Case Report - Imaging in Medicine (2020) Volume 12, Issue 4
Deep neck space infection, unusual progressing to mediastinitis in a COVID-19 patient: A case report
Akif İşlek1* & Sadullah Şimşek21Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey
2Nusaybin State Hospital, Radiology Clinic, Mardin, Turkey
- Corresponding Author:
- Akif İşlek
Nusaybin State Hospital
Otolaryngology-Head & Neck Surgery Clinic
Mardin, Turkey
E-mail: drakifislek@gmail.com
Abstract
Objective: Deep neck space infections most commonly originated from an oral infection focus and may show rapid progression to mediastinitis with conditions like an immunodeficiency. This report aims to examine the management of deep neck infection in a COVID-19 positive patient.
Case Summary: A 43yr old woman diagnosed as a deep neck space infection with under routine hemodialysis treatment and COVID-19 positive. Laboratory findings, imaging results, treatment protocol and clinical course of the patient were presented. The patient was a complaint of swelling, hyperemia, and pain in the neck with one-day history. Physical examination, ultrasonography and computerized tomography revealed deep neck space infection and superior mediastinitis. The initial laboratory results revealed a leukocytosis of 3.22/μL (83% Neutrophil and 16% lymphocyte) and a C-reactive protein of 68.6?mg/dL and positive Sars-Cov-2 rapid antibody test. A real-time plasma chain reaction confirmed the diagnosis COVID-19.
Conclusions: COVID-19 can adversely affect the morbidity of deep neck infection, like human immunodeficiency virus disease and other immunodeficiency conditions.
Keywords
COVID-19 ■ Deep neck space infection ■ Mediastinitis ■ Sars-CoV-2
Highlights
1. COVID-19 disease aggravates deep neck space infection.
2. Mechanism of the disease progression depends on the lymphopenia or leukopenia
3. Lymphadenitis may occur in COVID-19 disease
Introduction
Deep Neck Space Infections (DNI) most commonly originated from a septic focus of the mandibular teeth, tonsils, parotid gland, middle ear or sinuses, usually with a rapid onset and frequently with progression to lifethreatening complications. Mortality rises up to 40% with the presence of mediastinal extension [1]. Underlying immunocompromised individuals, risk factors, including diabetes mellitus, alcoholism, cirrhosis, arteriosclerosis, human immunodeficiency virus (HIV), corticosteroid therapy, chronic renal failure, malignancy, intravenous drug abuse, and obesity may predispose the patients with DNI to necrotizing fasciitis or may increase the risks or morbidity or mortality disease [2]. In this report, a COVID-19 patient with a deep neck infection with rapid progression as predicted by poor prognostic factors and subsequently an unexpectedly rapid recovery of this patient was presented. The institutional review board was approved by the Provincial Health Directorate for this case report.
Case Report
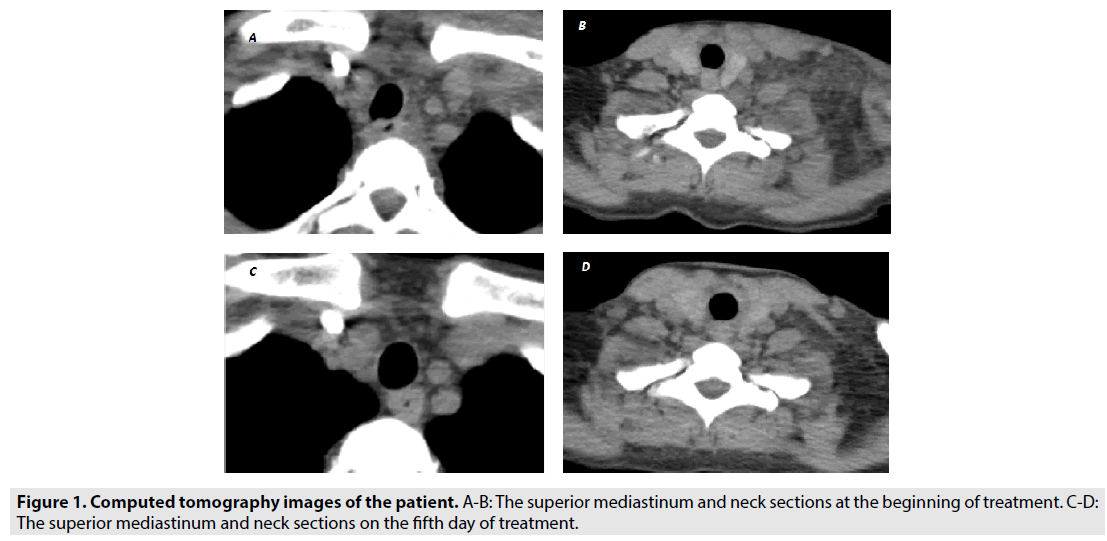
A 43yr old woman with chronic kidney failure and undergoing routine hemodialysis treatment was consulted to the otolaryngology clinic. In the anamnesis, there was swelling, hyperemia and pain in the neck, which continued for one day with a history of toothache and caries. On physical examination, there was swelling on the left neck between the midline of the neck, the mandible and the clavicle, diffuse stiffness in the skin, and tenderness with hyperemia. Ultrasonography (USG) indicated edema in deep tissues in the neck, increased echogenicity, reactive lymphadenitis, and impaired fat-fascia plans with no abscess or jugular vein thrombosis. Computerized tomography (CT) revealed infection-compatible findings in muscle and fascia layers starting from the submandibular space and extending to the upper mediastinum along the carotid sheath. CT showed no COVID-19 related lesions or other pathology in the lungs. The initial laboratory results revealed a leukocytosis of 3.22/μL (83% Neutrophil and 16% lymphocyte) and a C-reactive protein of 68.6 mg/dL. Due to the COVID-19 pandemic and possible surgical indications, Sars-CoV-2 rapid antibody test was performed with routine blood tests before hospitalization. Since the rapid antibody test was found to be positive, the patient was isolated and antibiotherapy was started according to creatine clearance. Treatment was determined as Piperacillin/ Tazobactam 4g/0.5g × 3/day, ciprofloxacin 200 mg × 1/day, Hydroxychloroquine 400 mg × 2 /first day (then 200 mg BID for 5-10 days), and Favipiravir 200 mg × 8/first day (days 2–5: 600 mg BID). CT and USG on the 5th day of treatment showed that the patient's neck findings regressed. Laboratory examinations also correlated with imaging methods and clinical findings. Hydroxychloroquine and Favipiravir was removed from the treatment on the fifth day, as no evidence of acute respiratory distress syndrome appeared, and the patient was discharged after completing antibiotherapy for ten days (FIGURE 1A-D).
Discussion
COVID-19 is a pandemic that broke out in December 2019, and the medical literature seems to have to reorganize its current diagnosis and treatment according to the pandemic [3]. Viral related head and neck diseases that may lead to deep neck infections are complicated lymphadenitis or sialoadenitis, and coronavirusassociated lymphadenitis has been previously reported in the literature [4]. In this case, reactive lymph nodes were shown by USG in the neck, but abscess formation was not detected. Coronavirus infection-induced tissue damage is more possible due to the human immune system response [5]. Therefore, coronavirus infection is more likely to be a poor prognostic factor for mortality and morbidity as in HIV infection for deep neck infection [2]. Similarly, mediastinitis was detected one day after the onset of symptoms in this patient. However, the progression of mediastinitis, no respiratory distress or hypoxaemia was detected in the patient. Although COVID-19 was proved by PCR in the case, the symptoms and clinical findings described in the recent literatüre has not occurred. COVID-19 was asymptomatic in this case according to known morbidity and mortality, and COVID-19 treatment was stopped on the fifth day. Rapid improvement of DNI in this patient has been attributed to the asymptomatic course of COVID-19 and to start treatment very early.
Conclusion
COVID-19 can adversely affect the morbidity of deep neck infection, like HIV disease and other immunocompromised conditions. During the Sars-CoV-2 pandemic, it should be kept in mind that special cases such as deep neck space infection may go with a worse prognosis. Because COVID-19 causes lymphopenia in the blood, DNSI can progress rapidly to complications with high mortality, such as mediastinitis. In addition, early treatment with appropriate antibiotics or antibiotic combinations affects the prognosis as much as the patient's immune status, as in this reported patient.
Acknowledgements
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest/Competing interests
The authors declare no conflict of interest.
References
- Velhonoja J, Lääveri M, Soukka T et al. Deep neck space infections: an upward trend and changing characteristics,” Eur. Arch. Oto-Rhino-Laryngology. 277, 863-872, (2020).
- Gunaratne DA, Tseros EA, Hasan Z et al. Cervical necrotizing fasciitis: Systematic review and analysis of 1235 reported cases from the literature. Head. Neck. vol. 40, 2094-2102, (2018).
- Wang K, Kang S, Tian R et al. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin. Radiol. 75, 341-347, (2020).
- Bastien N, Anderson K, Hart L et al. Human Coronavirus NL63 Infection in Canada. J. Infect. Dis. 191, 503-506, (2005).
- Li G, Fan Y, Lai Y et al. Coronavirus infections and immune responses, J. Med. Virol. 92, 424-432, (2020).