Case Report - Interventional Cardiology (2018) Volume 10, Issue 5
Crossover between low molecular weight heparin and unfractionated heparin in patients with acute coronary syndrome undergoing percutaneous coronary intervention: Clinical case report
- Corresponding Author:
- Si Dung Chu
ietnam National Heart Institute, Bach Mai Hospital., Hanoi, Vietnam
Tel: +84906086168
E-mail: dr.swiss.zhu@gmail.com
Received date: August 14, 2018 Accepted date: September 04, 2018 Published date: September 11, 2018
Abstract
Objective: Describe of Crossover between low molecular weight heparin (LMWH) and unfractionated heparin (UFH) in patient with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI). Method: Descriptive study, report clinical case has acute coronary syndrome undergoing percutaneous coronary intervention, the patient was crossover of LMWH and UFH. Results: A patientas female, 75 years old, admitted to Vietnam National Heart Institute on April, 2018. Reason for hospitalizationas left chest pain, shortness of breath. Medical examination showed the patient with acute coronary syndrome by left chest pain, ST segment elevation in V1 and V2, troponin T increased, suggest the Bloked of the Righ coronary artery (RCA) is the main cause. The result of scan of coronary arteries through radial artery was showed that RCA II is 80% blocked, RCA III is 99% blocked with blood clots. Left anterior descending (LAD) is completely bloked. LCX I is 95% bloked. Beside, collateral circulation is developed, which helps to nurture normal function of left heart muscles. We were conducted to the first PCI for two stent at RCA II and RCA III, the second PCI for the one stent at LCX I. We used crossover between LMW and UFH during PCI, undergoing two times PCI, the patient were conscious and no chest pain, estimate for the LAD by CTO-PCI method on the next time. Conclusion: Crossover between LMWH and UFH in patient with acute coronary syndrome undergoing percutaneous coronary intervention can make safe and more effective.
Keywords
Crossover, LMWH, UFH, acute coronary syndrome, PCI.
Introduction
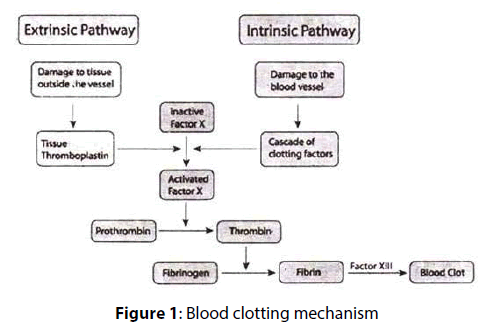
The role important of heparin in PCI, its anticoagulation mechanism, and dosage. Importance of use of heparin in percutaneous coronary intervention: Intravascular procedures using catheters , Catheters are synthetic and thrombogenic ➔ damaging tissues and in turn, triggering coagulation. Heparin has long been used during intravascular procedures to overcome the risk of coagulation. Intravascular procedures using catheters can never be completed without damaging tissues and in turn, triggering coagulation [1-3]. Blood clotting mechanism: There are two pathways for blood clotting: extrinsic and intrinsic. Both include the activation of thrombin [1-3]. So, how can heparin inhibit the coagulation?
Blood clotting mechanism: There are two pathways for blood clotting: extrinsic and intrinsic. Both include the activation of thrombin (Figure 1). So, how can heparin inhibit the coagulation?
The anticoagulant mechanism of heparin: Heparin does not have direct coagulation inhibition. Heparin binds competitively antithrombin (AT). Therefore, the coagulation reactions are inhibited (including the activation of XIIa, XIa, IXa, Xa factors and thrombin); so fibrin cannot be formed; finally, no clots are formed [1-3].
Unfractionated heparin dosage used during PCI: The first method’s Bolus injection with 1000-5000 IU right after catheterization, and maintaining IV of 1000 IU/L/hour. The second method’s Dosage can be calculated based on body mass is Bolus injection with 80 IU/kg, and maintaining IV of 18 IU/kg/h [2,4,5].
Proper dosage of UF heparin during PCI is extremely important and hard to monitor. So, proper dosage of heparin during PCI is: If it is too high, patients can develop hemorrhagic complications; If it is too low, anticoagulation effect of heparin is ineffective anticoagulation [5-7].
Previously, some reports showed that the risk of hemorrhagic, bleeding, bruising or embolism, ect... when the use of heparin duringg interventions as well as interventions in the thigh artery in common, so hematological monitoring during intervention is necessary [5-7].
Nowaday, We used to PCI through rotary artery’s common; Therefore, the use of heparin crossing is to be reconsidered. Our method’s crossover between low molecular weight heparin (LMWH) and unfractionated heparin (UFH) in patient with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI), the unfractionated heparin dosage during PCI with the method’s Bolus injection with 1000-5000 IU right after catheterization, and maintaining IV of 1000 IU/L/h, or the second method’s Dosage can be calculated based on body mass is Bolus injection with 80 IU/kg, and maintaining IV of 18 IU/kg/hour.
Case Description
Clinical and test presentation of patient with acute coronary syndrome
Admission: Female, 75 years old, admitted to Vietnam National Heart Institute on April 19, 2018. Reason for hospitalization: left chest pain, shortness of breath. Initial symptoms: sudden pain around left sternum, shortness of breath, with nausea and vomiting, no fever. Past medical history: No conditions have been discovered. 15 hours before entering the hospital, she started having left chest pain and shortness of breath. When she was admitted to the hospital, she still had sudden pain around left sternum, shortness of breath, with nausea and vomiting, no fever. She had no health conditions in the past.
Medical examination: Observation of vital signs, chest pain and abdomen. ECG, Blood test: Biochemical tests: Blood Urea, Creatinine, Electrolytes (Na+, K+, Cl- ), CK enzyme activity, CK-MB, Troponin T, ALT-AST. Complete blood count (CBC), Blood clotting test. Heart Ultrasound, Chest x-ray. Vital signs: Conscious, Glasgow score: 15, Body temperature: 36°C, P: 40 kg, h: 150 cm, IBM: 17.77 kg/m2 , Blood pressure: 130/80 mmHg, Heart rate: 67 bpm; but we heard unclear heart murmurs, no abnormal heart sounds, breathing rate’s 18 bpm, and her SpO2 was only 92%. Therefore, we had an indication’s supplied Oxygen at 2L/min. We did initial examination and the results are summarized as on the screen.
First, the patient was conscious with normal vital signs; However, She still had left chest pain. Lungs’s no rale, left chest pain, no edema, no abdominal pain, normal liver and spleen size, no weakness and paralysis, meningeal syndrome testing’s negative.
Biochemical test results: Normal liver and kidney functions, Normal electrolyte index, High blood glucose level (10.5 mmol/L), NT-proBNP level slightly increased (43.27 pmol/L), normal CK (112 U/L), CKMB (21 U/L) (tested 15 h after patient started having chest pain), increased troponin T (Increased Troponin T: 36.160 ng/L).
CBC and blood clotting tests: Indexes were in normal limits (RBC: 3.93 T/L, HGB: 116 G/L, PLT: 239 G/L, WBC 9.1 G/L), blood clotting tests (PT: 12.8 s, PT: 116%, PT-INR: 0.93, APTT: 26 s, Fibrinogen: 3.95 G/L)
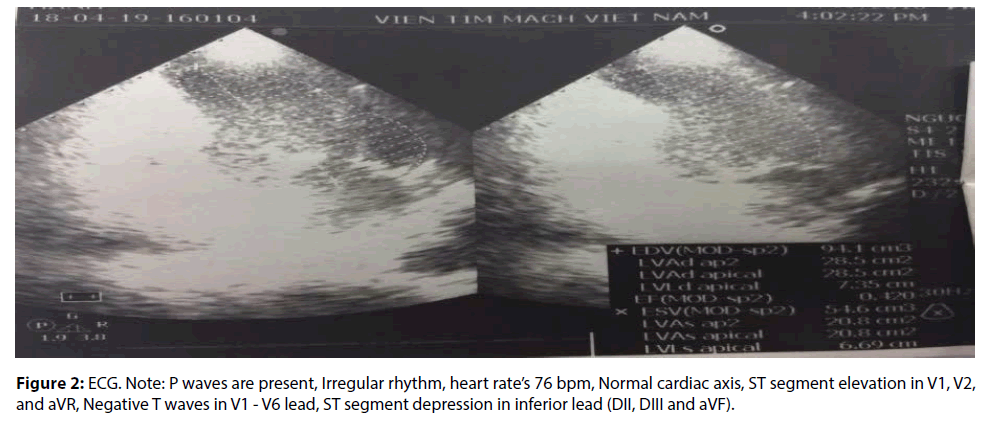
Heart ultrasound: Decreased motion of inferior interventricular septum - Increased left ventricle size - Left ventricular systolic function decreased (EF: 42- 46%) - Mild mitral valve prolapse - High pulmonary artery pressure: 49 mm (Figure 2).
Diagnosis: Patient had acute coronary syndrome.
Treatment
We conducted treatment including medication and Percutaneous coronary intervention (PCI). The patient was underwent two times for the PCI: The first second PCI for solving blockages in the Right coronory artery (RCA) II and RCA III branches. The second PCI for solving blockages in the left circumflex artery (LCX) branches. After the first and second PCI, patient was no hemorrhagic, no bleeding, normal CBC and blood clotting tests had indexes were in normal limits.
Medication in emergency and acute coronary care unit: We were used to Nitroglycerin drug (Dosage: 50 mL of diluted Nitroglycerin in Saline 0.9% IV at 3 mL/h), anesthetic and reducing pain drug, monitored by infusion pump. We were indicated to LMW heparin (Lovenox drug with 40 mg/0.4 mL, Subcutaneous, twice per day, 5-7 days), combination of Clopidogrel 75 mg and Acetylsalicylic acid 100 mg (DuoPlavin 75/100 mg × 1 tablet by oral, once per day, after meal), Enalapril drug (Zestril 5 mg × ½ tablet, Oral, once per day), Rosuvastatin drug (Crestor 10 mg × 1 tablet, oral, once per day, at 20:00 PM), and Esomeprazole (Nexium Mups 40 mg × 1 tablet, oral, once per day, at 20:00 PM).
Drugs used during PCI: Beside some drugs as anesthetic drug (diazepam) and reducing pain with morphine drug, We was used to Anti-coagulant’s Unfractionated Heparin (Enoxaparine sodium with 50 mL × 5 vials).
Further medication after the second PCI: Drug prescription Anti-platelet agents: combination of Clopidogrel (Plavix 75 mg × 1 tablet, oral, once daily, after meal) and Acetylsalicylic acid (Aspirin 80 mg × 1 tablet, oral, once daily, after meal), Angiotensinconverting enzyme (ACE) inhibitor: Lisinopril 5 mg (Zestril 5 mg x1 tablet, oral, ½ tabletet, once daily), Diuretics (Spiromide 50 mg/40 mg x1 tablet, daily morning), Rosuvastatin drug (Crestor 10 mg × 1 tablet, oral, once per day, at 20:00 PM), Anti-coagulant agent’s LMW heparin drug (Levonox 40 mg/0.4 mL x1, subcutaneous, twice daily, every 12 h). The patient took the drugs as shown on the above. After the second PCI, we did not use UFH, and We only used LMW Heparin from 5-7 days. We had a prognosis for this patient before the patient leave our hospital.
Discussion
Acute coronary syndrome
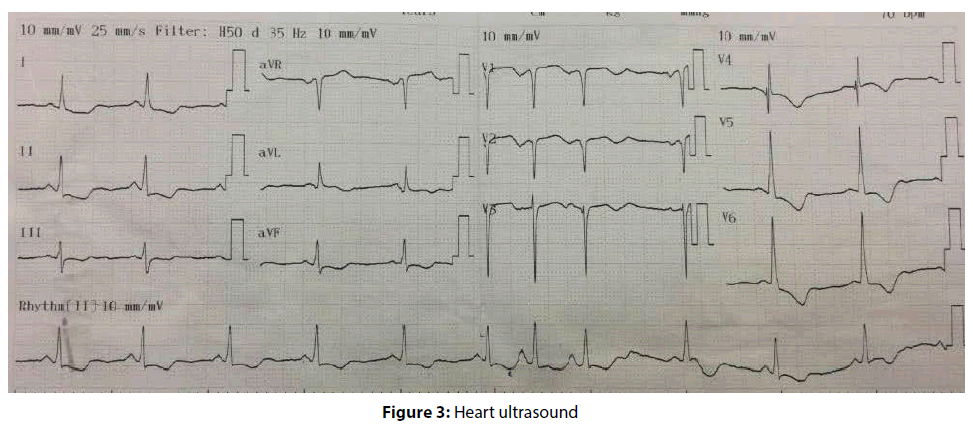
About ECG results, as you can see from the picture (Figure 3): P waves are present, Irregular rhythm, heart rate’s 76 bpm, Normal cardiac axis, ST segment depression in inferior lead (DII, DIII and aVF), ST segment elevation in V1, V2, and aVR; From that, we can conclude that the damage site is in right coronary arteries (RCA). Negative T waves in V1 to V6 lead, that indicates ischemia in many parts of heart muscles (Figure 4).
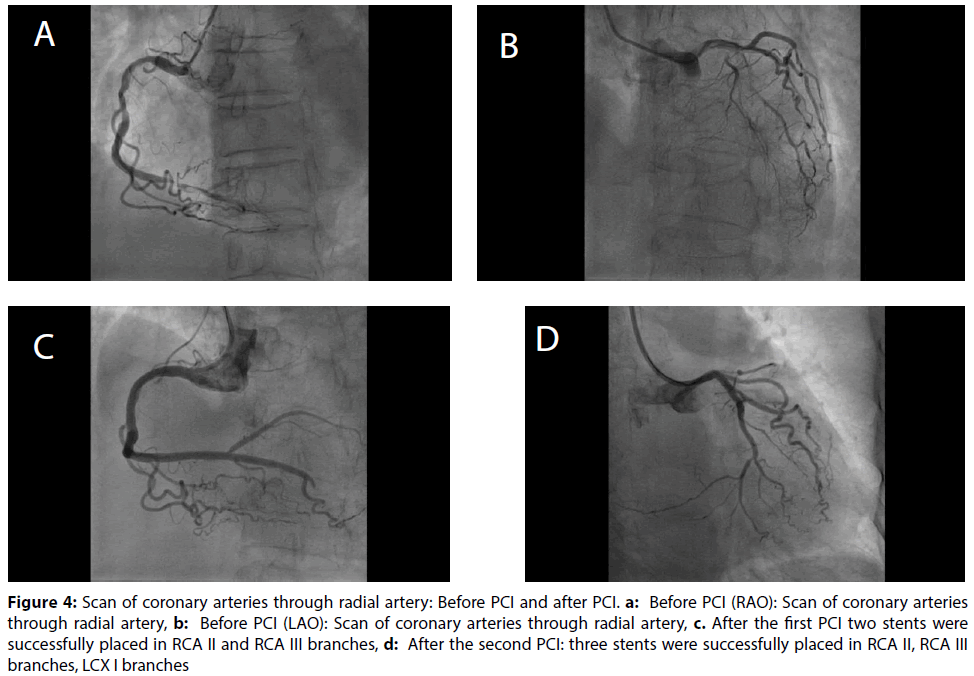
Figure 4: Scan of coronary arteries through radial artery: Before PCI and after PCI. a: Before PCI (RAO): Scan of coronary arteries through radial artery, b: Before PCI (LAO): Scan of coronary arteries through radial artery, c. After the first PCI two stents were successfully placed in RCA II and RCA III branches, d: After the second PCI: three stents were successfully placed in RCA II, RCA III branches, LCX I branches
We need to focus on the level of NT-proBNP, It increased, but the level was not too high, which means that the patient might have heart failure, but not an acute one. Normal CK and CK-MB, but It tested 12 h after (correct’s 15 h) patient started having chest pain. Also, Troponin T increased 15 h after the initial symptoms appeared, It indicates that the patient had acute coronary syndrome.
From all the results, we concluded that patient had acute coronary syndrome. We concluded that the patient had acute coronary syndrome based on three signs: (1) left chest pain, (2) ST segment elevation in V1, V2, and aVR lead, and (3) Troponin T increased (It tested 12 h after). We were also concluded that the damage site is in RCA branch [8,9].
Method treatment with crossover of Low MW and Unfractionated heparin
Medication and Percutaneous coronary intervention. So, we conducted treatment including medication and PCI [10,11].
Medication: The patient was prescribed with the list of drugs on the above, We use LMW heparin (Lovenox) and the combination of aspirin and Plavix (Duoplavin) [10,11].
Before PCI: Scan of coronary arteries through radial artery: The result confirmed that the RCA is the main cause with RCAII is 80% blocked, and RCAIII is 99% blocked with blood clots. Beside, the result was indicated that LAD is completely blocked, LCXI is 95% blocked, normal collateral circulation. Although left coronary artery system is completely blocked, collateral circulation is developed, which helps to nurture normal function of left heart muscles.
Drugs used during PCI: We were used to anymore Anti-coagulant’s unfractionated (Heparin 50 mL × 5 vials) while we used to LMW heparin (Lovenox) for this patients. In some developed countries, blood coagulation monitors are used to measure coagulation during PCI; But we did not use those machines by our clinical experiences were underwent for many years. Therefore, We Noted that Crossover of LMW and unfractionated heparin: LMW heparin is administered for 5-7 days before and after PCI, and Unfractionated heparin during PCI. So we call this drug combination as crossover of LMW and UFH.
The first PCI: As you can see from the diagram, after the first PCI, two stents were successfully placed in RCA II and III branches. Patient condition after the firts PCI: Patient were conscious, no chest pain, no shortness of breath, Pulse’s 76 bpm, Blood pressure’s 120/80 mmHg, no rales in lungs, normal abdomen, no hemorrhagic as well as no bleeding. We had a prognosis for this patient: we checked to status of patient after the first PCI for right anterior descending artery had good results, patient’s collateral circulation was shown to be good, patient was free of chest pain; While patient’s quite poor due to age (75 years old), long-developed condition, even though her LCX still had blockages and LAD was nearly completely blocked. Therefore, We had an early strategics for solving blockages in left circumflex artery (LCX artery) when patients gets well after the first PCI. After that, when patient gets well after the second PCI, the third can be conducted for solving blockages in left anterior descending artery (LAD artery) by CTO-PCI method in the next time.
The Second PCI: We were follow-up to after three days of the firts PCI, patient were conscious, no chest pain, no shortness of breath; normal vital signs, no hemorrhagic as well as the patient gets well after the fitst PCI; the second PCI was conducted for solving blockages in LCX artery. After the second PCI, one stent was placed in LCX branches’s successful. As our can see from the diagram (Figure 2), three stents were successfully placed in RCA II, RCA III branches and LCX branches. Patient condition after the second PCI: Patient were conscious, no chest pain, no shortness of breath, Pulse’s 75 bpm, Blood pressure’s 110/70 mmHg, no rales in lungs, normal abdomen. After 3 days of the second PCI, the Patient were conscious, no chest pain, no shortness of breath, normal vital signs, no hemorrhagic, normal CBC and blood clotting tests.
The patient took the drugs as shown on the above. After the second PCI, we did not use UFH, and We only used LMW Heparin from 5-7 days. We had a prognosis for this patient before the patient leave our hospital.
Short-term prognosis: PCI for right anterior descending artery had good results. PCI for LCX descending artery had good results. Patient’s collateral circulation was shown to be good. Patient was free of chest pain, even though her LAD still had blockages.
Long-term prognosis: The female patient, Quite poor due to age (75 years old). Long-developed condition. LAD was nearly completely blocked. Therefore, When patient gets well after the second PCI can be conducted for solving blockages in left anterior descending (LAD) artery by
CTO-PCI method.
We’re using crossover between LMWH and UFH in patient with acute coronary syndrome during CTO-PCI method when patient’s allready for solving blockages in the next time.
Conclusion
Crossover between LMWH and UFH in patient with acute coronary syndrome undergoing percutaneous coronary intervention can make safe and more effective.
References
- Resnick SB, Resnick SH, Weintraub JL, et al. Heparin in Interventional Radiology: A Therapy in Evolution. Semin Intervent Radiol. 22: 95-107 (2005).
- Kasper DL, Fausi A, Hauser S, et al. Harrison’s Principles of Internal Medicine, 19th edition. McGraw-Hill Companies, Inc, USA (2015).
- Zeymer U, Rao SV and Montalescot G. Controversies in cardiovascular medicine: Anticoagulation in coronary intervention. Eur Heart J. 37: 3376-3385 (2016).
- Cheem TH. Heparin has No Place as an Anticoagulant in PCI – A Protagonist’s View. ASEAN Heart J. 22: 14-18 (2014).
- Barbosa RR, Siqueira D, Coelho FM, et al. Crossover of Heparin Therapy and Bleeding Risk in Transradial Percutaneous Coronary Intervention in Acute Coronary Syndrome. Rev Bras Cardiol Invasiva. 20: 392-7 (2012).
- Mahaffey KW. Enoxaparin vs Unfractionated Heparin in Hight-Risk Patients With Non-ST Segment Elevation Acute Coronary Syndromes Managed With an Intended Early Invasive Strategy. JAMA, 292: 45-54 (2004).
- Kadakia MB, Desai NR, Alexander KP. Use of Anticoagulant Agents and Risk of Bleeding Among Patients Admitted With Myocardial Infraction. Cardiovasc Interv. 3: 1166-77 (2010).
- Fulde Gordian WO. Emergency Medicine: The principles of practice, 4th edition. Vaughn Curtis, Elsevier Australia (2005).
- Surawicz B and Knilans T. Chou’s Electrocardiography in clinical practice: Adult and Pediatric, 6th edition. Elservier Saunders (2008).
- Bonow RO, Braunwald E. Heart disease: a textbook of cardiovascular medicine. Elsevier Saunders, Philadelphia (2012).
- Lee CH, Cheng CL, Yang YHK, et al. Trends in the Incidence and Management of Acute Myocardial Infraction From 1999 to 2008: Get With the Guidelines Performance Measures in Taiwan. Journal of the American Heart, 3:e001066 (2014).