatively managed with standard pharmacotherapy, including two antiplatelet agents (clopidogrel and ecospirin) and high-dose statins. As stenosis was severe in RCA, Percutaneous Transluminal Coronary Angioplasty (PTCA) to RCA and LAD was planned. On 14 Sep 2021, PTCA was performed after implantation of a temporary pacemaker via the left femoral vein. The RCA stenosis was treated via the left femoral artery approach using a 6 F Vistabrite tip JR 3.5 guiding catheter (Cordis, Inc) to engage the ostium of the RCA. A 0.014˝ SION Blue (Asahi Intech) was parked in the Posterior Lateral Ventricular (PLV) branch. A second 0.0014” Whisper ES coronary guidewire (Abbott) was used to cross the lesion into the Posterior Descending Artery (PDA). After which 1.5 × 10 mm at 17 atm (predilataion), 2.0 × 10 mm at 17 atm (predilataion) was done at distal, mid and proximal RCA lesion site. Subsequently, 2.75 × 09 mm at 16 atm (predilataion) was done at the mid, and proximal RCA lesion site. One drug-eluting stent was implanted in distal RCA over Whisper ES wire (Yukon choice PC Elite 2.5 × 16 mm at 18 atm) followed by post dilatation done with 2,75 × 9 mm at 12 atm using NC Sprinter balloon (Medtronic). Three Drug-Eluting-Stents (DES) were implanted at mid and proximal RCA (Resolute Onyx 3.0 × 22 mm at 14 atm, 3.0 × 18 mm at 16 atm and 3.5 × 22 mm at 14 atm to mid, proximal to mid and proximal RCA, respectively). Predilatation to proximal and mid-RCA lesion was done with 3.0 × 22 mm stent balloon at 12 atm prior to deployment of proximal RCA stent. NC Sprinter (Medtronic) 3.5 × 09 mm at 17 atm and 4.0 × 09 mm at 12 atm (postdilatation) was done in proximal RCA stent. However, the proximal stent appeared fractured, deformed and underexpanded (Figure 3). The fractured stent was covered with another Resolute Onyx 3.5 × 15 mm at 16 atm DES (Figure 4). The patient had hypotension and bradycardia during the Percutaneous Coronary Intervention (PCI) and was managed with intravenous atropine 0.6 mg stat and 200 mL normal saline infusion. Thrombolysis in Myocardial Infarction (TIMI) III grade flow was achieved; however, severe deep calcified sheet suboptimal expansion of mid-RCA stent was observed (Figure 5). He was clinically stable without postoperative complication and managed with two antiplatelet agents along with low dose rivaroxaban (2.5 mg twice a day) to prevent stent thrombosis. On discharge, the patient was advised for staged PTCA to LAD and RCA under IVUS guidance with IVL and DEB.
Figure 1:Coronary angiogram of Left Anterior Descending artery (LAD) showed proximally significant disease (Straight arrow).
Figure 2: Coronary angiogram revealed tight lesion with heavily calcification (straight arrows) at Right Coronary Artery (RCA) proximal and mid long segment. A tight lesion (99%) in distal RCA with TIMI II Flow observed (curved arrow).
Figure 3: Coronary angiogram after PCI revealed underexpanded and fractured stent post dilatation at proximal RCA. A calcium sheet observed adjoining the underexpanded region (orange arrow).
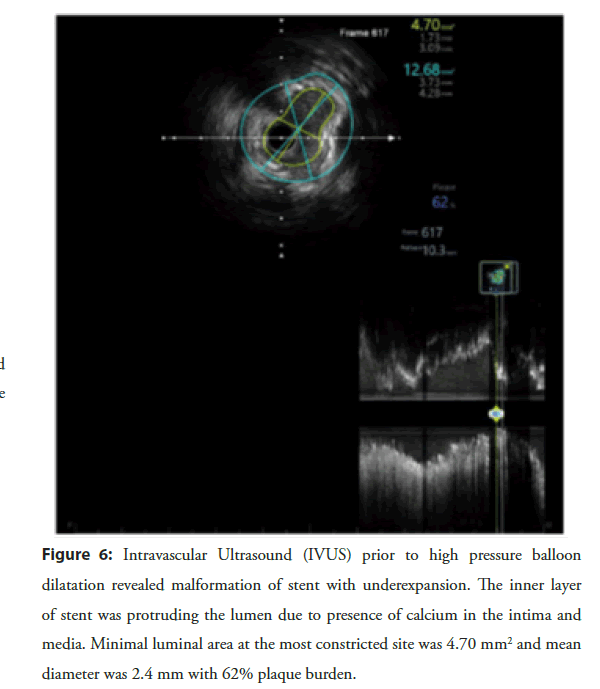
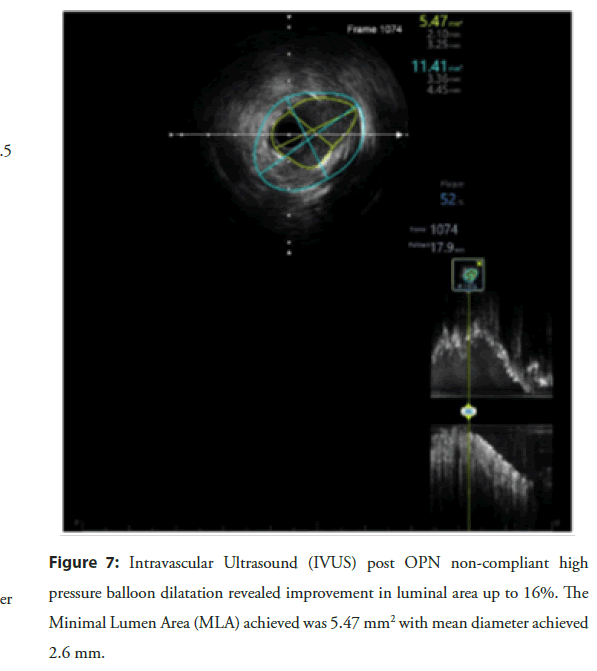
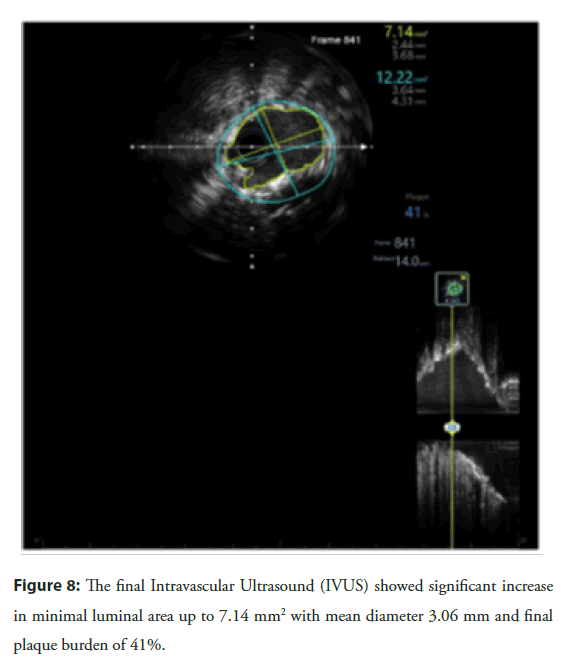
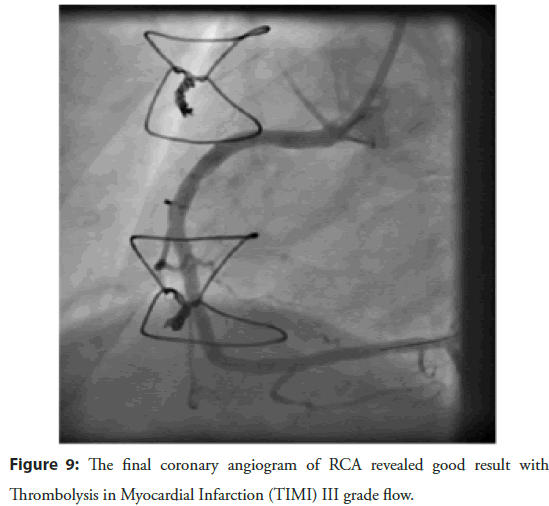
On 20 Oct 2021, the patient was reported to the hospital for planned PCI. Intravascular ultrasound at the double stent site confirmed underexpansion of the recently implanted stent (minimal stent area: 4.70 mm2 with 62% plaque burden (2.41 mm)) (Figure 6). A 3.5 × 10 mm OPN NC high-pressure balloon (SIS Medical AG) was inflated to 35 atm at the site of underexpansion but remained ineffective to improve plaque burden. Repeat IVUS revealed a minimal stent area: 5.47 mm2 with 52% plaque burden (2.67 mm) (Figure 7). A 3.5 × 12 mm lithotripsy balloon (SHOCKWAVE C2 IVL) was inflated at 4 atm and sequentially delivered four cycles of shockwave therapy (40 beats) at multiple points in mid-RCA. The lesion was nicely dilated with a 3.5 × 20 mm DEB (SeQuent® Please Neo, B BRAUN) after inflation at 10 atm for 50 seconds. The final IVUS run revealed significant improvement in Minimal Lumen Area (MLA) 7.14 mm2 with 41% plaque burden (3.06 mm) (Figure 8). The final RCA angiogram showed promising results with Thrombolysis in Myocardial Infarction (TIMI) III grade flow (Figure 9). A 3.0 × 22 mm at 13 atm drug-eluting stent was easily implanted at LAD. Acute kidney injury was reported post-operatively and managed with standard pharmacotherapy and fluid management. The patient was discharged on the third post-operative day.
Figure 6: Intravascular Ultrasound (IVUS) prior to high pressure balloon dilatation revealed malformation of stent with underexpansion. The inner layer of stent was protruding the lumen due to presence of calcium in the intima and media. Minimal luminal area at the most constricted site was 4.70 mm2 and mean diameter was 2.4 mm with 62% plaque burden.
Figure 7: Intravascular Ultrasound (IVUS) prior to high pressure balloon dilatation revealed malformation of stent with underexpansion. The inner layer of stent was protruding the lumen due to presence of calcium in the intima and media. Minimal luminal area at the most constricted site was 4.70 mm2 and mean diameter was 2.4 mm with 62% plaque burden.
Figure 9: The final coronary angiogram of RCA revealed good result with Thrombolysis in Myocardial Infarction (TIMI) III grade flow.
Results and Discussion
We present a real-world experience of S-IVL with DEB to treat a patient with mid-RCA stent fracture, underexpansion, and instent restenosis due to severe coronary calcification.
Vascular calcification is a phenotype of aging, atherosclerotic cardiovascular disease, diabetes mellitus, and chronic kidney disease [5]. Approximately 20% of PCI are challenged due to the presence of severely calcified lesions and may predict the failure of PCI, poor clinical outcome, or future major adverse cardiac events [6]. The presence and location of calcification in coronary vessels increases the time and procedural complexity [7].
The current standard treatment for the management of calcified lesions includes high-pressure non-compliant balloons, cutting/ scoring balloons, rotational/orbital atherectomy, and excimer laser but criticized due to their inherent limitations such as dissections, perforations, distal and deep embolization [8]. The appropriate selection among these techniques for the treatment and sequential alternatives if one technique fails are essential elements during planning for PCI. The present case was suitable for high-pressure balloon therapy due to stent under-expansion and in-stent restenosis at mid-RCA. The failure of a high-pressure non-compliant balloon suggested using novel S-IVL with DEB.
S-IVL is a novel therapy for treating severely calcified plaques in coronary and peripheral arteries. The therapy uses balloon inflation (max 4-6 atm) and emits localized pulsatile sonic pressure waves to disrupt calcified sheets in vessels similar to lithotripsy employed for kidney and ureteral stone [8]. The new technique was initially approved and employed for calcified lesions of peripheral vessels. On Feb 12, 2021, US-FDA approved S-IVL to treat coronary calcified lesions prior to stenting [4]. Few reports showed S-IVL safety and efficacy in-stent underexpansion and ISR due to severely calcified lesions [9-12]. However, after recent approval, real-world evidence on the performance and safety of IVL for treatment of stent underexpansion and ISR due to the severely calcified coronary lesion is an unmet need.
Conclusion
Inline, we presented a case that demonstrates the feasibility and safety of using S-IVL device with DEB to treat stent underexpansion and ISR at mid-RCA due to severe calcification. Our findings demonstrate the value of S-IVL with DEB as a novel, safe and effective procedure to treat undilatable, severely calcified coronary lesions. This novel technique can be promising to optimize the outcome of underexpanded stents presenting with in-stent restenosis in heavily calcified coronary artery disease.
References
- Mintz GS. Intravascular imaging of coronary calcification and its clinical implications. JACC Cardiovasc Imaging. 8(4): 461-71 (2015).
[CrossRef] [Google scholar] [Pubmed]
- De Silva K, Roy J, Webb I, et al. A Calcific, Undilatable stenosis: Lithoplasty, a new tool in the box? JACC Cardiovasc Interv. 10(3): 304-6 (2017).
[CrossRef] [Google scholar] [Pubmed]
- Ahn JM, Kang SJ, Yoon SH, et al. Meta-analysis of outcomes after intravascular ultrasound-guided versus angiography-guided drug-eluting stent implantation in 26,503 patients enrolled in three randomized trials and 14 observational studies. Am J Cardiol. 113(8): 1338-47 (2014).
[CrossRef] [Google scholar] [Pubmed]
- Intravascular imaging of coronary calcification and its clinical implications
- Kassimis G, Didagelos M, De Maria GL, et al. Shockwave intravascular lithotripsy for the treatment of severe vascular calcification. Angiology. 71(8): 677-88 (2020).
[CrossRef] [Google scholar] [Pubmed]
- Lee MS, Shah N. The impact and pathophysiologic consequences of coronary artery calcium deposition in percutaneous coronary interventions. J Invasive Cardiol. 28(4): 160-7 (2016).
[Google scholar] [Pubmed]
- Kobayashi Y, Okura H, Kume T, et al. Impact of target lesion coronary calcification on stent expansion. Circ J. 78(9): 2209-14 (2014).
[CrossRef] [Google scholar] [Pubmed]
- Kassimis G, Raina T, Kontogiannis N, et al. How should we treat heavily calcified coronary artery disease in contemporary practice? From atherectomy to intravascular lithotripsy. Cardiovasc Revasc Med. 20(12): 1172-83 (2019).
[CrossRef] [Google scholar] [Pubmed]
- Morabito G, Tripolino C, Tassone EJ, et al. A case of stent under-expansion due to calcified plaque treated with shockwave lithoplasty. Cardiology. 141(2): 75-7 (2018).
[CrossRef] [Google scholar] [Pubmed]
- Alfonso F, Bastante T, Antuña P, et al. Coronary lithoplasty for the treatment of undilatable calcified de novo and in-stent restenosis lesions. JACC Cardiovasc Interv. 12(5): 497-9 (2019).
[CrossRef] [Google scholar] [Pubmed]
- McCutcheon K, Bennett J, Adriaenssens T. Double stent fracture and in‐stent restenosis due to nodular calcification treated with shockwave coronary intravascular lithotripsy. Catheter Cardiovasc Interv. 96(4): E455-7 (2020).
[CrossRef] [Google scholar] [Pubmed]
- Górny B, Balak W, Bielawski G, et al. Underexpanded stent in left anterior descending coronary artery treated with intravascular lithotripsy. Postepy Kardiol Interwencyjnej. 16(2): 216-8 (2020).
[CrossRef] [Google scholar] [Pubmed]