Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 7
Diagnosis of sclerodermatomyositis in Ethiopian woman
- *Corresponding Author:
- Abilo Tadesse
Department of Internal Medicine, College of Medicine and health Sciences, University of Gondar, Gondar, Ethiopia
E-mail: abilo.tadesse@yahoo.com
Abstract
Background: Sclerodermatomyosits is an overlap syndrome diagnosed when systemic sclerosis and dermatomyositis are observed in one patient, which develops simultaneously or sequentially. The American College of Rheumatology - European League against Rheumatism (ACR-EULAR) classification Criteria was implemented to define both diseases.
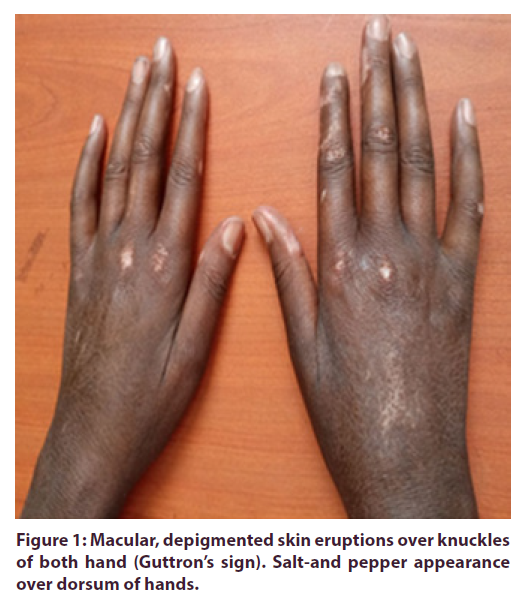
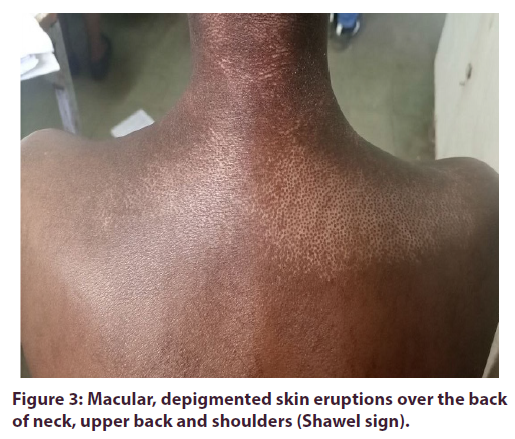
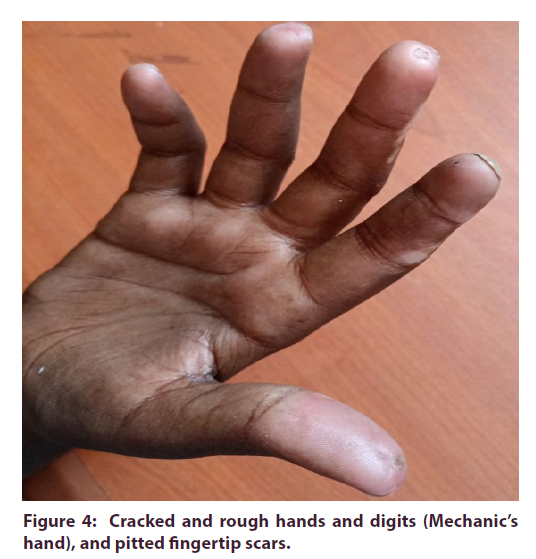
Case presentation: A 36-year-old female patient was presented with excessive clumsiness and sleepiness of one year duration. She was diagnosed with hypothyroidism and was started on levothyroxine. She noticed associated white-blue-red discoloration of digits upon exposure to cold, diffuse skin thickening and tightness, dysphagia to solid foods, constipation, and difficulty of standing up from a toilet seat, holding objects, and combing hair. She was tired all the time, had muscle aches, and had lost her appetite and weight. On physical examination, vital signs were within normal limits. She had diffuse scleroderma-like skin changes with a salt-and-pepper appearance over extremities, neck and trunk. She had erythematic skin eruptions over the palpebrae (heliotrope rash), and depigmented skin lesions over the knuckles (Guttron’s sign), neck and chest (V-sign), and back (Shawl sign), rough and cracked hands (mechanic’s hands) and pitted fingertip scars. She had difficulty of getting out of a chair and lifting objects. Skeletal muscle enzyme was elevated and muscle biopsy revealed muscle fiber atrophy with collagenous fibrosis. Diagnoses of systemic sclerosis and dermatomyositis were settled by ACR-EULAR classification criteria.
Conclusion: The patient described had sclerodermatomyositis using ACR-EULAR Classification Criteria. A high index of clinical suspicion is required to diagnose this rare disease in resource-limited settings to prevent adverse outcomes.
Keywords
sclerodermatomyositis • acr-eular classification criteria
Abbreviations: ACR-EULAR: American College of Rheumatology-European League against Rheumatism; ANA: Anti-Nuclear Antibody; ASS: Anti-Synthetase Syndrome; DM: Dermatomyositis; EMG: Electromyography; MCTD: Mixed Connective Tissue Diseases; PM: Polymyositis; RA: Rheumatoid Arthritis; RF: Rheumatoid Factor; SSc: Systemic Sclerosis; SLE: Systemic Lupus Erythematosus; SS: Sjogren’s Syndrome
Introduction
Background
Overlap syndrome is diagnosed when at least two classical connective tissue diseases are observed in one patient, which develops simultaneously or sequentially (1, 3, 5, 7). It includes a combination of Systemic Lupus Erythematosis (SLE), Rheumatoid Arthritis (RA), Systemic Sclerosis (SSc), Dermatomyocytis/Polymyositis (DM/PM), and Sjogren’s Syndrome (SS). When systemic sclerosis coexists with dermatomyositis, it is named as sclerodermatomyositis. It clinically manifests with scleroderma-like skin changes, myalgia/myositis, Raynaud’s phenomenon, dysphagia/esophageal hypomotility, interistial lung disease and positive anti-Pm/Scl antibody (10-12). Here, we report a rare clinical disorder named as sclerodermatomyositis.
Case presentation
A 36-year-old female patient was relatively healthy one year ago, after which she started to experience excessive clumsiness and sleepiness. She visited a health institution, and was diagnosed with hypothyroidism. She was started on levothyroxine 150 mg PO daily, and got significant improvement. She had noticed associated white-blue-red discoloration of the digits upon exposure to cold, which later became ulcerated at the fingertips. Three months later, she experienced skin tightness with vitiligo-like skin lesions over her extremities, neck and trunk. She had difficulty opening her mouth wide, dysphagia for solid foods, constipation, dryness of mouth and eyes, joint stiffness with limited movement, and menstrual irregularities. Six months later, she began to have difficulty standing up from a toilet seat, lifting objects, combing hair and holding up her head. She suffered from fatigue, malaise, muscle ache, loss of appetite, and weight loss. There was no previous history of join swelling. There was no history of coughing or phlegm. No history of dyspnea, orthopnea or palpitation. There was no history of visual disturbance or weakness of extremities. There was no history of diabetes mellitus, confirmed malignancy, exposure to toxic drugs or chemicals, or family history of similar illness. During the physical examination, she was conscious and oriented. Vital signs were Blood Pressure (BP) = 110/80 mmhg, Pulse Rate (PR) = 86 beats/minute, Respiratory Rate (RR) = 22 breaths/ minute, Temperature (T0) = 36.70C, Sa02 = 94% while breathing in room air. She had erythematous eruptions over both upper eyelids (Heliotrope rash). She had pink conjunctivae and non-icteric sclerae. She couldn’t open her mouth wide (reduced mouth aperture). No enlarged thyroid gland or lymph nodes at accessible sites. The chest was resonant to percussion and clear to auscultation. Heart sounds were well heard, and there was no murmur or gallop. The abdominal examination revealed no enlarged organs or signs of ascites. She had limited extension at the elbow and knee joints, and tendon friction rubs at the ankle and wrist joints on locomotor examination. On integumentary examination, there was diffuse skin thickening and tightness with a salt-andpepper appearance on the upper and lower extremities, neck and trunk. The Modified Rodnan Skin Score (MRSS) was 32/51. There were scaly, depigmented skin lesions over the knuckles (Gottron’s sign) (Figure 1), V-shaped distributed, depigmented skin lesions over the anterior neck and chest (V-sign) (Figure 2), and back and shoulders (Shawl sign) (Figure 3). There was roughening and cracking over the hands and digits resembling ‘manual laborer’ hands (Mechanic’s hands), and pitted fingertip scars (Figure 4). On neurologic examination, she was alert and oriented in time, place and person. No cranial nerve palsy. She had difficulty getting out of a chair, holding objects, and combing her hair. Sensation was intact. No meningeal irritation signs. On laboratory tests, WBC=5.61x103/μl (N=54.1%, L=44.7%) (normal range, 4.5-11.0 x103/μl) Hgb=15.4 gm/dl (normal range, 12-18 gm/dl), platelets=409x103/ μl (normal range, 150-450 x103/μl), ESR=30 mm in the first hour (normal range, 1 mm/hr to 25 mm/hr). Urinalysis was non-revealing. Liver biochemical tests and renal function tests were within normal limits. Serum creatine kinase level =616 IU/L (normal range, 29 IU/L to 168 IU/L). Thyroid function tests revealed serum Thyroid Stimulating Hormone (TSH) level = 12.54 μU/ ml (normal range, 0.35 μU/ml to 4.94 μU/ml), serum T4 = 7.68 μg/dl (normal range, 4.5 μg/dl to 10.9 μg/dl), serum T3 = 59 ng/dl (normal range, 60 ng/dl to 181 ng/ dl). A serum test for Antinuclear Antibody (ANA) was positive. Serum titer for Rheumatoid Factor (RF) was within normal limits (<20 IU/ml; normal range, 0 IU/ ml to 30 IU/ml) (Table 1). Other immunoassay panels were not done due to a limited clinical setup. Chest x-ray disclosed no abnormalities. Chest CT revealed no abnormalities. ECG indicated normal findings.
| Variables | Lab. values on admission | Reference |
|---|---|---|
| Hemogram | ||
| White blood cells (x103/µl) | 5.61 | 4.5-11.0 |
| Hemoglobin (gm/dl) | 15.4 | 12.0-18.0 |
| Platelets (x103/µl) | 409 | 150-450 |
| ESR (mm/hr) | 30 | Jan-25 |
| Urinalysis | 1+ | |
| Protein | Negative | - |
| Glucose | - | |
| 24-hr protein (mg/day) | 500 | < 150 |
| Liver biochemical tests | ||
| ALT (IU/L) | 19 | Oct-40 |
| AST (IU/L) | 20 | Oct-40 |
| Bilirubin (total) (mg/dl) | 1.1 | |
| Bilirubin (direct) (mg/dl) | 0.79 | |
| Alkaline phosphatase (U/L) | 178 | |
| Renal function tests | ||
| Serum Cr (mg/dl) | 0.79 | |
| BUN (mg/dl) | 24 | Oct-20 |
| Other chemistry tests | ||
| Serum creatine kinase | 616 | 29-168 |
| TSH (µU/ml) | 12.54 | 0.5-4.7 |
| T4 (µg/dl) | 7.68 | 4.5-10.9 |
| T3 (ng/dl) | 59 | 60-181 |
| Uric acid (mg/dl) | 5.5 | 3.5-6.5 |
| Serum cholesterol (mg/dl) | 99.7 | < 200 |
| Fasting glucose (mg/dl) | 98 | 70-100 |
| Serum K+ (mmol/L) | 3.17 | 3.5-5.5 |
| Serum Na+ (mmol/L) | 134.2 | 130-145 |
| Serum Calcium (mmol/L) | 2.1 | 2.2-2.9 |
| Serological tests | ||
| ANA | Positive | |
| RF (IU/ml) | < 20 | 0-30 |
| HBsAG | Negative | - |
| Anti-HCV antibody | Negative | - |
| Anti-HIV antibody | Negative | - |
NB:ALT: Alanine Aminotransferase; ANA: Anti-Nuclear Antibody; AST: Aspartate Aminotransferase; BUN: Blood Urea Nitrogen; Cr: Creatinine; ESR: Erythrocyte Sedimentation Rate; HBSAg: Hepatitis-B Surface Antigen; RF: Rheumatoid Factor; TSH: Thyroid Stimulating Hormone; T4 : Thyroxine; T3 : Thriiodothyronine
Table 1. Laboratory profiles of the patient with overlap syndrome (sclerodermatomyositis) in University of Gondar hospital, Northwest Ethiopia.
Echocardiography (using simplified Bernoulli’s equation) suggested pulmonary arterial hypertension (Pulmonary arterial systolic pressure=45 mmhg (normal range,<40 mmhg), Abdominal ultrasonography suggested fatty liver. Pre-and post-contrast MRI of thigh muscles (T1 coronal, T2 sagittal, PDW sagittal and axial) revealed normal muscular signal intensity and no abnormal muscular enhancement. Upper gastrointestinal endoscopy showed dilated, erythematic and edematous distal esophagus with accumulated food remnants. The stomach and duodenum were normal. Muscle biopsy revealed muscle fiber atrophy with collagenous fibrosis. The diagnosis of sclerodermatomyositis was made based on the ACR-EULAR classification criteria for systemic sclerosis and dermatomyositis. She was started on prednisolone 0.5 mg/kg PO daily (25 mg PO daily), methotrexate 7.5 mg PO weekly, folic acid 5 mg PO daily, cotrimoxazole 960 mg PO three times weekly, nifedipine (XR) 60 mg PO daily, and omeprazole 20 mg PO twice daily. Mometasone body cream, liquid paraffin (moisturizer) and broad-spectrum sun screen (SPF-30) were applied on skin on daily basis. Physical therapy was initiated as per scheduled. The Patient was advised to dress warmly, to wear socks and gloves, and to avoid exposure to cold and direct sun light. She had shown significant improvement in muscle strength within three weeks of steroid therapy. So then, de-escalation regimen of corticosteroids was started. She was appointed to ‘Chronic Illness Clinics’ of the hospital for close follow up after three weeks of admission to the medical ward, University of Gondar hospital.
Discussion
Systemic Sclerosis (SSc) is an autoimmune disease with the hall mark features of fibrosis of the skin and/ or internal organs, autoantibodies and vasculopathy. It has two forms, limited cutaneous SSc, and diffuse cutaneous SSc. Skin sclerosis on the distal extremities, Raynaud’s phenomenon, calcinosis cutis and cutaneous telangiectasia are clinical features of limited cutaneous SSc. Diffuse cutaneous SSc presents with diffuse skin sclerosis with internal organ fibrosis, which causes interstitial pulmonary fibrosis, pulmonary arterial hypertension, esophageal hypomotility and scleroderma renal crisis [1-3]. The diagnosis of the patient was classified under ‘systemic sclerosis’ (score 17 points (>9 points)) as per ‘ACR-EULAR Classification Criteria for Systemic Sclerosis’ as evidenced by detection of skin thickening of both hands extending proximal to Metacarpophalangeal (MCP) joints, fingertip lesions (pitted digital scars), Raynaud’s phenomenon and pulmonary hypertension. Nail capillary pattern abnormalities and SSc-specific autoantibodies were not determined [4]. Dermatomyositis (DM) is an idiopathic inflammatory myopathy characterized by symmetric proximal muscle weakness with photosensitive, erythematous skin eruptions over the fingers, face, neck and trunk. Most patients usually have elevated skeletal muscle enzymes at the time of active myositis. Muscle biopsy findings of perimysial and/or perivascular inflammatory infiltrates with muscle fiber necrosis suggest inflammatory myopathy. Electromyography (EMG) is helpful in confirming myogenic changes [5- 7]. The diagnosis of the patient was classified under ‘definite’ idiopathic inflammatory myopathy (score 14.4 points (>8.7 points with biopsy)) as per ‘ACR-EULAR Classification Criteria for Idiopathic Inflammatory Myopathies’ as evidenced by a young woman who had progressive, symmetric, proximal muscle weakness of both upper and lower extremities, neck flexor weakness, guttron’s and helitrope rash, esophageal dysmotility, and elevated Creatine Kinase (CK) level [8]. In addition, ‘probable’ diagnosis of dermatomyositis was met using ‘Bohan and Peter’s diagnostic criteria for dermatomyositis’ as evidenced by the detection of symmetric proximal muscle weakness, elevated serum skeletal muscle enzyme and typical skin rash of DM [9]. The overlapped presence of SSc and DM in one patient settles the diagnosis of sclerodermatomyositis. Possible differential diagnoses include Mixed Connective Tissue Disease (MCTD) and Anti-Synthetase Syndrome (ASS). MCTD presents with combined features of Systemic Lupus Erythematosus (SLE), systemic sclerosis, Rheumatoid Arthritis (RA), dermatomyositis/ polymyositis, and a positive anti-U1-RNP antibody. The presence of Raynaud’s phenomenon, pulmonary hypertension, myopathy, esophageal dysmotility and scleroderma of the hands favors diagnosis of MCTD. Components of SLE or RA were not observed in our case. Anti-U1-RNP, serological marker for MCTD, was not done. Anti-synthetase syndrome is characterized by the presence of interstitial lung disease, myopathy, polyarthritis, Raynaud’s phenomenon, mechanic’s hands and positive anti-Jo-1 antibody. Interstitial lung disease and polyarthritis were not detected in our case. Anti- Jo-1 which is histidyl-tRNA synthetase antibody was not done. [10-12]. High dose systemic corticosteroid is the therapy of choice for dermatomyositis, but higher doses might precipitate undetected scleroderma renal crisis. So then, prednisolone 0.5 mg/kg PO daily was initiated. After disease control, dose of steroid would be de-escalated at 5 mg PO weekly, and would be maintained on low-dose steroid (10 mg PO daily). Methotrexate 7.5 mg PO weekly was started as steroid sparing immunosuppressant. In addition, she was started on dihydropyridine-type calcium-channel inhibitors for Raynaud’s phenomenon, and proton pump inhibitors for gastro-esophageal reflux disease. Topical steroids, broad-spectrum sun screens and moisturizers were used for dermatologic problems [13, 14]. She was scheduled for ‘Chronic Illness Clinic’ outpatient visits after discharge. In conclusion, the patient described had sclerodermatomyositis using ACR-EULAR Classification Criteria. The low expectations and diagnostic challenges of this rare disease in limited clinical settings might contribute to delayed diagnosis and treatment. High index of clinical suspicion is required to diagnose sclerodermatomyositis in resource-limited settings to prevent adverse outcome.
Acknowledgements
We are grateful to the medical personnel who were caring for the patient.
Funding
The authors received no financial support from any source.
Authors’ contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Ethical approval
Our institution does not require ethical approval for reporting individual case reports.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editorin- Chief of this journal.
Conflict of interest
The authors declare no potential conflict of interest with respect to the research, authorship or publication of the article.
References
- Varga J. Disorders of immune-mediated injury: Systemic sclerosis (scleroderma) and related disorders. In: Jameson JL, Fauci AS, Kasper DL, et al. 20th edn. Harrison’s principle of internal medicine. New York: McGraw-Hill, USA, 2546–2560 (2018).
- Varga J. Clinical manifestations and diagnosis of systemic sclerosis (scleroderma) in adults. Uptodate. (2021).
- Erzer JN, Jaeger VK, Tikly M et al. Systemic sclerosis in sub-Saharan Africa: a systematic review. Pan. Afric. Med. J. 37(176), (2020).
- Hoogen FVD, Khanna D, Fransen J et al. Classification criteria for systemic sclerosis: An ACR-EULAR collaboration initiative. Arthritis. Rheum. 65(11), 2737–2747 (2013).
- Greenberg SA, Amato AA. Disorders of immune-mediated injury: Inflammatory myopathies. In: Jameson JL, Fauci AS, Kasper DL et al. 20th edn. Harrison’s principle of internal medicine. New York: McGraw-Hill, USA, 2590–2596 (2018).
- Miller ML, Vleugels RA, Amato AA. Clinical manifestation of dermatomyositis and polymyositis in adults. (2020).
- Chinniah KJ, Mody GM. The spectrum of idiopathic inflammatory myopathies in South Africa. Clin. Rheum. 40, 1437–1446 (2021).
- Lundberg IE, Tjaralund A, Bottai M et al. 2017 EULAR/ACR classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Arthritis. Rheum. 69(12), 2271–2282 (2017)
- Bohan A, Peter JB, Diagnostic criteria for dermatomyositis. N. Engl. J. Med. 292, 344–347 (1975).
- Febyani M, Purbo HD, Hamijoyo L et al. Sclerodermatomyositis. Indon. J. Rheum. 3, 32–36 (2011).
- Toll A, Monfort J, Benito P et al. Sclerodermatomyositis associated with severe arthritis. Dermatol. Online. J. 10(2), 18–19 (2004).
- Ambade GR, Dhurat RS, Lade N et al. Childhood sclerodermatomyositis with generalized morphea. Indian. J. Dermatol. Venereol. Leprol. 74(2), 148–150 (2008).
- Kowal-bielecka O, Fransen J, Avouac J et al. Update of EULAR recommendations for treatment of systemic sclerosis. Ann. Rheum. Dis. 76, 1327–1339 (2017).
- Kohsaka H, Mimori T, Kanda T et al. Treatment consensus for management of polymyositis and dermatomyositis among rheumatologists, neurologists and dermatologists. Neurol. Clin. Neurosci. 7, 3–21 (2019).