Editorial - Imaging in Medicine (2012) Volume 4, Issue 4
Current and future roles of molecular breast imaging in the community-based breast center
Jean M Weigert and Douglas A Kieper1Hampton University, School of Science, Center for Advanced Medical Instrumentation, Hampton, VA 23668, USA
2The Hospitals of Central Connecticut, 40 Hart Street, New Britain, CT 06052, USA
- *Corresponding Author:
- Jean M Weigert
The Hospitals of Central Connecticut
40 Hart Street, New Britain
CT 06052, USA
E-mail: jweigert@pol.net
Abstract
Keywords
breast imaging; breast-specific gamma imaging; mammography; molecular breast imaging; sestamibi; tetrofosmin; ultrasound
Nearly all modern breast centers are dependent on two primary forms of anatomical breast imaging: x-ray mammography and ultrasound. With these modalities, breast cancers are detected based on anatomical features that present as secondary deformations due to the underlying pathologies. Although this imaging approach is quite effective for the majority of breast cancer patients, the sensitivity of these techniques in patients with dense or complex breast tissue can be significantly diminished, particularly in the high-risk population [1].
Molecular breast imaging (MBI), also referred to as breast-specific gamma imaging (BSGI), is a metabolic imaging procedure typically conducted using the radiotracers 99mTc-sestamibi or 99mTc-tertofosimin. This type of imaging differs from mammography and ultrasound in that it provides physiological imaging of the malignant process, specifically the hyperplastic nature of malignant breast lesions. It should be noted that while either tracer may be used in Europe, only Sestamibi is approved for breast imaging in the USA. This imaging modality has demonstrated high sensitivity in both the fatty and dense breast and has been shown to improve the sensitivity of breast cancer detection when added to mammography and ultrasound in the diagnostic work-up of patients [2].
Unlike its predecessor, scintimammography or mammoscintigraphy, which was conducted with standard, large field-of-view (LFOV) gamma cameras, the MBI/BSGI technique uses breast-optimized gamma cameras that allow the breast to be compressed between a small detector and a compression paddle or between two small detectors. Nearly 100 peer-reviewed papers dating back more than 15 years have documented the experience of breast imaging with Sestamibi and Tetrofosmin [3]. In addition, several studies comparing standard and optimized camera designs have provided evidence that the breastoptimized designs improve the clinical accuracy of this procedure, especially in sensitivity for sub-cm lesions [4]. Clinical evidence demonstrating the increased lesion sensitivity of MBI/BSGI over scintimammography is now available [5]. In addition, there have been several publications indicating that the sensitivity and specificity for BSGI/MBI are both approximately 89–96 and 65–90%, respectively [6–9].
According to the Breast Scintigraphy Procedure Guidelines for Tumor Imaging issued by the European Association of Nuclear Medicine in 2003 and the Society of Nuclear Medicine Guideline for Breast Scintigraphy with Breast-Specific Gamma Cameras in 2010, breast imaging should be conducted using a dose of 740–1110 MBq (20–30 mCi) [101,102]. This dose was determined largely by the low photon sensitivity of the standard gamma camera systems when equipped with highresolution collimators. Since that time, several breast-optimized gamma camera systems have been developed with three- to five-times higher photon sensitivity, which may make imaging with lower doses possible.
99mTc-Sestamibi and 99mTc-Tetrofosmin are 140 KeV gamma ray-emitting isotopes in a lipophilic cation molecule. They are injected intravenously and are retained in cells probably by electronegative cellular and mitochondrial membrane potentials. Studies show that this accumulation is roughly proportional to blood flow, desmoplastic activity and cellular proliferation, and therefore accumulation is higher in breast cancers compared with surrounding tissues [10,11]. Both tracers are lipophilic substrates for the P-glycoprotein (Pgp), a cellular efflux pump for various compounds. Therefore, these tracers exhibit rapid tumor wash-in (within ~2 min) followed by a slow tumor washout (over the course of several hours) [12,13]. Based on these factors, imaging can begin within minutes after injection and can continue for up to approximately 90 min postinjection, providing ample time for all required views to be conducted before the washout cycle negatively impacts lesion-to-background tracer concentration ratio. Some authors have suggested that since tumor expression of Pgp is also related to multidrug resistance, comparing early MBI/BSGI images (within 15 min postinjection) and delayed imaging (2–3 h postinjection) may help to identify tumors that are resistant to chemotherapy, but this is not currently common practice [14,15].
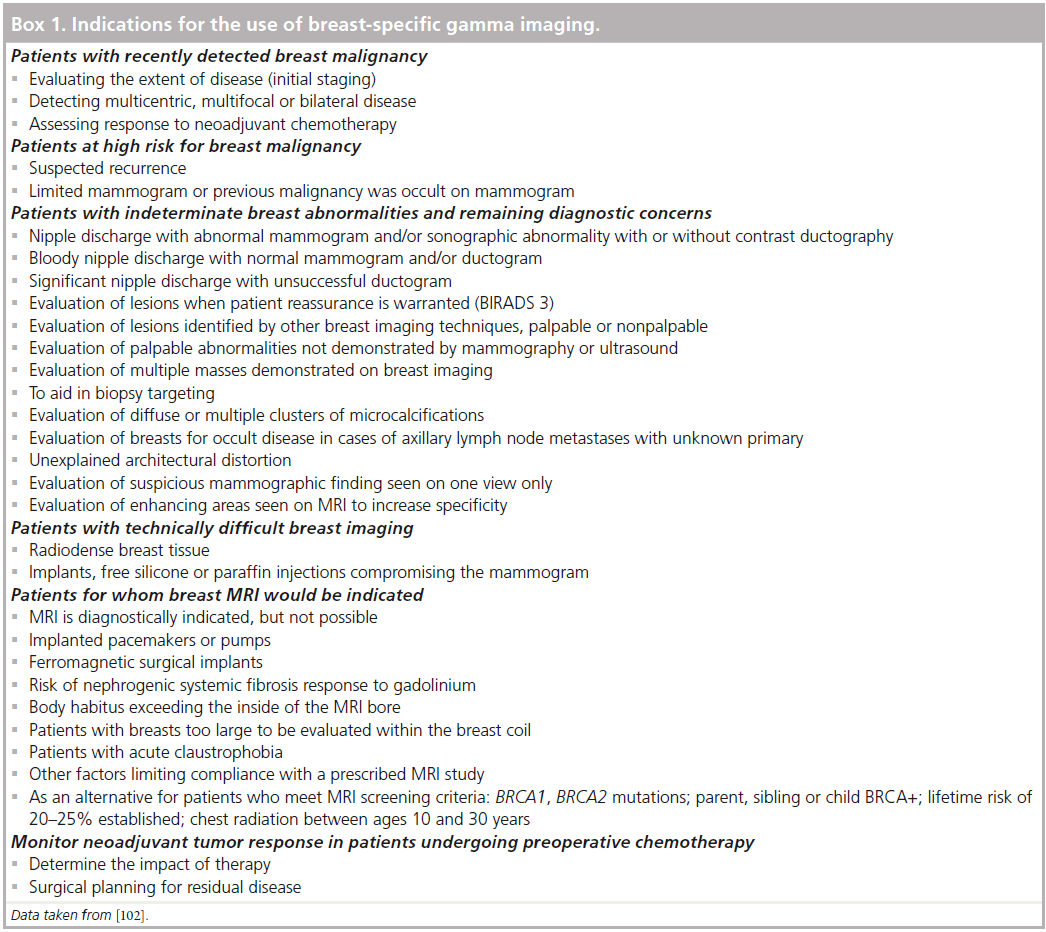
According to the Society of Nuclear Medicine Guideline for Breast Scintigraphy with Breast- Specific Gamma Cameras, there are several potential indications for the use of this imaging technology (Box 1) [102].
“Clinical evidence demonstrating the increased lesion sensitivity of molecular breast imaging/breast-specific gamma imaging over scintimammography is now available ... there have been several publications indicating that the sensitivity and specificity for breast-specific gamma imaging/molecular breast imaging are both approximately 89–96 and 65–90%, respectively.”
From the available data, it appears that these new detector technologies may reduce the dose required to conduct breast imaging with 99mTc-MIBI or dramatically improve image quality compared with those from the standard gamma camera systems using the same 740 MBq dose [16]. Reducing the dose from 740–1110 MBq (20–30 mCi) to 259–370 MBq (7–10 mCi) can reduce patient radiation exposure by nearly a factor of 3; however, as with all radiologic procedures, lower doses increase image noise, which will make the visualization of small, low-contrast lesions more difficult. The radiation exposure from a 259 MBq (7mCi) injection of MIBI is approximately 2 millisieverts and is approximately equivalent to the radiation dose patients receive from the combination of screening and diagnostic mammograms.
It is important to note that while several manufacturers of breast gamma cameras are promoting the use of doses as low as 74–148 MBq (2–4 mCi) there is no peer-reviewed published clinical data to validate the sensitivity of low- dose BSGI/MBI. Of the more than 100 articles published on BSGI/MBI imaging has been conducted using a dose of 740 MBq or more.
There are several references available to help understand the potential health risks of radiation exposure. The first, according to a statement from the Health Physics Society:
“There is substantial and convincing scientific evidence for health risks following high-dose exposures. However, below 5–10 rem [per year], risks of health effects are either too small to be observed or are nonexistent.”
– Health Physics Society [103].
Based on their findings, they recommended against estimating the risk from radiation effective dose of less than 5 rem per year or 10 rem in a lifetime. Using a dose of 740 MBq, this equates to approximately eight BSGI/MBI studies in a single year or 16 in a lifetime. The NIH’s radiation dose risk model estimates the likelihood of a radiation-induced cancer from the 740 MBq dose of MIBI to be 24 cancers per 1000,000 examinations, 0.024% [104].
Determining the optimal imaging dose is an important part of establishing an institutional protocol and several factors must be considered. The primary consideration should be a risk versus benefit analysis based on specific indications. For the typical diagnostic patient, the primary concern should be image quality, while for the asymptomatic screening patient the radiation dose should be minimized. Second, one must consider how to address the relatively broad variation (standard deviation: ±39%) of breast tissue uptake that has been documented in the clinical literature [105]. Therefore the clinician must either choose a dose high enough to ensure good image quality for all patients or be willing to increase imaging time for patients on the low end of the uptake range.
The currently available clinical literature provides convincing evidence that the 99mTc- Sestamibi-based MBI/BSGI technique is a useful diagnostic adjunct to mammography and ultrasound. There are three primary areas for future development: methods and impact of radiation dose reduction; evaluation of its role in breast cancer screening; and investigation into new radiotracers for breast tumors.
As presented in the section above, the patient radiation exposure in MBI/BSGI is delivered via the radiotracers injected for imaging and the new breast-optimized detector systems provide higher photon sensitivity. This increased detector sensitivity could be used to lower the dose of radiotracer required for this procedure, but there is not yet sufficient data to establish the clinical efficacy of this imaging procedure at lower doses. The Mayo clinic (MN, USA) and other research institutions in the USA are in the process of conducting clinical trials to evaluate the effectiveness of the low-dose procedure and several groups believe that further dose reduction is achievable using an opposed, dual head system with imaging fusion. Such a system would allow a simultaneous acquisition of the breast image from two detectors thus doubling the system photon sensitivity of a single head detector design. However, there may be some significant technical limitations to this approach. First, the breast is a heterogeneous organ comprised of fat, glandular tissue and connective tissue. Each of these tissues has a different metabolic rate, and thus radiotracers can have a different uptake ratio in each tissue type. This can result in a patchy appearance in the MBI/BSGI image. In such cases, the image fusion required to reduce the dose can magnify the patchiness and cause confusion. This occurs since each detector sees the near-field patchiness a bit better than the other. Think of it as superimposing two maps of the same area, which are very similar, but not exactly the same and then trying to read the fused result. The impact of this image fusion on the procedure’s specificity needs to be examined. Second, while the single head system allows sufficient access for image-guided needle biopsy to be conducted, the presence of two detectors on opposite sides of the breast may make access to the breast for biopsy significantly more difficult. The third complication is system cost. Such a dual head system costs approximately twice as much as the single head design. This is an area of significant research and interest that should be better understood in the next few years.
“Mammography will probably remain the primary tool for breast cancer screening, but low-dose molecular breast imaging/breast-specific gamma imaging may be useful in specific subsets of patients, such as those with dense breast tissue and an elevated risk of disease.”
According to the Society of Nuclear Medicine Guidelines and the American College of Surgeons, MBI/BSGI is a useful modality for patients who require additional diagnostic imaging [17]. There is limited data on the use of this procedure in screening the asymptomatic population for disease. There are several ongoing studies that may help expand the role of MBI/BSGI into the screening applications, but this will probably not gain broad acceptance without the dose reduction effort. While there is a significant prevalence of malignancy in the diagnostic population, the prevalence of disease in the screening group is much lower, thereby changing the risk-to-benefit ratio. Mammography will probably remain the primary tool for breast cancer screening, but lowdose MBI/BSGI may be useful in specific subsets of patients, such as those with dense breast tissue and an elevated risk of disease.
The development of breast-optimized gamma cameras has sparked new interest in radiotracers that target breast lesions. The new generation of drugs may expand the use of MBI/BSGI beyond the area of breast cancer diagnosis and into a new role of treatment planning. One example is Z-123I-MIVE, an estrogen receptor-specific compound. This compound allows in vivo imaging of the tumor estrogen receptor status and may allow the clinician to determine whether the tumor will be responsive to hormone therapy.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as: *of interest
- Berg WA, Blume JD, Cormack JB et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 299(18), 2151–2163 (2008).
- Weigert J, Bertrand M, Stern L, Kieper D. Results of a multicenter patient registry to determine the clinical impact of breast-specific gamma imaging, a molecular breast imaging technique. AJR 198(1), W69–W75 (2012). & Provides an analysis of the impact of breast-specific gamma imaging on patient management in the community breast center.
- Hussain R, Buscombe JR. A meta-analysis of scintimammography: an evidence-based approach to its clinical utility. Nucl. Med. Commun. 27(7), 589–594 (2006). & Excellent resource for the history of Sestamibi breast imaging that provides compiled data from many sources.
- Brem R, Kieper D. Rapelyea J. Majewski S. Evaluation of a high-resolution, breastspecific, small-field-of-view gamma camera for the detection of breast cancer. Nucl. Instr. Meth. 497(1), 168–173 (2003).
- Brem RF, Schoonjans JM, Kieper DA, Majewski S, Goodman S, Civelek C. High-resolution scintimammography: a pilot study. J. Nucl. Med. 43, 909–915 (2002).
- Tadwalkar RV, Rapelyea JA, Torrente J et al. Breast-specific gamma imaging as an adjunct modality for the diagnosis of invasive breast cancer with correlation to tumour size and grade. Br. J. Radiol. 85(1014), e212–e216 (2011). & Good resource and analysis of the types and sizes of malignancies detected with molecular breast imaging/breast-specific gamma imaging.
- Rosenberg A, Kieper DA, Williams MB, Johnson N, Lanzkowsky L. The role of molecular imaging technologies in breast cancer diagnosis and management. In: Imaging of the Breast – Technical Aspects and Clinical Implication. Tabar L (Ed.). InTech Publishing, Rijeka, Croatia, 179–196 (2012). n Excellent educational resource on the basics of breast-specific gamma imaging/molecular breast imaging and current clinical data.
- Zhou M, Johnson N, Gruner S et al. Clinical utility of breast specific gamma imaging for evaluating disease extent in the newly diagnosed breast cancer patient. Am. J. Surg. 197(2), 159–163 (2009).
- Zhou M, Johnson N, Blanchard D, Bryn S, Nelson J. Real-world application of breast-specific gamma imaging, initial experience at a community breast center and its potential impact on clinical care. Am. J. Surg. 195 (5), 631–635 (2008).
- Carvalho PA, Chiu ML, Kronauge JF et al. Subcellular distribution and analysis of technetium-99m-MIBI in isolated perfused rat hearts. J. Nucl. Med. 33, 1516–1521 (2002).
- Piwnica-Worms D, Kronauge JF, Chiu ML. Uptake and retention of hexakis (2-methoxyisobutyl isonitrile) technetium (I) in cultured chick myocardial cells. Mitochondrial and plasma membrane potential dependence. Circulation 82, 1826–1838 (1990).
- Cutrone JA, Yospur LS, Khalkhali I, Tolmos J, Devito A, Diggles L. Immunohistologic assessment of technetium-99m-MIBI uptake in benign and malignant breast lesions. J. Nucl. Med. 39, 449–453 (1998).
- Piwnica-Worms D, Chiu ML, Budding M, Kronauge JF, Kramer RA, Croop JM. Functional imaging of multidrug-resistant P-glycoprotein with an organotechnetium complex. Cancer Res. 53, 977–984 (1993).
- Ballinger JR, Hua HA, Berry BW, Firby P, Boxen I. 99mTc-Sestamibi as an agent for imaging P-glycoprotein-mediated multidrug resistance: in vitro and in vivo studies in a rat breast tumour cell line and its doxorubicin-resistant variant. Nucl. Med. Commun. 16, 253–257 (1995).
- Moretti JL, Caglar M, Boaziz C, Caillat- Vigneron N, Morere JF. Sequential functional imaging with technetium-99m hexakis-2- methoxyisobutylisonitrile and indium-111 octreotide: can we predict the response to chemotherapy in small cell lung cancer? Eur. J. Nucl. Med. 22, 177–180 (1995).
- Hruska CB, O’Connor MK, Collins DA. Comparison of small field of view gamma camera systems for scintimammography. Nucl. Med. Commun. 26 (5), 441–445 (2005).
- Silverstein M, Recht, A, Lagios MD et al. Image-detected breast cancer: state-of-the-art diagnosis and treatment. J. Am. Coll. Surg. 209(4), 504–520 (2009).
„„ Websites
- Breast Scintigraphy Procedure Guidelines for Tumor Imaging, European Association of Nuclear Medicine. www.eanm.org/publications/guidelines/ gl_onco_breast.pdf
- SNM Guideline for Breast Scintigraphy with Breast-Specific Gamma Cameras 1.0. Society of Nuclear Medicine. http://interactive.snm.org/docs/ BreastScintigraphyGuideline_V1.0.pdf & Provides a reference to the current clinical practice of breast-specific gamma imaging/molecular breast imaging.
- Health Physics Society. Radiation Dose in Perspective. www.hps.org/documents/radiationrisk.pdf
- NIH RSC Report: Improving Informed Consent for Research Radiation Studies (2001). http://drs.ors.od.nih.gov/services/rsc/forms/ informed_consent.pdf
- Kieper DA. Böhm-Vélez M. Breast imaging using Tc99m-Sestamibi: can lower doses be used for breast-specific gamma imaging/ molecular breast imaging? http://ipp.myesr.org/esr/ecr2012/index.php? v=posterd&poid=102909&ippwwwsid=5jnh o9nq3agreqirle8hkru2l2


