Mini Review - Interventional Cardiology (2021) Volume 13, Issue 5
Distal cephalic vein access for right heart catheterization from the anatomical snuffbox
- Corresponding Author:
- Hady Lichaa
Ascension Saint Thomas Heart Rutherford Institution,
1840 Medical Center Parkway-Suite 201,
Murfreesboro,
TN 37129,
USA,
E-mail: Hady.lichaa@gmail.com
Received date: July 12, 2021 Accepted date: July 26, 2021 Published date: August 02, 2021
Abstract
Distal radial artery access for Left Heart Catheterization (LHC) from the anatomical snuffbox has become more prevalent in clinical practice due to its multiple well described advantages. If an associated Right Heart Catheterization (RHC) is required, it is usually performed from the antecubital area or distal medial arm access. This requires a dual procedural field preparation which adds more time, patient inconvenience, radiation exposure to the operator as well as suboptimal ergonomics.
We hereby present a new technique for right heart catheterization from a distal cephalic access. This novel approach offers many advantages: Patient comfort, ease of setup, operator convenience in access/ergonomics, reduction of radiation exposure and simultaneous arterial and venous hemostasis with the same distal radial compression device, allowing for improved efficiency and better patient throughput.
Keywords
Anatomical snuffbox • Right heart catheterization • Distal cephalic vein access • Distal radial artery access • Hemodynamic assessment
Introduction
This is a review of a novel technique involving the performance of a RHC from a distal cephalic vein access in the anatomical snuffbox [1].
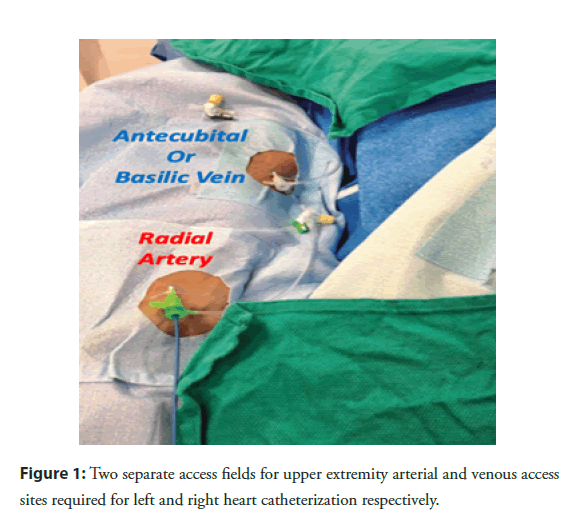
Radial artery access has clearly demonstrated its superiority over femoral access, with regards to cardiac catheterization procedural morbidity and mortality, in patients with acute myocardial infarction [2,3]. With the radial artery gaining popularity as a default access site for LHC in most parts of the world, some interventional cardiologists are nostalgic about the days when LHC and RHC can be performed from the same procedural field in the groin, rather than two separate fields in the arm [4] (Figure 1). Two separate fields in the upper extremity for arterial and venous access are not only inconvenient and non-ergonomic for the patient, staff and operator alike, but it leads to more radiation exposure to the operator and requires two separate hemostasis methods, which increase total procedural time and slows patient throughput in the catheterization laboratory (cath lab).
Literature Review
The need for an alternative venous access site in the upper extremity
One may ask: Why not access one of the satellite radial veins which course alongside the radial artery?
Well, these radial veins are often too small to accommodate a 5/6F sheath, even after application of a tourniquet around the distal forearm. To solve this problem, one would have to think “outside the box” with regards to alternative venous access sites. This can be safely achieved in the anatomical snuffbox.
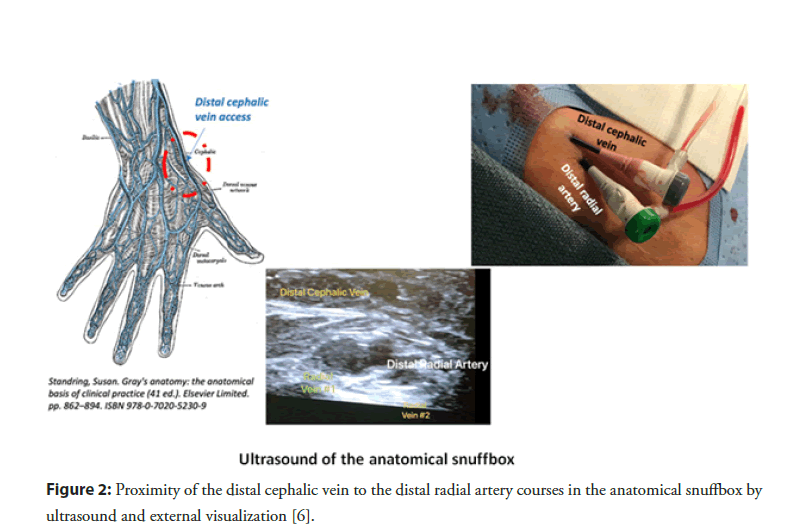
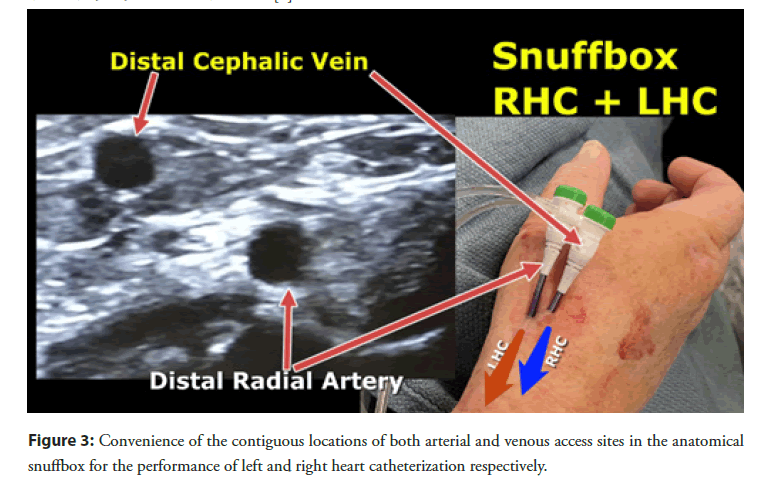
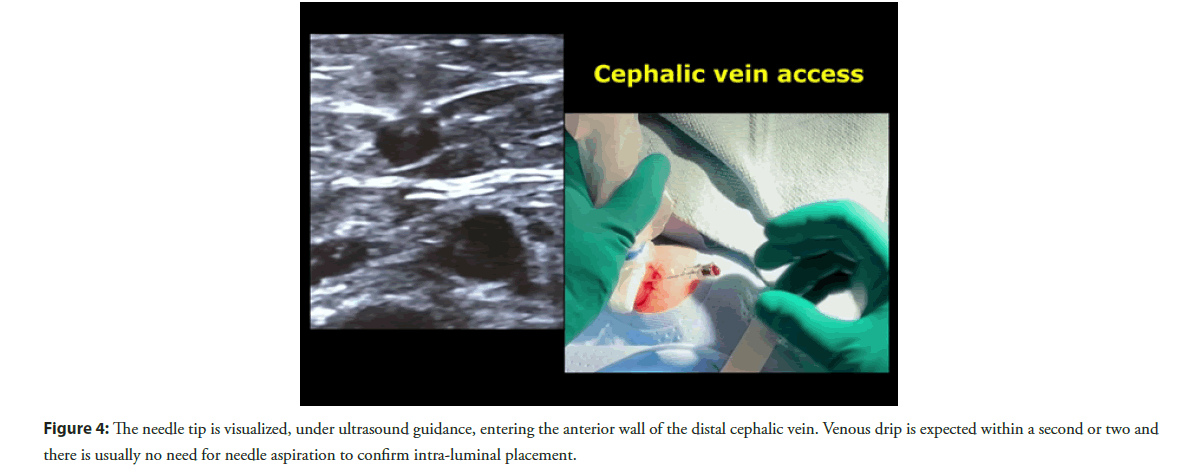
Distal radial artery access for Left Heart Catheterization (LHC) from the anatomical snuffbox has become more prevalent in clinical practice due to its multiple well described advantages [5]. The distal cephalic vein originates from the dorsal metacarpal veins of the hand and courses through the anatomical snuffbox, in the superficial fascia overlying the distal radial artery [6] (Figure 2). It often has a similar size as the distal radial artery and this can be significantly increased with a tourniquet placed under the drape at the distal forearm right before venous access (Figures 3 and 4). The compliance of venous wall allows it to handle sheath sizes from 5 to 6 French (F) depending on the size of the patient and the vein itself. One important advice is to avoid the usual aspiration and flushing of the sheath side port after insertion, because the vein often spasms at the tip of the sheath and negative aspiration will often cause air bubbles to appear, from suction through the sheath valve. If one would like to flush the sheath, it is advisable to open the sheath side port and let it passively bleed, then flushing the sheath with saline afterwards.
Figure 2: Proximity of the distal cephalic vein to the distal radial artery courses in the anatomical snuffbox by ultrasound and external visualization [6].
Advantages of distal cephalic vein access
RHC and LHC from the anatomical snuffbox allow for optimal patient comfort, since the hand is positioned in a neutral position alongside the patient’s body. This reinforces patient satisfaction even more than in traditional radial access, which requires abduction and external rotation of the arm (less comfortable for obese patients and associated with more radiation exposure to the operator).
This technique also allows for a more comfortable procedural setup for the cath lab staff. If the operator depends on the nursing staff in getting sterile intravenous access in the antecubital fossa ahead of the procedure, this eliminates this need, hence saving time and avoiding the complexity of removing the transparent adhesive dressing, in the middle of field of access, in a sterile fashion.
This distal cephalic vein approach to RHC is also a much more ergonomically friendly to the operator, who can manipulate and torque the catheter much more easily while standing straight, instead of leaning forward and reaching the medial aspect of the patient’s proximal arm.
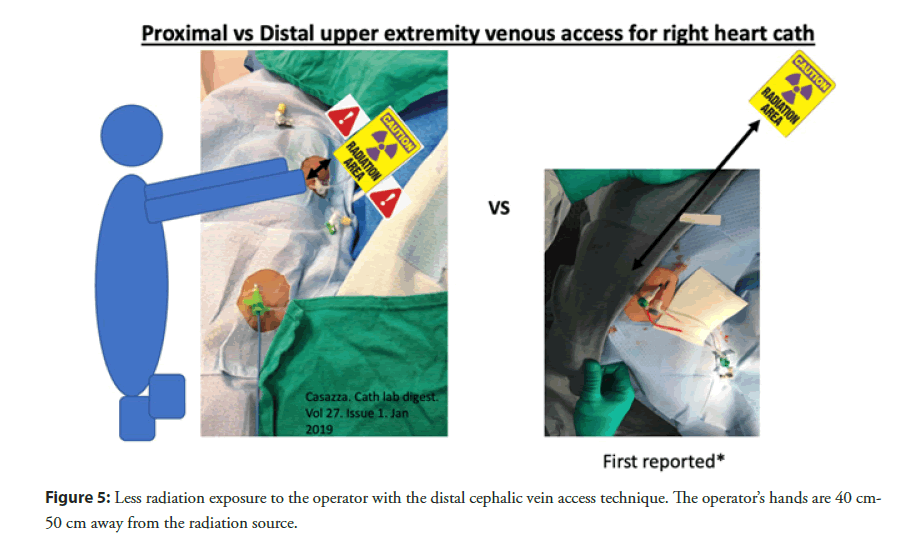
Additionally it results in a much lower radiation exposure to the operator since right heart catheter manipulation is performed further away from the radiation source (Figure 5). With traditional arm antecubital venous access for right heart catheterization, the operator’s hand is very close to the radiation source while advancing the right heart catheter. Conversely, with this new technique, the operator’s hand is at least 40 cm-50 cm further away from the fluoroscopy field which significantly reduces radiation exposure.
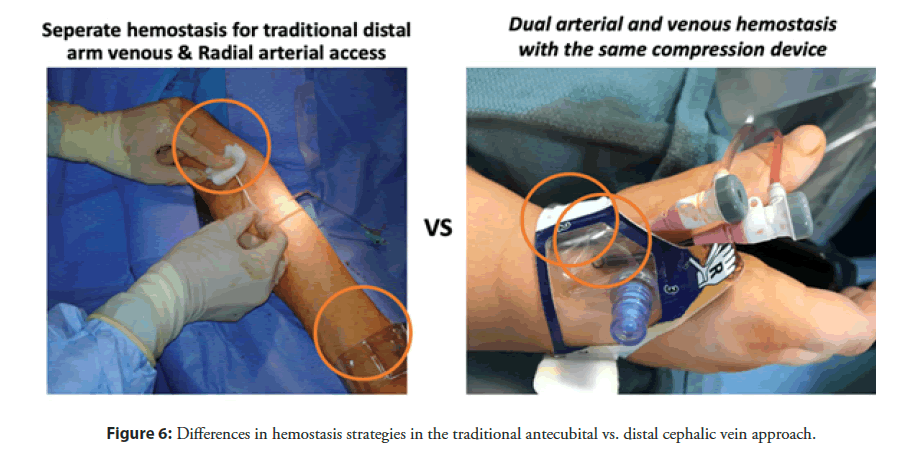
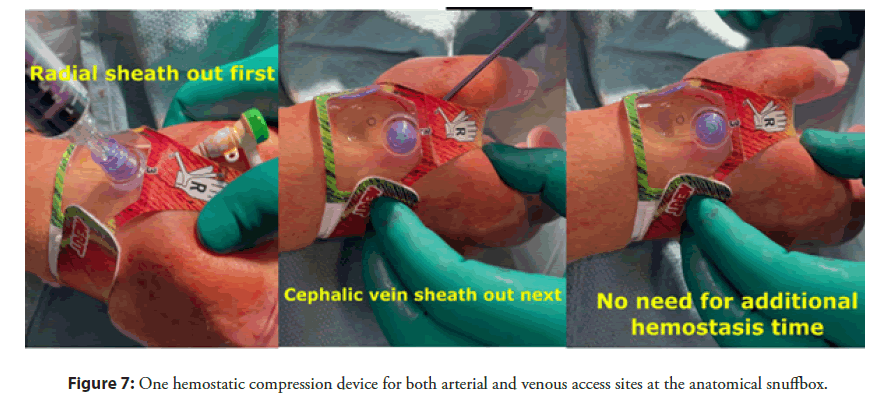
Another advantage lies in the use of one hemostatic compression device for both contiguous arterial and venous access sites, when compared to the traditional approach that requires additional manual hold time for venous hemostasis (Figures 6 and 7). After pulling the radial arterial sheath with the patent hemostasis technique, the venous sheath is pulled, without the need for additional compression. This saves precious time and allows for faster patient throughput in the cath lab, while increasing patient satisfaction. Patients love the minimally invasive approach of getting to both sides of their heart from the “back of the thumb”. They are frequently amazed by it.
Figure 6: Differences in hemostasis strategies in the traditional antecubital vs. distal cephalic vein approach.
Disadvantages of distal cephalic vein access
On the other hand, the major downside of this technique is the long distance to the pulmonary capillary wedge position which is often longer than the 110 cm catheters available on the market, in patient taller than 167 cm. As far as we know, there are no dedicated right heart catheters longer than 110 cm on the current market. Hence, patients taller than that are not good candidates for this technique unless 150 cm flexible peripheral 4F catheters (e.g. 4F angled Navicross catheter-Terumo) are used. The latter technique is performed over a supportive 0.014” wire (e.g. Grandslam [Asahi intec], Spartacore [Abbott Vascular], etc.) with a hemostatic Y valve connected to the back of the catheter, hence allowing for continuous pressure assessment while the catheter is advanced through the right chambers over the wire. Cardiac output can be estimated by the Fick method, however it does not allow for measurement of the cardiac output with the thermodilution method. We are hoping that industry starts manufacturing 170 cm balloon tipped catheters, which allow for the use of this technique in most patients.
Moreover, another disadvantage is the relatively small size of the distal cephalic vein at this anatomical location, which is significantly smaller than the distal arm basilic or brachial veins and smaller than the mid cephalic or antecubital veins. However, with the application of a tourniquet at the distal forearm, 5/6 or even 6/7F thin walled sheaths can be often placed without difficulty. Ultrasound examination prior to draping, while a distal forearm tourniquet is applied, is highly recommended. Identification of a very small venous size at this location before draping saves time and effort. It also allows selection of patients where this technique is not anatomically possible and for a quick change of vascular access strategy from the beginning of the case, hence improving procedural efficiency.
Care must be taken to avoid multiple venous punctures, since veins in this location quickly spasm and become inappropriate for further access attempts. The operator could use the modified Seldinger access technique with the bare needle used for radial access, however if one feels more comfortable with the combined “needle-in-IV” approach for the recommended shallow angle of venous entry, it is also considered reasonable.
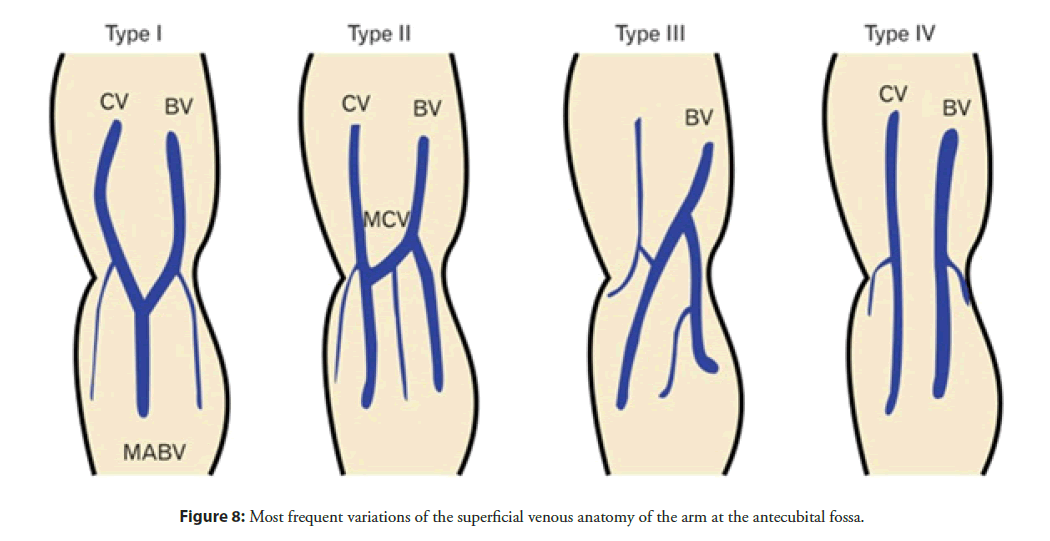
Finally, the sharp angle of the cephalic vein relative to the axillary vein and often the presence of a valve at that transition may require an 0.025˝ or 0.018˝ wire for crossing. However, there are four types of anatomical connections between the cephalic and basilic veins [7] (Figure 8), which allow for switching routes to the right heart chambers, by transitioning from the cephalic to the basilic vein, which has a more straightforward course to the heart. Usually, advancement of a bare right heart catheter under fluoroscopic guidance, of course without inflation of the tip balloon before reaching the shoulder, leads to the subclavian vein. If difficulties are encountered in the process, a “road mapped” cephalic venogram would be recommended from the access sheath, with 7 ml-8 ml of iodinated contrast. Clear and efficient venography is achieved with distal forearm manual compression, to augment and accelerate venous outflow.
Figure 8: Most frequent variations of the superficial venous anatomy of the arm at the antecubital fossa.
Technical tips and tricks
Fifteen practical tips and tricks for achieving success with this technique are presented in Table 1.
| Practical tips and tricks | |
|---|---|
| Tip 1 | Patient height <167 cm-Measure approximate right heart catheter course |
| Tip 2 | Mandatory ultrasound (US) with high frequency hockey stick probe (7 MHz) |
| Tip 3 | US before preparation and draping for planning of access strategy |
| Tip 4 | Patient hand in neutral position with slight ulnar deviation over a rolled towel under the wrist joint |
| Tip 5 | Very gentle pressure on US probe to minimize venous collapse |
| Tip 6 | Venous before arterial access |
| Tip 7 | 20-30 degree angle of venous needle entry |
| Tip 8 | Slow alternating needle movements to improve visualization of needle tip under US |
| Tip 9 | At blood return, wire needle without removing US probe |
| Tip 10 | If unsuccessful, try more proximal post subcutaneous nitroglycerin |
| Tip 11 | Venous sheath access size 1-2F larger than intended right heart catheter used to accommodate the most proximal thick portion of the catheter |
| Tip 12 | Braided thin walled sheath |
| Tip 13 | No aspiration from sheath side port |
| Tip 14 | If PCWP cannot be reached go sheathless which adds a 7 cm reach (thick portion of the proximal catheter) |
| Tip 15 | Alternatively use 150 cm 4F peripheral soft catheter over the wire |
Table 1: Fifteen practical tips and tricks.
Conclusion
This novel technique, consisting of performing a RHC from a distal cephalic vein access, right next to the distal radial artery which serves as an access for LHC, is a safe, comfortable, convenient and ergonomic approach with potential for less radiation exposure and faster patient throughput. In other words it is a winning situation for the patient, cath lab staff and operator alike.
References
- Lichaa H. Right heart catheterization: Right from the anatomical snuffbox. J Invasive Cardiol. 32(9): E233-E237 (2020).
- Andò G, Capodanno D. Radial access reduces mortality in patients with acute coronary syndromes: Results from an updated trial sequential analysis of randomized trials. JACC Cardiovasc Interv. 9(7): 660-70 (2016).
- Valgimigli M, Frigoli E, Leonardi S, et al. Radial versus femoral access and bivalirudin versus unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): Final 1-year results of a multicentre, randomised controlled trial. Lancet. 392(10150): 835-848 (2018).
- Seto A. Ultrasound guidance for upper extremity arterial and venous access. Cath lab digest. 23(12): (2015).
- Coomes EA, Haghbayan H, Cheema AN. Distal transradial access for cardiac catheterization: A systematic scoping review. Catheter Cardiovasc Interv. 96(7): 1381-1389 (2019).
- Susan S. Gray's anatomy: The anatomical basis of clinical practice (41 ed.) pp. 862-894 (2020).
- Lee H, Lee SH, Kim SJ, et al. 2015 Variations of the cubital superficial vein investigated by using the intravenous illuminator. Anat Cell Biol. 48(1): 62-5 (2015).