Case Report - Interventional Cardiology (2024)
Double chronic total occlusion of left ascending artery proximally and right coronary artery
- Corresponding Author:
- Abdelaziz Ahmed Abdelaziz
Department of Cardiology, Al- Azhar University, Cairo, Egypt,
E-mail: abdelaziz_1975@yahoo.com
Received date: 30-Aug-2024, Manuscript No. FMIC-24-146870; Editor assigned: 02-Sep-2024, PreQC No. FMIC-24-146870 (PQ); Reviewed date: 16-Sep-2024, QC No. FMIC-24-146870; Revised date: 23-Sep-2024, Manuscript No. FMIC-24-146870 (R); Published date: 02-Oct-2024, ![]()
Abstract
Introduction: Percutaneous Coronary Intervention (PCI) for Chronic Total Coronary Occlusions (CTOs) is a highly demanding treatment in interventional cardiology and carries a higher risk of major consequences. The operation becomes significantly more challenging with two-vessel occlusion.
Patient concerns: A male patient 53 yrs old, suffered from non-insulin-dependent Diabetes Mellitus (DM), Hypertension (HTN), dyslipidemia and had typical chest pain for the last three months on minimal exertion. The Electrocardiogram (ECG) showed ST elevation and Q wave from VI-V5 and Q wave in lead III and a vessel failure. His echocardiography revealed impaired function with Ejection Fraction (EF) 46% and regional wall motion abnormality in the Left Anterior Descending (LAD) and the Right Coronary Artery (RCA).
Diagnoses: The coronary angiography results revealed the CTO of the LAD proximally and the CTO of the RCA shortly after its ostium.
Interventions: PCI to LAD and RCA were done using implantation of 2 Drug-Eluting Stents (DES) in LAD and one DES in RCA.
Outcomes: Successful PCI to LAD and RCA using 3 DES.
Conclusion: Successful PCI to CTO LAD and RCA with implantation of 3 DES.
Keywords
Chronic total occlusion • Left anterior descending • Percutaneous coronary intervention • Right coronary artery • Heart apex • Stenting
Abbreviations
DES: Drug-Eluting Stent; ECG: Electrocardiogram; HTN: Hypertension; LAD: Left Anterior Descending Artery; CTO: Chronic Total Occlusion; RCA: Right Coronary Artery; PCI: Percutaneous Coronary Intervention
Introduction
Coronary Chronic Total Occlusions (CTOs) are seen in around one-third of individuals who have diagnostic coronary angiography and the prevalence of CTOs tends to increase with age. CTOs remain the most complex form of lesion that interventional cardiologists face. The benefits of a successful CTO recanalization treatment include improved chances of survival, especially in patients with a significant ischemia burden (>10%). Additionally, it results in enhancements in anginal symptoms and left ventricular function, decreases the necessity for Coronary Artery Bypass Grafting (CABG) surgery and augments exercise tolerance. Nevertheless, fewer than 10% of all CTOs have undergone percutaneous operations for an extended duration of time [1].
The retrograde technique for PCI in CTO was established in 2005 and brought about a significant transformation in the field of CTO recanalization. However, based on the existing data, the rates of PCI for CTOs are as low as 10%-15%. Additionally, the majority of these patients receive medical therapy or undergo CABG [2].
In this report, we describe a patient who had a significant amount of ischemic tissue damage and two coronary arteries, the Left Anterior Descending (LAD) artery and the Right Coronary Artery (RCA), that were completely blocked for a long period of time. However, both arteries were effectively treated during a single medical procedure.
Case Presentation
An Egyptian patient, aged 59, was hospitalized to the cardiology department at Teachers Hospital due to experiencing chest pain with minimal physical activity. The patient had other comorbidities, namely hypertension, non-insulin-dependent diabetes mellitus and dyslipidemia. The diagnosis of the case was verified using the ECG, which showed ST elevation and Q wave from VI to V5, as well as a Q wave in lead III and aVF. The echocardiogram results showed reduced function with an ejection fraction of 46% and aberrant movement of the heart wall in the areas supplied by the LAD and RCA.
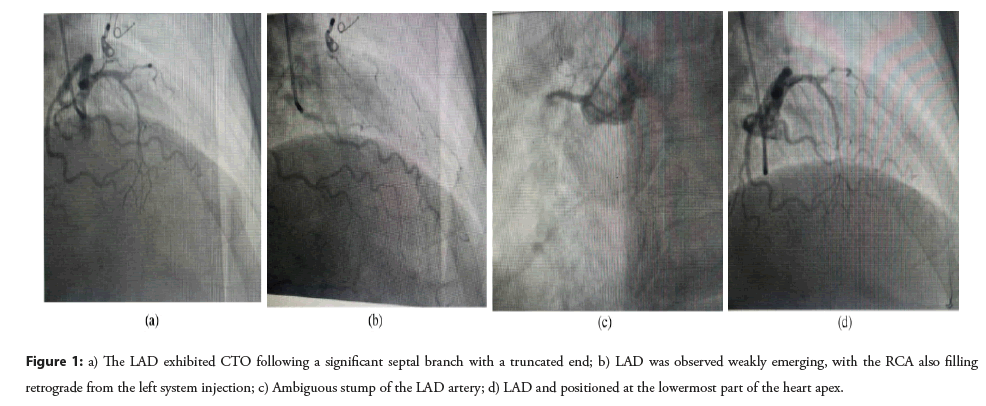
The coronary angiography was performed utilizing a trans-radial method, which showed that the LM artery had a moderate size and divided into the LAD and Left Circumflex (LCX) arteries. The LAD exhibited CTO following a significant septal branch with a truncated end (Figure 1a). After a sufficient period of time for the dye to be carried away in the same RAO projection image, the distal LAD was observed weakly emerging, with the RCA also filling retrograde from the left system injection (Figure 1b).
Figure 1: a) The LAD exhibited CTO following a significant septal branch with a truncated end; b) LAD was observed weakly emerging, with the RCA also filling retrograde from the left system injection; c) Ambiguous stump of the LAD artery; d) LAD and positioned at the lowermost part of the heart apex.
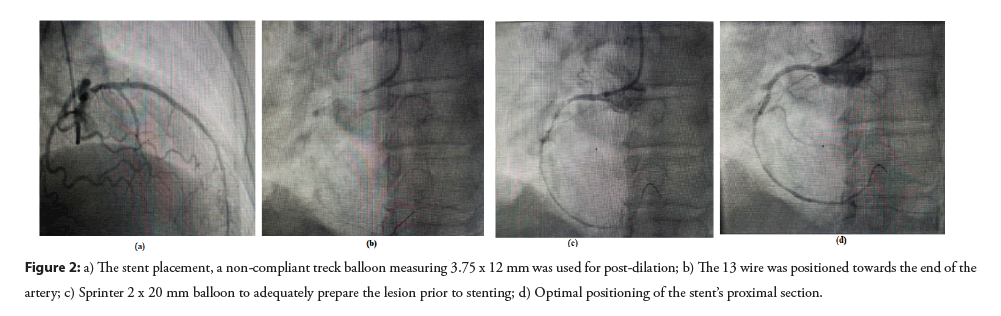
The LM was activated using the XB3 6F guiding catheter. The CTO of the LAD artery was addressed using a PT2 MS wire, aided by a Maverick 1.5 x 15 mm balloon. This was done to accurately guide the wire tip into the LAD artery and away from the nearby septal and diagonal branches, which were located at the ambiguous stump of the LAD artery (Figure 1c). The PT2 wire was effectively threaded through the blocked LAD and positioned at the lowermost part of the heart apex (Figure 1d). Multiple Percutaneous Transluminal Coronary Angioplasty (PTCA) procedures were performed utilizing a Maverick 1.5 x 15 mm balloon and another Sprinter 2 x 20 mm balloon to adequately prepare the lesion prior to stenting and accurately evaluate the stent size. Subsequently, two Drug-Eluting Stents (DES) were inserted, specifically the Xience Alpine stents measuring 2.75 x 38 mm and 3 x 38 mm. These stents were placed in a way that they overlapped each other. Following the stent placement, a noncompliant treck balloon measuring 3.75 x 12 mm was used for post-dilation (Figure 2a).
Figure 2: a) The stent placement, a non-compliant treck balloon measuring 3.75 x 12 mm was used for post-dilation; b) The 13 wire was positioned towards the end of the artery; c) Sprinter 2 x 20 mm balloon to adequately prepare the lesion prior to stenting; d) Optimal positioning of the stent’s proximal section.
The RCA was utilized with the same XB3 6F guiding catheter. The entire blockage of the RCA was successfully crossed using a PT2 MS wire, aided by a Maverick 1.5 x 15 mm balloon. The 13 wire was positioned towards the end of the artery (Figure 2b). Following the successful crossing of the wire to the lesion, numerous Percutaneous Transluminal Coronary Angioplasty (PTCA) procedures were performed utilizing a Maverick 1.5 x 15 mm balloon and another Sprinter 2 x 20 mm balloon to adequately prepare the lesion prior to stenting (Figure 2c). Next, the Xience Alpine stent with dimensions of 2.5 x 38 mm was inserted at the location of complete blockage and expanded using an NC force balloon measuring 3.25 x 20 mm to ensure optimal positioning of the stent’s proximal section (Figure 2d). Ultimately, the duration of fluoroscopy was around 50 minutes and the patient departed the catheterization laboratory with TIMI III flow and without any problems.
Results and Discussion
Chronic Total Occlusive (CTO) lesions are characterized by a significant buildup of atherosclerotic plaque, an unpredictable path of the blood flow where the blockage occurs and extended segments of blockage inside the artery. As a result, the rate of success in revascularization is reduced compared to non-CTOs [3].
CTOs present the greatest complexity and difficulty in managing them by percutaneous revascularization. Previous studies have found procedural success rates ranging from 58.9% to 75.2% [4,5]. Recently, the success rate of CTO-PCI has surpassed 80%, thanks to the utilization of innovative and advanced approaches, as well as the creation of specific devices [6,7]. The occurrence of several CTOs is less common compared to having only one CTO and the outcome with conservative therapy is worse. Generally, surgical intervention is a preferred option for these patients. Successful PCI of CTOs is associated with enhanced survival and the attainment of complete revascularization, which serves as a reliable indicator of survival. However, there is a lack of comprehensive evidence on the percutaneous revascularization of numerous CTOs [8].
The case involved a patient who had a reduced ability of the left ventricle to pump blood, with an EF% of 46%. The patient also had aberrant movement of the heart wall in the areas supplied by the LAD and RCA. A trans-radial route was used to perform coronary angiography, which revealed CTO in the LAD after a significant septal branch, as well as another CTO in the RCA. PCI was performed to revascularize the LAD and RCA. The intervention entailed the effective positioning of three DESS; two in the LAD and one in the RCA. The treatment was successfully executed without any difficulties, resulting in the patient attaining TIMI III flow.
The initial iteration of DES showed advancements in clinical and angiographic outcomes. However, there were apprehensions over long-term results due to elevated rates of stent thrombosis as compared to BMS, as well as mechanical problems including stent fractures. A new study 2 assessing the long-term safety and efficacy of DES in CTO lesions found that DES outperformed BMS in lowering Major Adverse Cardiac Events (MACES), TLR and TVF over a five-year period [9].
Between 10% and 20% of CTO-PCI failures can be attributed to balloon uncrossable lesions. Approaches to address such issues begin with straightforward technical suggestions, such as enhancing guide catheter support and employing deep seating or buddy wire techniques. While femoral access is generally preferred for CTO-PCI, there have been isolated studies highlighting the potential benefits of a radical approach. However, it is important to note that in the current patient, this radial approach may not offer adequate backup support [10].
A previous report presented by Konstantinidis and Sianos [11]. This report describes a case where a CTO recanalization surgery was successfully performed on a young patient who had two coronary arteries that were persistently blocked and a significant amount of ischemic damage. Both CTOs were discussed at the same sSession using various specialized procedures to reopen the blocked blood vessels, while ensuring that safety concerns regarding the use of contrast dye and exposure to radiation were not overlooked. A new DES containing a biodegradable polymer was utilized for the treatment of the lesions.
However, a previous study by Rathore et al., reported that CTOPCI success rates are generally lower in cases of multivessel illness with a thrombus burden larger than 15 mm [12].
Successful revascularization was achieved with the utilization of primary PCI procedures and DES, resulting in notable clinical improvement. The patient’s successful procedure highlights the potential of PCI in efficiently treating complicated coronary artery disease, providing a less intrusive alternative to surgical procedures such as CABG.
Conclusion
The feasibility and clinical efficacy of PCI in managing complex CTOs in both the LAD and RCA were achieved through the implantation of three DES. Distal LAD and RCA filling in CTO cases plays an important role in predicting success of PCI whether ante-or-retro grade filling. Despite the complexity of treating two-vessel CTOs, the patient achieved excellent results without complications, highlighting the effectiveness of advanced PCI techniques in managing complex coronary artery disease.
References
- Khadtare A, Makhale C, Hiremath S, et al. Characteristics of patients undergoing percutaneous coronary intervention for chronically total occluded arteries: A single-center observational study in India. Cardiol Plus. 9(2):157-161 (2024).
[CrossRef] [Google Scholar] [PubMed]
- Ogaili A, Brilakis ES. To go retrograde or not? CC score to the rescue. Am J Card. 211:369-371 (2024).
[CrossRef] [Google Scholar] [PubMed]
- Baykan AO, Gür M, Acele A, et al. Predictors of successful percutaneous coronary intervention in chronic total coronary occlusions. Postepy Kardiol Interwencyjnej. 12(1):17-24 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Gong X, Zhou L, Ding X, et al. The impact of successful chronic total occlusion percutaneous coronary intervention on long-term clinical outcomes in real world. BMC Cardiovasc Disord. 21(1):1-9 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Hamzaraj K, Kammerlander A, Gyöngyösi M, et al. Patient selection and clinical indication for chronic total occlusion revascularization-a workflow focusing on non-invasive cardiac imaging. Life (Basel). 13(1):15-26 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Ybarra LF, Cantarelli MJ, Lemke VM, et al. Percutaneous coronary intervention in chronic total occlusion. Arq Bras Cardiol. 110(5):476-483 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Wemer GS, Brilakis ES. Chronic total coronary occlusion. Interv Cardiol J. (2022).
- Olivari Z, Rubartelli P, Piscione F, et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: Data from a multicenter, prospective, observational study (TOAST-GISE). J Am Coll Cardiol. 41(10):1672-1678 (2003).
[CrossRef] [Google Scholar] [PubMed]
- Colmenarez HJ, Escaned J, Fernández C, et al. Efficacy and safety of drug-eluting stents in chronic total coronary occlusion recanalization: A systematic review and meta-analysis. J Am Coll Cardiol. 55(17):1854-1866 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Wu CJ, Fang HY, Cheng CI, et al. The safety and feasibility of bilateral radial approach in chronic total occlusion percutaneous coronary intervention. Int Heart J. 52(3):131-138 (2011).
[CrossRef] [Google Scholar] [PubMed]
- Konstantinidis NV, Sianos G. Double chronic total occlusion recanalisation with antegrade and retrograde techniques and the use of a novel drug-eluting stent with biodegradable polymer. Interv Cardiol. 8(1):46-49 (2013).
[CrossRef] [Google Scholar] [PubMed]
- Rathore S, Matsuo H, Terashima M, et al. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: Impact of novel guidewire techniques. JACC Cardiovasc Interv. 2(6):489-497 (2009).
[CrossRef] [Google Scholar] [PubMed]