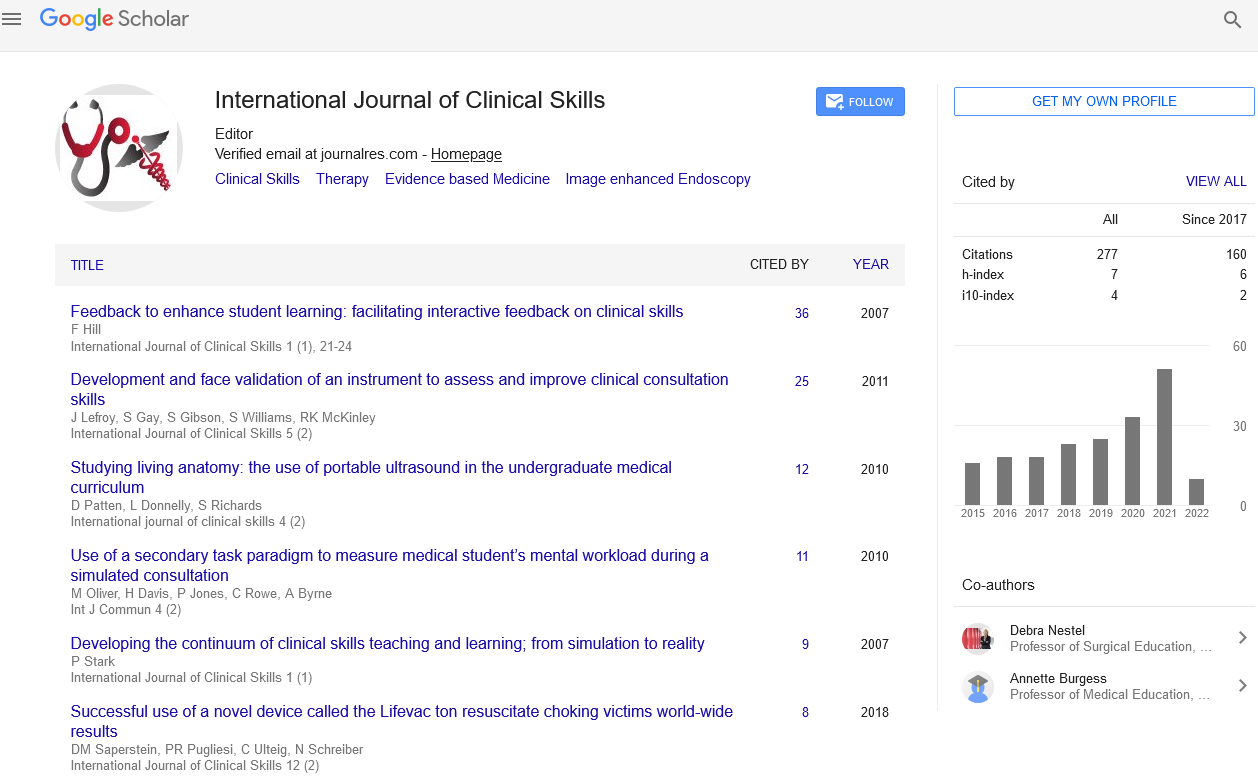
Review Article - International Journal of Clinical Skills (2017) Volume 11, Issue 3
Drug-Resistant Tuberculosis and Modern Approaches towards its Diagnosis
- Corresponding Author:
- Kuliya Skak
Department of Tuberculosis
Karaganda State Medical University
Karaganda, Kazakhstan (USSR)
Tel: +7 7775403637
E-mail: skak.kuliya@yandex.ru
Abstract
The review of the literature has shown that tuberculosis as a socially conditioned disease remains a serious problem in Kazakhstan and worldwide in general, currently taking the first position among the infectious diseases causing mortality. One of the main reasons of poor effectiveness of treatment and heavy mortality caused by tuberculosis is prevalence of multiple resistance of tuberculosis mycobacteria to antituberculotics. Modern immunological and molecular genetic tuberculosis diagnostic methods, in comparison with the traditional methods, are more sensitive and specific and allow within a short time detecting the presence of tuberculosis mycobacteria in bio-substrates and their resistance to drugs, which reduces the time of abacillation among the patients, increases effectiveness of the treatment, prevents prevalence of drug-resistant strains of tuberculosis mycobacteria, should allow decreasing the tuberculosis infection rate in general and incidence of Multiple/Extensive Drug-Resistant tuberculosis in particular.
Keywords
Multiple drug resistance, Extensive drug resistance, Bacteriological method, Xpertmtb/RIF, BACTEC, Hain test
Introduction
Tuberculosis (TB) is currently the second significant factor of mortality caused by an infectious agent after HIV/AIDS. According to a report of the World Health Organization in 2010, 8.8 million people fell ill with TB and 1.4 million people died from this disease. According to the authors’ data more than 95% of the TB mortality cases take place in the countries with low and middle income level, and this disease is one of the three main mortality causes among females aged from 15 to 44. In this regard, tuberculosis continues to invade the humanity taking away more human lives than any other disease. Over the last years the situation has been worsened by the global economic stagnation. According to the forecasts, tuberculosis will remain one of the ten gravest diseases in the world up to 2020 [1,2].
Over the last 15 years the global problem of Multiple Drug-Resistant TB has reached the focus of scientists especially in the countries of Eastern Europe and CIS, where high antituberculotic drug-resistant rate is observed. Economic, political and social problems in the late 21st century led to the changes in the healthcare system and its insufficient financing which had an effect on the health of population including the tuberculosis morbidity [3].
The World Health Organization (WHO) annually registers half a million of the new Multiple Drug-Resistant TB cases. Drugresistant tuberculosis is characterized by high mortality rates, complexity of treatment and high treatment expenses. A form of Multiple Drug-Resistant tuberculosis is Extensive Drug- Resistant TB, when a patient with Multiple Drug-Resistant TB has resistance to the most effective second-line antituberculotics (at least, to one of fluroquinolones and an injection drug) [4-6].
On 13th October 2016, the WHO released the Global Tuberculosis Report-2015 with frightening statistics. In 2015 the mortality caused by tuberculosis increased to 1.8 mln in comparison with 1.5 mln in 2014. According to the report, 41% of the diseased are not provided with diagnostics and treatment. There is still low guaranty of ensuring treatment for the people fell ill with drug-resistant tuberculosis, and in 2015 only 20% of such patients were provided with proper treatment [7].
In the world TB is one of the 10 leading mortality causes. In 2015, 10.4 millions of people fell ill with tuberculosis and 1.8 million people (including 0.4 million people with HIV) died from this disease. More than 95% of the TB mortality cases take place in the countries with low and middle income level. In 2015 in the world according to the data analysis 4,80,000 people developed Multiple Drug-Resistant TB. In different countries the incidence of Multiple Drug-Resistant tuberculosis varies over a wide range: in the USA – 3.5%, France – 0.5%, England and Wells – 0.6%, Switzerland – 1.7%, Italy – 2.5%. It is found that the incidence among those who come from the countries with high tuberculosis prevalence it is higher in comparison with the residents [8].
The WHO reports that in the countries of Central Asia the highest level of tuberculosis morbidity is observed, and judging by the number of new Multiple Drug-Resistant TB cases the republics of Central Asia take the leading positions in the world. The Central Asian countries enter the top five among the countries of Europe by the number of people with tuberculosis. Kazakhstan takes the third position in this list with the number of 139 patients per 1,00,000 residents. On the average, in Europe and Central Asia the morbidity is equal to 39 cases per 100 000 people. Out of 133 only 34 states taking part in the regional survey of the WHO in the period of 2013 and 2014 have a complete national plan and the strategy of solving the problem of resistance to antibiotics and other antimicrobial drugs [9].
Among the new and recurrent cases of active form of tuberculosis, the proportion is the following: in Bulgaria – 2.0 and 24%, Armenia – 9.4 and 43%, Georgia – 9.5 and 31%, Latvia - 10 and 24%, Lithuania - 11 and 52%, Kyrgyzstan - 14 and 39%, Kazakhstan - 14 and 45%, Uzbekistan - 14 - 49%, Ukraine - 16 and 44%, Estonia - 18 and 44%, the Russian Federation - 18 and 46%, Moldova - 19 and 65%, Azerbaijan - 22 and 56% and Tadjikistan - 17 and 62% respectively (according to the data of the WHO over the period of 2010-2011) [10-14].
According to the forecasts of the WHO in between 2011 and 2015 more than 2 million new cases of Multiple Drug-Resistant TB will be diagnosed. On present showing, annually in the world about 450 000 new cases of Multiple Drug-Resistant TB are diagnosed, provided that over 50% of all the cases are accounted for such countries as China, India and Russia. In the majority of the world countries in 2011 less than 5% of new and previously treated patients with tuberculosis were tested for Multiple Drug- Resistant TB and only 20% of the registered patients obtained proper therapy [12-14].
The existing cause of high rates of Multiple Drug-Resistant TB prevalence in Kazakhstan is insufficient observance of infection control measures in TB dispensaries, where all the patients: people with new diagnosed TB, recurrent disease with preserved sensitivity and people with probable drug-resistant TB are kept together until the drug susceptibility testing (DST) results are obtained. The DST results of a patient of the TB dispensaries are usually obtained in 2-3 months [15-17].
The therapy of the mycobacteria tuberculosisа (МТ) drug-resistant patients is much more expensive than treatment of the MT discharging patients sensitive to the main chemotherapeutics. The necessity to wait for the DST results leads to postponing proper chemotherapeutics and consequently causes the increase in expenses for antituberculotics [18].
The MT drug resistance is a significant factor limiting the effectiveness of tuberculosis chemotherapeutics (CHT) and by its nature is a peculiarity of the MT to adapt to any conditions of external environment, including developing resistance to antituberculotics [19].
In the current conditions the number of Multiple Drug-Resistant TB cases is on the rise. Drug resistance is an important indicator showing the gaps in the implementation of the National antituberculosis programs. There are microbiological, clinical and programconditioned prerequisites of the MT drug resistance development, though the main cause of development of this phenomena is the human factor [20].
Migration processes in Kazakhstan as well as constant increase in the number of people of the high-risk group including those with TB/ HIV and IDU, alcoholics, in and out-migrants, low-income individuals, prisoners and people released from imprisonment worsen the TB epidemiologic situation.
The increase in the drug-resistant TB cases, particularly Multiple Drug-Resistant TB is currently observed all over the world. Drug resistance has a negative impact not only on the treatment results, but also increases the expenses for the treatment of these tuberculosis forms, particularly when there is resistance to two main the most effective antibiotics (isoniazid and rifampin). Drug resistance is an important indicator showing the gaps in the implementation of the National antituberculosis programs.
Materials and Methods
There are several methods for defining drug resistance of mycobacteria, and the method of limit concentration is the most widespread in Kazakhstan. The principle of the method is measured inoculation of the mycobacterial suspension into the tubes with Lowenstein Jensen medium, containing antituberculotics in limit concentration, and into the tubes without antibiotics. The results are estimated in 21 days after the inoculation by the presence of growth of the mycobacteria in the media containing antituberculotics. The culture is deemed to be sensitive if the number of MTB colonies grown in the tube with the antibiotics does not exceed 20 and provided heavy growth in the control tube. If there are 20 and more colonies in the tube with the chemical and heavy growth in the control tube, the culture is considered to be resistant.
An alternative way of definition of the MTB drug resistance is detection of micro colonies in the thin layer agar.
The test is simple and does not require expensive consumable materials and complicated equipment; the average time for obtaining the result is 13 days. Besides, the method allows both indirect and direct definition of drug resistance immediately in sputum which is undoubtedly its advantage. The test showed good diagnostic characteristics and high convergence with the results of traditional methods [21,22].
The brand new level of tuberculosis bacteriological diagnostics has been achieved by the practical application of automated systems of broth cultivation BACTEC MGIT 960 (“Becton Dickinson”) and MB/BacT (“Organon Teknika”) for accelerated detection of mycobacteria, which allow detecting the growth of the culture in the diagnostic material in 10-20 days [23,24].
Results and Discussion
Automated system BACTEC MGIT 960 proved itself to be a reliable method of tuberculosis bacteriological diagnostics both throughput the world and in many regions of Russia [23-30].
According to the authors’ data, sensitivity of the ВАСТЕС MGIT 960 automated system in detection of the MTB cultures appeared to be by 10% higher than the traditional way of inoculation into the Lowenstein Jensen medium (LJ). The BACTEC MGIT 960 system also showed higher isolation rate of MT from bacterioscopically negative material, by about 15% in comparison with solid media. For bacterioscopically positive material sensitivity of liquid and solid media for cultivation appeared to be identical [24].
According to the data of foreign researchers, they managed to achieve by about 2.2-4% more MT isolates in the ВАСТЕС MGIT 960 automated system, than in solid LJ medium [28,30]. Application of BACTEC MGIT 960 type bacteriological systems allowed reducing the time of MT culture picking. In average, the period of cultivation of a sample through ВАСТЕС MGIT 960 was equal to 11-15, in solid medium 20-28 days [26,30,31].
BACTEC MGIT 960 automated system allowed investigating the picked cultures of mycobacteria tuberculosis for sensitivity to first-line antituberculotics, including to pyrazinamide, in a relatively short period of time in average in 2 weeks [23,27,31]. The traditional method for defining drug susceptibility to main antituberculotics is the method of limit concentrations in LJ solid medium [32]. The BACTEC MGIT-960 system showed significant convergence of results of the MT drug susceptibility testing with those obtained by the method of limit concentration. For rifampin and isoniazid the convergence of the data about presence of sensitive or resistant MTB forms was equal to 98.5 and 98.25% respectively, for streptomycin-97.26, for ethambutol–93.77%. Therewith the terms for obtaining the results of drug susceptibility in the BACTEC MGIT 960 automated system were from 4 to 13, while through the method of limit concentrations they were from 21 to 26 days, which is very important for timely and right choice of the antituberculotic therapy scheme [24,33].
The necessity of antituberculotic measures improvement with the application of innovative technologies of prevention, diagnostics and treatment of tuberculosis, recommended by the WHO, is also in the focus of the ‘Complete Anti-Tuberculosis Plan for the period of 2014-2020, approved in September 2013 [34]. Solution of these problems has not only medical but also economic significance. The complete plan provides conduction of scientific researches of the methods of effective tuberculosis diagnostics among children and adolescents (Diaskin-test, Quantiferon test), further introduction of XpertMTB/ RIF, BACTEC, Hain test into the laboratory service of TB dispensaries.
Immunological and molecular genetic methods are currently widely applied. The necessity of application of some or other diagnostic methods is provoked by the epidemic situation in the region. As recommended by the WHO and according to the data of various researches, in the regions with low level of morbidity it is more reasonable to use immunological tests which allow detecting latent infection, while in the regions with high level of morbidity- molecular genetic as well as bacteriological methods of defining MT and Multiple/Extensive Drug- Resistant МТ [35].
A molecular genetic method of MTB detection in sputum is Genexpert MTB/RIF, simultaneously ensuring quick diagnostics of tuberculosis and resistance to rifampin (Rif). Genexpert MTB/ RIF uses the method of semi-quantitative hilldrop polymerase chain reaction (PCR) in real time carried out in vitro. The Genexpert MTB/ RIF system is approved by the WHO and is recommended for application in all countries of the world as a screening test for detecting tuberculosis [36].
Development of Xpert MTB/RIF analysis for the GeneXpert platform was completed in 2009. This event is considered as a real breakthrough in the fight against TB. For the first time the molecular test became simple and reliable enough for its application beyond the raditional laboratory conditions. Xpert MTB/ RIF detects mycobacteria tuberculosis, as well as the mutations pointing at the resistance to rifampin using three special primers and five unique molecular probes for ensuring high degree of specificity. The analysis provides the result at direct manipulations with sputum less than in two hours. Notably, the GeneXpert platform and the Xpert MTB/RIF analysis are currently the only tested technology representing the new generation of automated platforms for molecular diagnostics. Хpert MTB/RIF detects mycobacteria tuberculosis, as well as the mutations pointing at the resistance to rifampin using three special primers and five unique molecular probes for ensuring high degree of specificity. There is no cross-reactivity with non-tuberculosis mycobacteria (NTM), that’s why MT and resistance to antibiotics are detected correctly, even with the presence of НТМ. The test specificity is equal to 99%. The sensitivity is up to 90% at testing of three samples. The result at direct manipulations with sputum is provided less than in two hours. DNA purification and amplification is carried out in a cartridge, preprocessing of diagnostic material is reduced to minimal manipulations. The possibility of contamination drastically decreases. It does not require zoning of the rooms. Хpert MTB/RIF is recommended to be used as the initial diagnostic test among the people with the assumption of Multiple Drug-Resistant TB or HIV-associated TB [35,37-41].
The Hain MTBDR plus genetic test system [35,37,38,40,41] is used for simultaneous detection of resistance to isoniazid and rifampin. The method is based on detection of the most frequent mutations in genes associated with resistance to isoniazid and rifampin, with the use of reversed ISH of amplified DNA of mycobacteria tuberculosis strain or clinical probe (microscopically positive sputum samples) with the DNA samples immobilized at nitrocellulose strip. Definition of resistance to rifampin with the use of the HainMTBDR plus test system is carried out by means of detection of the most significant mutations in rpoB gene. The chain of the probes is complementary to the section of wild rpoB gene, coding β-subunit of RNA polymerase of M. tuberculosis, which is the target for the rifampin action. The chain of the probes is complementary to known mutations in the same section leading to resistance of M. tuberculosis to rifampin. To define high level of resistance to isoniazid katG gene is investigated, which codes catalase-peroxydase; to define low level of resistance the zone of promotor in inhA gene is investigated. Presence or absence of mutations or wild type sections is detected by coloring the corresponding strip sections, and basing on it M. tuberculosis strain is considered to be sensitive or resistant to antibiotics. This method may be carried out both directly at the sputum sample of the person discharging bacteria and at the isolated M. tuberculosis culture grown in solid or liquid medium. Diagnostic sensitivity of this method is 96 and 97% respectively, and diagnostic specificity is 90.7 and 83.3% respectively. The time period from receiving the sample to obtaining the results is 1-2 days. As the conduction of this analysis is technically more complicated and the test itself is more sensitive to contamination of the sample in comparison to Xpert MTB/RIF, this analysis is acceptable to be carried out only in laboratory conditions [35].
Conclusion
The review of the literature has shown that tuberculosis as a socially conditioned disease remains a serious problem in Kazakhstan and worldwide in general, currently taking the first position among the infectious diseases causing mortality. One of the main reasons of poor effectiveness of treatment and heavy mortality caused by tuberculosis is prevalence of multiple resistance of tuberculosis mycobacteria to antituberculotics.
Immunological and molecular genetic methods of tuberculosis diagnostics compared with traditional methods are more sensitive and specific and allow detecting mycobacteria tuberculosis in short time in bio-substrates and their drug-resistance which reduces the time of patients’ abacillation, increases the effectiveness of treatment, prevents prevalence of drug-resistant strains of mycobacteria tuberculosis, and also should allow decreasing the level of tuberculosis morbidity in general as well as Multiple/Extensive Drug-Resistant tuberculosis in particular.
References
- Dye C, Scheele S, Dolin P,et al. Consensus statement: Global burden of tuberculosis: estimated incidence, prevalence and mortality by country. WHO Global Surveillance and Monitoring Project. Jama-J.Am. Med. Assoc282 (7), 677-686 (1999).
- Multidrug and extensively drug-resistant TB M /XDR-TB: 2010 global report on surveillance and response. Geneva, Switzerland: World Health Organization (2010).
- Guidelines for the treatment of tuberculosis with multidrug resistance. Partners in Health. Switzerland, Geneva: World Health Organization (2003).
- Guidelines for the programmatic management of drug-resistant tuberculosis. Switzerland, Geneva: World Health Organization (2007).
- Statistical Review of tuberculosis in the Republic of Kazakhstan. Almaty: Nauka (2013).
- Francis JC. Drug-resistant tuberculosis: a survival guide for clinicians. San Francisco: National Tuberculosis Center and California Department of Health Services (2004).
- Korovkin V, Laptev A. The molecular basis of drug resistance in Mycobacterium tuberculosis. Pulmonology phthisiology: Selected lectures and review articles. 131(3),227-243 (2006).
- Ilyin AV. TB drugs and drug resistance. Reports of the National Academy of Sciences of the Republic of Kazakhstan. 302,116-134 (2015).
- Caminero JA. Multidrug-resistant tuberculosis: epidemiology, risk factors and case finding. Int. J. Tuberc. Lung. Dis14 (4), 382-390 (2010).
- Chiang CY, Centis R, Migliori GB. Drag-resistant tuberculosis: bpast, present, future. Respirology.15(3),413-432 (2010).
- Global Tuderculosis Control actuators: surveillance, planning, financing: WHO report 2010. Geneva, Switzerland: World Health Organization (2010).
- Shevchenko OS. Multidrug-resistant tuberculosis: Characteristic resistance profiles isolates M. Tuberculosis. Ekologichnaikilinchnaimunologiya that immunoreabilitatsiya. 2(116), 54-58 (2013).
- Urazova OI. Molecular-genetic factors of pulmonary tuberculosis. Bulletin of the Siberian Medicine5,5-13 (2010).
- Guidelines for the programmatic management of drug-resistant tuberculosis: emergency update 2008. WHO / HTM / TB / 2008.402. Geneva, Switzerland: World Health Organization (2008).
- Guide PIH MDR-TB health management. Boston, Massachusetts: Partners in Health (2003).
- Guidelines for the management of cases of multidrug-resistant and extensively drug in the Republic of Kazakhstan. Almaty, Kazakhstan: Guidelines (2014).
- Zhang Y, Yew WW. Mechanisms of drug resistance in Mycobacterium tuberculosis.Int. J. Tuberc. Lung. Dis13(11),1320-1330 (2009).
- Mishin VY, Chukanov VI, Vasiliev IA. The effectiveness of the treatment of pulmonary tuberculosis caused by mycobacteria multidrug-resistant. Int. J. Tuberc. Lung. Dis2,18-22 (2011).
- Yoshida S, Suzuki K, Iwamoto T, et al.Comparison of rifabutin susceptibility and rpoB mutations in multi-drug-resistant Mycobacterium tuberculosis strains by DNA sequencing and the line probe assay.JInfect.Chemother360-363 (2010).
- Ibraeva AR, Akhmetov AZ, Kozhamkulov YA, et al. Genetic analysis of drug resistance in clinical isolates M. Tuberculosis from different regions of Kazakhstan on the basis of DNA - sequencing.Med. Academic. J 4,84-86 (2012).
- Martin A, Fissette K, Varaine F, et al.Thin layer agar compared to BACTEC MGIT 960 for early detection of Mycobacterium tuberculosis. J.Microbiol. Methods78(1),107-108 (2009).
- Toit K, Mitchell S, Balabanova Y, et al.The Colour Test for drug susceptibility testing of Mycobacterium tuberculosis strains. Int. J. Tuberc. Lung. Dis16(8),1113-1118 (2012).
- Litvinov VI, Frost AM. Laboratory diagnosis of TB. Moscov: MNPTSBT (2001).
- Irtuganova OA. Rapid diagnosis of tuberculosis culture using automated systems VASTES MGIT 960 and MB. Probl. tubes1, 58-62 (2002).
- Balabanova YM. The use of an automated system VASTES MGIT 960 in the diagnosis of drug resistance to the drugs in the reserve Samara. Tuberculosis and Lung Disease9,63-70 (2009).
- Bykdarova KR. The automated system of rapid culture diagnostics of tuberculosis. Proceedings of the VII Congress of Russian TB doctors. 28 (2003).
- Irtuganova OA. Determination of the sensitivity of Mycobacterium tuberculosis to pyrazinamide on bacterial analyzer VASTES 960. Probl. tubes7, 40-42 (2003).
- Augustynowicz-Kopeć E, Jaworski A, Zwolska Z. Evaluation of Bactec MGIT 960 fluorescent method in diagnosis of tuberculosis. Pneumonol.Alergol. Pol70 (9-10), 450-457 (2002).
- Chien HP, Yu MC, Wu MH, et al.Comparison of the BACTEC MGIT 960 with Lowenstein-Jensen medium for recovery of mycobacteria from clinical specimens. Int. J. Tuberc. Lung. Dis4(9), 866-870(2000)
- Lee JJ, Suo J, Lin CB, et al.Comparative evaluation of the BACTEC MGIT 960 system with solid medium for isolation of mycobacteria. Int. J. Tuberc. Lung. Dis2003; 7(6), 569-574.
- Malakhov VN. The quality of bacteriological identification and drug susceptibility testing of Mycobacterium tuberculosis members of the federal system of external quality assessment of clinical laboratory tests in 2002–2003. Problems. tubes4, 6 –10 (2005)
- Frost AM. Laboratory diagnosis of tuberculosis: reality and prospects. Tuberculosis today - problems and prospects. Moscov: NFG (2000).
- Kondratyuk NV. Porivnyalna characteristic medikamentoznoichutlivostishtamiv Mycobacterium tuberculosis. Mikrobiol. Well68(4), 54-59 (2006)
- A comprehensive plan to fight tuberculosis in the Republic of Kazakhstan for 2014-2020. Resolution of the Government dated 09.24.2013.
- Tolemisova AM, Balmahaeva RM. On innovation in the laboratory diagnosis of tuberculosis in the Republic of Kazakhstan. Herald KazNMU. 5(2), 54-58 (2013).
- Boehme C, Nabeta P, Hillemann D, et al. Boehme Rapid Molecular Detection of Tuberculosis and Rifampin Resistance. N. Engl. J. Med363, 1005-1015 (2010)
- Starshinova AA, Pavlov MV, Dovgaluk IF, et al.Immunological and molecular genetic methods of diagnosis of tuberculosis. - Innovative technologies in tuberculosis and pulmonology. Scientific session FGBU. St. Petersburg Research Institute of Phthisiopulmonology. 26 (2013).
- Rusakova LI. Detection and diagnosis of tuberculosis at the present etape. Moscow: Moscow Central Research Institute of Tuberculosis RAMS (2012).
- Rapid implementation of the diagnostic test Hpert MTB/RIF. Technical and operational recommendations. Questions of practical primeneniya. Switzerland, Geneva: World Health Organization (2011).
- Reshetnikov SS, Gladkov SE, Officers VI. Serological diagnosis of tuberculosis: a new test system forserodiagnosis of tuberculosis.
- Chernousova LN. Modern technology for microbiological diagnosis of drug-resistant TB CARE tuberkuleza. Presentation of the project II. Moscov: FGBU Central Tuberculosis Research Institute of Medical Sciences (2013).